Abstract
Fluid shifts are commonplace in chronic hemodialysis patients during the intra- and interdialytic periods. In this study, we evaluated fluid shifts of body compartments using both bioimpedance spectroscopy and blood volume monitoring from the start to the end of hemodialysis. 24 stable hemodialysis patients were included on the study. Relative change of blood volume was progressively reduced from the start to the end of hemodialysis (1 hr, -7.22±3.23%; 2 hr, -9.78±4.69%; 3 hr, -12.88±5.65%; 4 hr, -15.41±6.54%, respectively). Mean % reduction of intracellular fluid was not significantly different to that of extracellular fluid at the end of hemodialysis (Δ ICF, -6.58±5.34% vs. Δ ECF, -7.07±5.12%). Mean % fluid reduction of arms, legs and trunk was -11.98±6.76%, -6.43±4.37% and -7.47±4.56%, respectively at the end of hemodialysis. There were 3 characteristic patterns in blood-volume change. Similar amounts of fluid were removed from the extracellular and intracellular compartments during hemodialysis, with the arms showing the greatest loss in terms of body segments. The pattern of blood volume change measured by blood volume monitoring may be useful for more accurate determination of dry-weight and for correcting volume status in hemodialysis patients.
Body fluid shifts are commonplace in chronic hemodialysis (HD) patients during the intra- and interdialytic periods, and are associated with dialysis-related complications (1). A great challenge for physicians caring for HD patients is accurately assessing volume status. Not surprisingly, clinical determination of dry weight results in substantial error (2). There are several methods for assessing balance and shift of body fluid in HD patients, such as those involving the biochemical markers (ex. cyclic guanosine monophosphate [cGMP], atrial natriuretic peptide [ANP], brain natriuretic peptide [BNP]), inferior vena cava (IVC) diameter, bioimpedance analysis (BIA) and blood volume monitoring (BVM) (2, 3). Biochemical markers of volume overload are fraught with excessive variability and poor correlation with volume status (4, 5). Another limitation of using these markers is the inability to detect volume depletion, since there are no differences in values between normovolemia and hypovolemia. IVC ultrasound is effective, but has several limitations (6-9).
BIA, a simple non-invasive method of assessing body composition has been used to determine the compartmental distribution of body fluid including intracelluar fluid (ICF), extracellular fluid (ECF) and total body water (TBW) (10-12). However, BIA can not differentiate the amounts and changes of the intravascular volume from those of ECF.
BVM is helpful in estimating the relative changes of the intravascular volume whereas BVM can not identify the absolute changes of the intravascular volume and other fluid compartment during HD (2). That can measure the blood volume only in the ratio of relative volume to the predialysis blood volume (14). For this reason, we think the combination method using BIA and BVM is superior to each of the methods alone in assessing the changes and shifts of the fluid compartment during HD.
Else, two recent studies (15, 16) showed contradictory results in assessing fluid changes of body segments during hemodialysis. One study (15) showed fluid reduction of legs was the greatest whereas another study (16) reported fluid removal of trunk was higher than extremity during hemodialysis.
So, in this study, we evaluated fluid shifts of body compartments using both BIA and BVM from the start to the end of hemodialysis.
Twenty four stable HD patients with fixed dry weight (14 men and 10 women; 10 diabetic and 14 non-diabetic) at Dr. Kang's Dialysis Center were participated in this study. Patients within 6 months of starting dialysis therapy, clinical signs of overhydration (predialysis mean arterial pressure >106 mmHg, peripheral edema, pulmonary edema on chest radiograph), hemodynamically unstable subjects (those with cardiac failure and frequent hypotension during hemodialysis), infection, hemiplegia were excluded as were amputees and those aged <18 yr. The studied patients have been on HD therapy for a mean of 64 months (range 7-480 month) and had a mean age of 57 yr (32-87). Some of the patients' characteristics are given in Table 1.
All patients underwent low-flux HD 3 times weekly with bicarbonate buffer for 4 hr, 1.0- to 1.4-m2 hollow fiber polysulfone membranes, blood flow rates of 250-280 mL/min and dialysate flow rates of 500 mL/min, using the Fresenius 4008H machine (Germany) with a built-in ultrasonic blood volume monitor. Ultrafiltration volume ranged from 270 to 3,940 mL, and treatment time was 4 hr. Dialysis fluid contained sodium, 138 mEq/L; potassium, 2 mEq/L; calcium, 2.5 mEq/L; magnesium, 1.0 mEq/L; chloride, 108.5 mEq/L; bicarbonate, 35 mEq/L; and glucose, 99.1 mg/dL, with the temperature maintained at 36℃. Intradialytic hypotension was defined as systolic blood pressure <90 mmHg or systolic blood pressure <100 mmHg with symptoms (nausea, vomiting, sweating, dizziness, and yawning).
A multi-frequency BIA analyzer (Inbody BS1®, Biospace Co. Ltd, Seoul, Korea) was used to measure resistance or impedance at 6 frequencies ranging between 1 kHz and 1 MHz. Eight tactile electrodes were in contact with surfaces of both thumb, palm, front sole, and rear sole. This analyzer is modeling body to 5 cylinders (right arm, left arm, trunk, right leg and left leg). Segmental analysis by Inbody BS1 can not estimate ICF and ECF separately. After it measures a resistance or impedance at frequencies ranging between 1 kHz and 1 MHz from each side, values of resistance or impedance were calculated at all frequencies as follows (17).
