Abstract
A duodenal duplication cyst is an uncommon congenital anomaly that is usually encountered during infancy or in early childhood. Duodenal duplication cysts generally appear on the first or second portion of the duodenum and may cause duodenal obstruction, hemorrhage or pancreatitis. Here, we report a case of a duodenal duplication cyst on the second and third portion of the duodenum in an old aged man with obstructive jaundice and acute pancreatitis, which was treated successfully by a surgical excision.
Duodenal duplication cyst (DDC) is a rare congenital anomaly (1-13), which can appear during the neonatal period or later in life depending on the degree of the gastric outlet obstruction. About thirty percent of patients diagnosed with duplication cysts are older than twelve years of age, and the oldest patient with DDCs reported was 73 yr old (1). These lesions often present a diagnostic and therapeutic challenge to surgeons. Duplications of the duodenum may be either cystic or tubular and are composed of a muscular wall with a gastrointestinal epithelial lining. Duplication cysts may be found at any level from the mouth to the anus and are usually attached intimately to some portions of the gastrointestinal tract. Only 4-12% of these duplications are located in the duodenum. Here, we describe the first Korean case of a DDC associated with bowel obstruction, obstructive jaundice and acute pancreatitis in the later period of life.
A 65-yr-old man was referred to our hospital complaining of pain in the right upper quadrant and vomiting for previous 3 days. His past medical history was unremarkable except for a spinal operation performed due to a falling-down injury 10 yr ago. A physical examination demonstrated tenderness and a soft palpable mass on the right upper quadrant of the abdomen. The laboratory examinations showed a hemoglobin level of 15.3 g/dL (normal range, 14 to 18), a white blood cell count of 12,590/µL (normal range, 4,000 to 10,000), and a platelet count of 254,000/µL (normal range, 140,000 to 400,000). The liver function tests showed a total serum bilirubin level of 3.3 mg/dL (normal range, 0.1 to 1.2), a direct bilirubin level of 2.1 mg/dL (normal range, 0.1 to 0.4), alkaline phosphatase level of 323 IU/L (normal range, 20 to 90), a gamma glutamyl transpeptidase level of 371 IU/L (normal range, 0 to 50), an aspartate aminotransferase level of 267 IU/L (normal range, 10 to 35); alanine aminotransferase, 228 IU/L (normal range, 0 to 40); amylase, 972 IU/L (normal range, 50 to 160) and a lipase level of 2,767 IU/L (normal range, 0 to 200). A duodenoscopy revealed a huge extrinsic mass with an intact mucosa causing almost complete luminal obstruction in the second portion of the duodenum. On palpation with a biopsy forcep, the mass was found to be soft and easily compressible (Fig. 1). A computerized tomography scan showed a 12×6 cm sized elliptic cystic lesion with a distinct wall at the second-to-third portion of the duodenum. The lesion occupied the intramural portion of the duodenal wall. These findings above were consistent with a DDC (Fig. 2). The intrahepatic duct and common bile duct were dilated, and the gallbladder was markedly distended (Fig. 3). A percutaneous transhepatic biliary drainage for the relief of obstructive jaundice was performed one day after admission. pylorus-preserving pancreaticoduodenectomy (modified Whipple's operation) was performed 24 days after supportive treatment. The surgical specimens included the segments of the duodenum and the duplication cyst, the gallbladder and some portions of the pancreas. The duplication cyst was located along the antimesenteric border and was 9 cm in length and 2.8 cm in the inner diameter (Fig. 4). There was no luminal communication between the cyst and the duodenum. The inner surface of the cyst was flat and showed multiple erosions and ulcers. Histologically, the cyst showed denudation of the mucosal layer, which was replaced by granulation tissue, due to the mucosal inflammation, but most parts of the cyst contained a smooth muscle layer (Fig. 5). The post-operative course of the patient was uneventful, and the patient has been doing well for 6 months after surgery without any complication.
Duplication cysts are congenital anomalies that are formed during the embryonic period of the development of the human digestive system. The most common site for a gastrointestinal duplication cyst is the distal ileum followed by the esophagus and duodenum (2). Duplication cysts must adhere to a portion of the gastrointestinal tract, contain a smooth muscle layer in their walls and be lined with an alimentary epithelium. The epithelial lining of the duplication cysts may be that of the adjacent bowel, and ectopic gastric or pancreatic tissue may sometimes be present within (2, 3). Gastric duplications occur along the greater curvature, and intestinal duplication cysts are found on the mesenteric side of the bowel. The cysts may be spherical or tubular, and there may be infrequent communications with the gastrointestinal tract. DDCs are diagnosed more often in children. They are mostly limited to the first or second part of the duodenum usually adjacent to the pancreatic surface sharing a common wall and blood supply with the duodenum. DDCs may be silent for many years before they cause any symptoms including bowel obstruction, pain, distention or gastrointestinal bleeding. Bleeding, ulceration, and perforation may occur in the cysts containing ectopic gastric mucosa (2, 3). The clinical presentation depends on the size and location of the cysts. In our case, the patient was old and had accompanying symptoms of bowel obstruction, obstructive jaundice, and acute pancreatitis. The compression caused by the duplicated segment of the duodenum attributed to the above symptoms. The cyst was in the second and third portions of the duodenum and had an ulceration on the inner side.
The three criteria for the diagnosis of a duplication cyst are the presence of an intimate attachment to the gastrointestinal tract, a smooth muscle coat, and an alimentary mucosal lining (2). Of above three criteria, the presence of a smooth muscle coat is absolutely essential for the diagnosis of a duplication cyst. In our case, although the lining epithelial cells were entirely denuded and replaced by inflamed granulation tissue due to increased intraluminal pressure and inflammation, most of the cyst contained smooth muscle coats with foci of a neural plexus, which supported the diagnosis of a duplication cyst.
The differential diagnosis of DDCs and choledochoceles demands particular attention. The principal distinguishing features between these two conditions are their histological characteristics. DDCs are covered both inside and outside by duodenal mucosa containing a distinct layer of smooth muscles. In contrast, choledochoceles are lined by either a bile duct or gallbladder mucosa and lack a smooth muscle layer (14).
DDCs have been traditionally treated with surgery. The surgical approach should be made in accordance with the relationship between the cyst wall and the biliary and pancreatic drainage systems. The surgical goal is the free drainage of the cyst into the duodenum without damaging the biliary and pancreatic ducts. Occasionally, the close relationship between the DDC and the pancreaticobiliary system makes surgery difficult and risky. In these cases an endoscopic procedure appears to be a reasonable option (4, 5). A total excision of the cyst prevents further hazards including the development of a malignancy that may arise from the residual ectopic gastric mucosa (6). Thus, our case was treated with a pyloruspreserving pancreaticoduodenectomy, which cured the patient.
Figures and Tables
Fig. 1
Duodenoscopic finding. A huge extrinsic mass causing a luminal obstruction in the proximal second portion of the duodenum, with an intact mucosa.
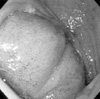
Fig. 2
Computerized tomographic finding. A cystic lesion with a distinct wall in the second-to-third portion of the duodenum (A, B) is shown. The duodenum (closed arrow) is compressed by the cystic lesion and is displaced to the medial side of the lesion (open arrow) (A).
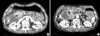
Fig. 3
Computerized tomographic finding. Dilated intrahepatic duct (A) and a common bile duct and markedly distended the gallbladder (B) is shown.

