Abstract
The aim of the present study was to evaluate the pattern of recurrence after complete resection of pathological stage I, II non-small cell lung cancer, especially according to the cell type. We reviewed the clinical records of 525 patients operated on for pathologic stage I and II lung cancer. The histologic type was found to be squamous in 253 and non-squamous in 229 patients. Median follow-up period was 40 months. Recurrences were identified in 173 (36%) of 482 enrolled patients; distant metastasis in 70%, distant and local recurrence in 11%, and local recurrence in 19%. Distant metastasis was more common in non-squamous than in squamous cell carcinoma (p=0.044). Brain metastasis was more frequently identified in non-squamous mthan in squamous cell carcinoma (24.2% vs. 7.3%. p=0.005). Multivariate analyses showed that cell type is the significant risk factor for recurrence-free survival in stage I and stage II non-small cell lung cancer. Recurrence-free survival curves showed that non-squamous cell carcinoma had similar risks during early periods of follow-up and more risks after 2 yr from the operation compared to squamous cell carcinoma. Pathological stage and histologic type significantly influence recurrence-free survival.
Lung cancer became the leading cause of cancer death in the world; however, even the early stage does not have a satisfactory long-term survival rate after complete resection. During follow-up after surgical resection in our center, we noted a possible difference in recurrence patterns between squamous cell carcinoma and non-squamous cell carcinoma. After resection of non-small cell lung cancer, histologic type is noted as a prognostic factor in some reports, but not in others. Recently, some studies have reported on the prognostic significance of several biological factors in the early stage of non-small cell lung cancer (1, 2). Histologic characterization offers a starting point for the analysis of biological prognostic factors. The aim of the present study was to evaluate the pattern of recurrence after curative resection of pathological stage I and II non-small cell lung cancers, with special attention to the cell type.
We reviewed the clinical records of 525 patients operated on for pathologic stage I and II lung cancer between January 1995 and December 2000. Four hundred and forty-seven lobectomies, 75 pneumonectomies, and 3 wedge resections were performed. Eighteen patients with in-hospital mortality, including operative mortality, were excluded. Another 25 patients were also excluded because they had carcinoid tumor, or mucoepidermoid carcinoma. Clinicopathologic characteristics of the remaining 482 patients are described in Table 1. We obtained follow-up data by chest CT at 3 month intervals for the first 2 yr and at 6 month intervals after 2 yr. Recurrence was evaluated with our hospital records and information from other hospitals. Recurrence pattern was classified into two categories: locoregional and distant metastasis. Locoregional recurrence included cancer development to supraclavicular nodes, mediastinal nodes, pleural effusion or seeding, bronchial stump and ipsilateral lung. Distant metastasis categorized metastasis to contralateral lung, brain, bone, liver, adrenal and other organs. Simultaneous locoregional and distant metastasis was considered distant metastasis group.
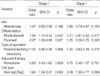
Sex, pathological stage, tumor differentiation (well, moderate, poor), extent of resection (wedge resection, lobectomy including sleeve resection, and pneumonectomy), and histologic type (squamous cell carcinoma, nonsquamous carcinoma including adenocarcinoma and large cell carcinoma) were evaluated by univariate and multivariate analysis. Survival rates were calculated by the actuarial method and compared by the log-rank test with SPSS software.
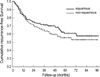
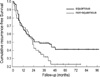
Median follow-up period was 40 months (2-99 months) after operation. Recurrences were identified in 173 (36%) of 482 patients during follow-up; distant metastasis 70%, simultaneous distant metastasis and local recurrence 11%, and local recurrence 19%. Distant metastasis was more common in non-squamous cell carcinoma (adenocarcinoma and large cell carcinoma) than in squamous cell carcinoma (p=0.044). Brain metastasis was found more frequently in non-squamous cell carcinoma than in squamous carcinoma (24.2% vs. 7.3%. p=0.005). There were no significant differences between local and distant recurrences, according to either stage I or stage II (p=0.382). Overall actuarial 5-yr survival rates for stage I and stage II were 74% and 42% (p<0.001), respectively. Overall 5-yr recurrence-free survival rates were also statistically different (stage I, 57% and stage II, 36%, p<0.001). Univariate analyses of recurrence-free survival in stage I and stage II are described in Table 2. Multivariate analyses by the Cox regression test showed that cell type is the significant risk factor for recurrence-free survival in both stage I and stage II non-small cell lung cancer (Table 3). Recurrence-free survival curves showed similar risks during early periods of follow-up for non-squamous cell carcinoma, and more risks after 2 yr from the operation when compared to squamous cell carcinoma (Fig. 1, 2).
We were fortunate to obtain nearly complete follow-up of patients after surgical resection for local non-small cell lung cancer. Our study was initiated based on our initial observations that recurrence patterns appeared to be different, according to the histology at outpatient follow-up. According to previous reports, the histologic type of the tumor is one of the determinants of survival in patients with resected local non-small cell lung cancer. In the Lung Cancer Study Group, cancer recurrences and cancer-related death were more frequent and recurrence rates were higher in patients with non-squamous histology (3). However, Martini et al. reported that there was no difference in overall survival between squamous and non-squamous cancers (4). Ramacciato et al. also reported that histologic type did not play a statistically significant role in the total incidence of recurrence (5). Rena et al. reported better 5-yr survival rates for adenocarcinoma than for squamous cell carcinoma (6). Our data demonstrated similar results to those of the Lung Cancer Study Group. Recent data reported by Okada et al. demonstrated that advanced stage, high involvement of lymph nodes, male gender, and non-squamous cancer were independent, unfavorable prognostic factors in completely-resected lung cancer patients (7). We confirmed that the poor prognosis of non-squamous cell carcinoma becomes evident after 2 yr. This finding could be explained by the fact that distant metastases were more common in non-squamous cell tumors than in the squamous type.
Our data also demonstrated that brain metastases were more common in non-squamous carcinoma than in squamous cell carcinoma, and some reports and preceding report by our institute showed corresponding results to ours (8-10). Whether the patients benefit from the therapy for single brain metastases remains another issue for study.
Figures and Tables
References
1. Cagini L, Monacelli M, Giustozzi G, Moggi L, Bellezza G, Sidoni A, Bucciarelli E, Darwish S, Ludovini V, Pistola L, Gregorc V, Tonato M. Biological prognostic factors for early stage completely resected non-small cell lung cancer. J Surg Oncol. 2000. 74:53–60.