Then, these data was exchanged to body fluid amounts by means of BIA software. All patients were maintained in the supine position. The measurements were repeated three times and the average value was used for the data analysis. The BIA measurements were taken immediately before HD and each hour during HD session.
BVM was performed using a real-time online ultrasonic blood volume monitor (Fresenius BVM, Germany). This instrument measures the velocity of sound across flowing blood by using a cuvette designed for this purpose in the extracorporeal circuit. The variability of the velocity of sound in this system depends on changes in the density of total protein content (sum of plasma proteins and hemoglobin). Relative blood volume at any given time may be determined from changes in protein concentration relative to the initial starting value. A high precision temperature measurement compensates for the dependence of sound velocity on blood temperature. The method has been validated as a precise and reliable measurement of relative blood volume and has a very low noise signal ratio (<0.2%) and a sampling rate as low as 3 sec. The technique has been compared against standard reference methods involving serial measurements of hemoglobin and microcentrifuge hematocrit. The measurements were repeated three times and the average value was used for the data analysis.
We expressed clinical data as mean±standard deviation. Statistical tests used were repeated ANOVA, t-test and Kruskall-Wallis test for differences between means where appropriate. We converted the data of blood volume monitoring to coordinates value (x, y) after setting up time to x axis, relative blood volume to y axis with Microsoft Excel 2000 program at intervals of 5 min. Statistics and making graphs was done with Microsoft Excel 2000 and SPSS package version for Windows (SPSS Inc., Chicago, IL, U.S.A.).
Eighty four sets of data were obtained from 24 patients. Relative change of blood volume was progressively reduced from the start to the end of HD (1 hr, -7.22±3.23%; 2 hr, -9.78±4.69%; 3 hr, -12.88±5.65%; 4 hr, -15.41±6.54%, respectively) (Fig. 1).
Fluid was removed from both extracellular and intracellular compartments during HD. ECF was predominantly reduced compared to ICF until 3 hr of HD (ΔECF, -11.08±20.48% vs. ΔICF, -3.32±4.05%). After 3 hr of HD session, relative reduction of ICF became steep. Mean % reduction of ICF was not significantly different to that of ECF at the end of HD (ΔICF, -5.69±6.15% vs. ΔECF, -11.9±20.03%, p value=0.064) (Fig. 1).
The fluid of arm, leg and trunk was significantly and progressively decreased from the start to the end of HD. % fluid reduction of arms, legs and trunk was -13.1±13.97%, -7.26±14.36% and -8.55±13.64%, respectively at the end of HD. The fluid reduction of arms was the greatest but, there was no statistical defferences (p value=0.086) (Fig. 2).
There were 3 characteristic patterns in blood-volume change (Fig. 3). Continuous and linear reduction, curvilinear, early reduction and restoration of blood volume during HD is classified to type 1, 2, 3, respectively. The patients of type 3 have higher ECF/TBW ratio and ECF/UF at the end of HD session compared to those of type 1, 2 (0.42±0.01 vs. 0.36±0.03, 0.33±0.06; 5.77±0.08 vs. 3.41±0.78, 3.29±1.45, respectively) (Table 2).
Main findings of the present study were: First, that fluid was similarly removed from both extracellular and intracellular compartments at the end of HD and the % reduction of segmental body fluid was arms, trunk and legs in order. Second, we could find that there were 3 characteristic patterns in the change of blood volume.
Available previous reports (9, 10) using BIA measurement alone suggest that fluid is removed from both extracellular and intracellular compartments during dialysis, with a predominance of ECF. Our data using BIA and BVM showed that ECF was predominantly reduced compared to ICF until 3 hr of HD. After 3 hr of HD session, reduction curve of ICF became steep. And then, mean % reduction of ICF was not significantly different to that of ECF at the end of HD. These results may suggest that fluid reduction during HD begins in extracellular compartment, initially. After then, significant fluid movement from intracellular to extracellular compartment is followed at the last quarter of HD. Despite significant movement of ICF into ECF, blood volume was continuously reduced to the end of HD. This means that transferred ICF may be remained in interstitial fluid (ISF) in HD patients having clinically euvolemic status. According to the above finding, there is a possibility that movement of ISF to vascular space may start after session of HD in patients who do not experience frequent intradialytic hypotension and have volume overloading.
Whether the fluid is removed disproportionately from the peripheral (arms, legs) or central (trunk) segments has been assessed in two studies (15, 16). In the study of Shulman et al. (15), BIA measurements after a standard 2 kg UF over the first 75 min of dialysis indicated that more than 70% of plasma refilling during HD comes from leg ECF, not central ECF. Another study of Chanchairujira and Mehta (16) reached conclusions that were at odds with the above. This study found that approximately 60% of the ECF change during HD occurred from the trunk rather than the extremities. It is possible to reconcile that part of differences may be attributed to the timing when the bioimpedance measurements were made: Shulman et al. performed the measurements 75 min into dialysis, while Chanchairujira and Mehta obtained them 20-30 min after dialysis. The longer duration and greater amount of UF in the Chanchairujira and Mehta study may also have played a role. Therefore, we suggested that the relative fluid reduction of the arms is the largest is due to the differences of the time interval of measuring BIA. To overcome this fault, we conducted this study that both measurements of BIA and BVM were taken immediately from the start to the end of HD.