References
1. Browning RW. Duodenal duplications. Rev Surg. 1963. 20:226–229.
2. Gross RE, Holcomb GW Jr, Farber S. Duplications of the alimentary tract. Pediatrics. 1952. 9:449–468.
3. Rubin RB, Saltzman JR, Zawacki JK, Khan A, Swanson R. Duodenal duplication cyst with massive gastrointestinal bleeding. J Clin Gastroenterol. 1995. 21:72–74.
4. Wada S, Higashizawa T, Tamada K, Tomiyama T, Ohashi A, Satoh Y, Sugano K, Nagai H. Endoscopic partial resection of a duodenal duplication cyst. Endoscopy. 2001. 33:808–810.

5. Sezgin O, Altiparmak E, Yilmaz U, Saritas U, Sahin B. Endoscopic management of a duodenal duplication cyst associated with biliary obstruction in an adult. J Clin Gastroenterol. 2001. 32:353–355.

6. Falk GL, Young CJ, Parer J. Adenocarcinoma arising in a duodenal duplication cyst: a case report. Aust N Z J Surg. 1991. 61:551–553.

7. Narlawar RS, Rao JR, Karmarkar SJ, Gupta A, Hira P. Sonographic findings in a duodenal duplication cyst. J Clin Ultrasound. 2002. 30:566–568.

8. Zamir G, Gross E, Shmushkevich A, Bar-Ziv J, Durst AL, Jurim O. Duodenal duplication cyst manifested by duodeno-jejunal intussusception and hyperbilirubinemia. J Pediatr Surg. 1999. 34:1297–1299.

9. Arbell D, Lebenthal A, Blashar A, Shmushkevich A, Gross E. Duplication cyst of the duodenum as an unusual cause of massive gastrointestinal bleeding in an infant. J Pediatr Surg. 2002. 37:E8.

10. Fan ST, Lau WY, Pang SW. Infarction of a duodenal duplication cyst. Am J Gastroenterol. 1985. 80:337–339.
11. Ogura Y, Kawarada Y, Mizumoto R. Duodenal duplication cyst communicating with an accessory pancreatic duct of Santorini. Hepatogastroenterology. 1998. 45:1613–1618.
12. Richer JP, Faure JP, Maillot N, Silvain C, Levillain P, Carretier M. Duodenal duplication cyst communicating with the bile duct with a long common biliary-pancreatic channel. Eur J Surg. 2000. 166:504–507.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download