2. D'Amico TA, Aloia TA, Moore MB, Herndon JE 2nd, Brooks KR, Lau CL, Harpole DH Jr. Molecular biologic substaging of stage I lung cancer according to gender and histology. Ann Thorac Surg. 2000. 69:882–886.
3. Thomas PA Jr, Rubinstein L. Malignant disease appearing late after operation for T1 N0 non-small cell lung cancer. The Lung Cancer Study Group. J Thorac Cardiovasc Surg. 1993. 106:1053–1058.
4. Martini N, Bains MS, Burt ME, Zakowski MF, McCormack P, Rusch VW, Ginsberg RJ. Incidence of local recurrence and second primary tumors in resected stage I lung cancer. J Thorac Cardiovasc Surg. 1995. 109:120–129.

5. Ramacciato G, Paolini A, Volpino P, Aurello P, Balesh AM, D'Andrea N, Del Grande E, Passaro U, Tosato F, Fegiz G. Modality of failure following resection of stage I and stage II non-small cell lung cancer. Int Surg. 1995. 80:156–161.
6. Rena O, Oliaro A, Cavallo A, Filosso PL, Donati G, Di Marzio P, Maggi G, Ruffini E. Stage I non-small cell lung carcinoma: really an early stage? Eur J Cardiothorac Surg. 2002. 21:514–519.

7. Okada M, Nishio W, Sakamoto T, Harada H, Uchino K, Tsubota N. Long-term survival and prognostic factors of five-year survivors with complete resection of non-small cell lung carcinoma. J Thorac Cardiovasc Surg. 2003. 126:558–562.

8. Mussi A, Pistolesi M, Lucchi M, Janni A, Chella A, Parenti G, Rossi G, Angeletti CA. Resection of single brain metastasis in non-small-cell lung cancer: prognostic factors. J Thorac Cardiovasc Surg. 1996. 112:146–153.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download