The percentage of segmental body fluid to reduced TBW was trunk, legs, and arms in order. This contradictory result is due to the absolute value of body fluid of trunk being the largest.
Our results showed that the fluid of arm, leg and trunk was significantly and progressively decreased from the start to the end of HD. Relative % fluid reduction of extremities was higher than that of trunk through-out HD sessions. Surprisingly, relative % fluid reduction of arms was the greatest according to the our data. When TBW and ECF measurements using bioimpedance were compared to tracer dilution techniques using deuterium oxide and sodium bromide, there was poor agreement between the two methods of measurements (16). According to the Chanchairujira and Mehta's study, while both whole body and segmental bioimpedance measurements can be used to track relative changes in TBW and ECF in HD patients, they are both inaccurate in quantifying absolute ECF volume. Thus, isolated measurements of ECF and ICF by bioimpedance are of no value in clinical practice. However, the reproducibility of measurements is adequate, making bioimpedance a reasonable option to track sequential changes in TBW and ECF (13). Our data showed more relative and sequential fluid changes of HD compared to previous results. And the data of previous studies (15, 16) were the change of ECF in body compartments, while that of our results were the change of TBW in body segments.
There were 3 characteristic patterns in continuous blood-volume monitoring in our patients who were regarding as clinically euvolemic patients. We can suggest that the patients of type 1 are predictive of proximity to dry weight and the likelihood of intradialytic hypotension with further weight reduction. Type 2 patients have the most hypotensive events among these three groups. The patients of type 3 have higher ECF/TBW ratio, ECF/UF and lower ultrafiltration volume at the end of HD session compared to those of type 1, 2. Above finding means that the patients of type 3 are in excess of volume status.
One result of previous studies showed that reduction in relative blood volume at the hypotensive group was significantly greater (18). However, different results were obtained in another study. By Andrulli et al., intradialytic changes in relative blood volume during HD cannot predict whether a patient will be normotensive, prone to symptomatic hypotension, or hypertensive (19, 20). Baseline plasma-dialysate sodium gradient, relative blood volume line irregularity, and early relative blood volume reduction during dialysis influenced the relative risk for symptomatic hypotension.
Our data support the partial use of BVM in chronic HD patients as a tool both in preventing intradialytic hypotension and in identifying patients with volume overload who could benefit from intensified ultrafiltration. While BVM is easy to use and interpret, several limitations apply: blood volume has no standardization (no absolute values exist, no normality parameters for changes in blood volume are established), and different pathophysiologic states can affect plasma refilling. Thus, patients need to be monitored frequently and sequentially to optimize results (14). Despite six time measurements of blood volume in type 3 patients (n=2), a potential limitation of the present study is the small and heterogeneous nature of the subject groups. Enrolled patients underwent various times of BIA estimation and BVM measurements. Thus we used eighty four sets of data obtained from 24 patients, altogether. Therefore, to determine the relationship between blood volume monitoring and accurate volume status in the patient group, future studies will ideally have larger and more homogeneous subject groups compared to the present study.
In conclusions, the changes of body fluid at the end of HD was similarly removed from both extracellular and intracellular compartments and the % reduction of arms was the greatest in chronic stable hemodialysis patients. The pattern of blood-volume change measured by BVM be useful for determining more accurate dry-weight and correcting volume status in patients with HD.
Figures and Tables
Fig. 1
Time course differences of blood volume, ICF, ECF. Relative change of blood volume is significantly reduced from the start to the end of hemodialysis (1 hr, -7.22±3.23%; 2 hr, -9.78±4.69%; 3 hr, -12.88±5.65%; 4 hr, -15.41±6.54%, respectively). Extracellualr fluid is predominantly reduced compared to intracellular fluid until 3 hr of hemodialysis (ΔECF, -6.37±5.88% vs. ΔICF, -3.34±2.83%,). After 3 hr of hemodialysis session, reduction of intracellular fluid becomes steep. Mean % reduction of ICF is equal to that of ECF at the end of hemodialysis (ΔICF, -6.58±5.34% vs. ΔECF, -7.07±5.12%).
ICF, intracellular fluid; ECF, extracellular fluid.
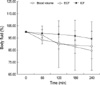
Fig. 2
Time course differences of body compartments. The fluid of arm, leg and trunk is significantly and progressively decreased from the start to the end of hemodialysis. % fluid reduction of arms, legs and trunk is -11.98±6.76%, -6.43±4.37% and -7.47±4.56%, respectively at the end of hemodialysis. The fluid reduction of arms is the greatest.
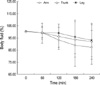
Fig. 3
Three patterns in reduction of blood volume. (A) Type 1 is "continuous and linear reduction type". (B) Type 2 is "curvilinear reduction type". (C) Type 3 is "early reduction and plasma refilling type".

References
2. Jack QJ, Ravindra LM. Assessment of dry weight in hemodialysis: An overview. J Am Soc Nephrol. 1999. 10:392–403.
3. Ishibe S, Peixoto AJ. Methods of assessment of volume status and intercompartmental fluid shifts in hemodialysis patients: implications in clinical practice. Semin Dial. 2004. 17:37–43.

4. Kouw PM, Kooman JP, Cheriex EC, Olthof CG, de Vries PM, Leunissen KM. Assessment of postdialysis dry weight: a comparison of techniques. J Am Soc Nephrol. 1993. 4:98–104.

5. Lauster F, Gerzer R, Weil J, Fulle HJ, Schiffl H. Assessment of dry body weight in hemodialysis patients by the biochemical marker cGMP. Nephrol Dial Transplant. 1990. 5:356–361.
6. Franz M, Pohanka E, Tribl B, Woloszczuk W, Horl WH. Living on chronic hemodialysis between dryness and fluid overload. Kidney Int Suppl. 1997. 59:Suppl 59. S39–S42.
7. Moreno FL, Hagan AD, Holmen JR, Pryor TA, Strickland RD, Castle CH. Evaluation of size and dynamics of the inferior vena cava as an index of right-sided cardiac function. Am J Cardiol. 1984. 53:579–585.

8. Cheriex EC, Leunissen KM, Janssen JH, Mooy JM, van Hooff JP. Echography of the inferior vena cava is a simple and reliable tool for estimation of "dry weight" in hemodialysis patients. Nephrol Dial Transplant. 1989. 4:563–568.
9. Katzarski KS, Nisell J, Randmaa I, Danielsson A, Freyschuss U, Bergstrom J. A critical evaluation of ultrasound measurement of inferior vena cava diameter in assessing dry weight in normotensive and hypertensive hemodialysis patients. Am J Kidney Dis. 1997. 30:459–465.

10. Fisch BJ, Spiegel DM. Assessment of excess fluid distribution in chronic hemodialysis patients using bioimpedance spectroscopy. Kidney Int. 1996. 49:1105–1109.

11. Zhu F, Schneditz D, Levin NW. Sum of segmental bioimpedance analysis during ultrafiltration and hemodialysis reduces sensitivity to changes in body position. Kidney Int. 1999. 56:692–699.

12. Zhu F, Schneditz D, Wang E, Martin K, Morris AT, Levin HW. Validation of changes in extracellular volume measured during hemodialysis using a segmental bioimpedance technique. ASAIO J. 1998. 44:M541–M545.

13. Cox-Reijven PL, Kooman JP, Soeters PB, Van der Sande FM, Leunissen KM. Role of bioimpedance spectroscopy in assessment of body water compartments in hemodialysis patients. Am J Kidney Dis. 2001. 38:832–838.

14. Diskin CJ, Stokes TJ, Dansby LM, Carter TB, Radcliff L, Thomas SG. Towards an understanding of oedema. BMJ. 1999. 318:1610–1613.

15. Shulman T, Heidenheim AP, Kianfar C, Shulman SM, Lindsay RM. Preserving central blood volume: changes in body fluid compartments during hemodialysis. ASAIO J. 2001. 47:615–618.

16. Chanchairujira T, Mehta RL. Assessing fluid change in hemodialysis: whole body versus sum of segmental bioimpedance spectroscopy. Kidney Int. 2001. 60:2337–2342.

17. Bedogni G, Malavolti M, Severi S, Mussi C, Fantuzzi AL, Battistini N. Accuracy of an eight point tactile-electrode impedance method in the assessment of total body water. Eur J Clin Nutr. 2002. 56:1143–1148.
18. Zucchelli P, Santoro A. Dialysis-induced hypotension: A fresh look at pathophysiology. Blood Purif. 1993. 11:85–98.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download