Abstract
The purpose of this study was to identify the major etiological agents responsible for invasive bacterial infections in immunocompetent Korean children. We retrospectively surveyed invasive bacterial infections in immunocompetent children caused by eight major pediatric bacteria, namely Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, Listeria monocytogenes, and Salmonella species that were diagnosed at 18 university hospitals from 1996 to 2005. A total of 768 cases were identified. S. agalactiae (48.1%) and S. aureus (37.2%) were the most common pathogens in infants younger than 3 months. S. agalactiae was a common cause of meningitis (73.0%), bacteremia without localization (34.0%), and arthritis (50%) in this age group. S. pneumoniae (45.3%) and H. influenzae (20.4%) were common in children aged 3 months to 5 yr. S. pneumoniae was a common cause of meningitis (41.6%), bacteremia without localization (40.0%), and bacteremic pneumonia (74.1%) in this age group. S. aureus (50.6%), Salmonella species (16.9%), and S. pneumoniae (16.3%) were common in older children. A significant decline in H. influenzae infections over the last 10 yr was noted. S. agalactiae, S. pneumoniae, and S. aureus are important pathogens responsible for invasive bacterial infections in Korean children.
Invasive bacterial infection is a major cause of morbidity and mortality in children. The etiology of invasive bacterial infections in immunocompetent children can vary according to study conditions, such as the country of origin, age of patients, level of hygiene, vaccine policy, survey time, and types of diagnostic tests performed.
In the United States, the major etiologic agents associated with invasive bacterial infections during the neonatal period during the 1950s-1960s were Staphylococcus aureus and Escherichia coli; since then, group B streptococcus (also known as Streptococcus agalactiae) and Gram-negative enteric bacteria have become the most common pathogens (1). However, the epidemiology of group B streptococcus has changed over time with the implementation of antenatal antimicrobial prophylaxis for group B streptococcus (2). Recently, changes in the epidemiology of two major pathogens in post-neonatal infants, namely Streptococcus pneumoniae and Hemophilus influenzae type b (Hib), have been observed in countries where the vaccine coverage rates are high among young infants and children (3, 4). The relative incidence of each bacterial pathogen has important implications for vaccine policy and empirical antibiotic treatment. Therefore, it is important to know the distribution of the major etiological agents of invasive bacterial infections in children in the setting of a local community.
In Korea, antenatal antimicrobial prophylaxis for group B streptococcus is not yet implemented as part of routine clinical practice. The vaccination rate for Hib increased gradually from 16% in 2002 to about 50% in 2005 (5, 6) and was estimated to be over 80% in 2008. Although the 7-valent pneumococcal conjugate vaccine was introduced in November 2003, its coverage rate was still very low by 2005 (7).
We conducted a retrospective, multicenter study to analyze the prevalence of the major bacterial etiological agents present in immunocompetent Korean children according to age, clinical features, and time.
The population of infants and children less than 18 years of age is about 10 million in Korea. About 48% of infants and children live in the National Capital Region that includes two metropolitan cities, Seoul and Incheon, and Gyeonggi-do. Another 21% live in regional metropolitan cities, based on the population data from the 2005 Census (8). Out of the 89 university-affiliated hospitals in Korea, 50 hospitals are located in the National Capital Region. Seventeen university-affiliated hospitals participated in this study. These 18 hospitals have a nationwide distribution: 13 hospitals are located in the National Capital Region (St. Paul's Hospital, Kyunghee University Hospital, Seoul National University Children's Hospital, Soonchunhyang University Hospital, Severance Children's Hospital, Ewha Womans University Mokdong Hospital and Ewha Womans University Dongdaemoon Hospital, Kangnam Sacred Heart Hospital, Hanyang University Hospital, Incheon St. Mary's Hospital, Inha University Hospital, Korea University Ansan Hospital, St. Vincent's Hospital), and five hospitals are located in the regional central cities of provinces (Gangwon-do-Wonju Christian Hospital, Chungcheongnam-do-Dankook University Hospital, Jeollabuk-do-Chonbuk National University Hospital, Gwangju/Jeollanam-do-Chonnam National University Hospital and Busan/Gyeongsangnam-do-Pusan National University Hospital).
The survey period was from January 1996 to December 2005. The medical records of children less than 18 yr of age with invasive bacterial infections were reviewed retrospectively at the 18 university hospitals. Cases were selected from databases of hospital discharge records and the microbiology registry of the departments of laboratory medicine. Initially, cases with positive results for the target organisms were selected. Investigators then reviewed the medical records of the cases and determined whether the case should be included in the study based on the case definition of the study protocol. Both community onset and hospital-acquired infections were included. A standard case report form was used to collect case information. Demographic data, underlying illnesses, clinical diagnoses, isolated organisms, site(s) of bacterial isolation, clinical manifestations, laboratory findings, antibiotic susceptibility, and treatment results were collected. The distribution of bacterial pathogens was analyzed according to age, clinical diagnosis, and time.
An 'invasive bacterial infection' was defined as the isolation of a bacterial organism from a normally sterile body fluid, such as blood, cerebrospinal fluid, pleural fluid, pericardial fluid, joint fluid, bone aspirate, or a deep tissue abscess (2). If the same pathogen was found in another sample taken within 30 days after the previous positive sample, or during the same admission period, the episode was considered a single case. Cases with conditions predisposing to invasive bacterial infections, such as congenital or acquired immunodeficiency, steroid or cancer chemotherapy, prematurity, and infections associated with anatomic abnormalities (e.g., cerebrospinal fluid leakage), were excluded (9). Urinary tract infections without bacteremia were excluded because culture results for specimens collected by the bag method, which was used in most cases, are not reliable. In addition, superficial infections such as acute otitis media were not included unless a bacterial organism was isolated simultaneously from other sterile body fluids.
An invasive infection was classified on the basis of consistent clinical findings and isolation of pathogens from the specimens. 'Bacteremia without localizing signs' was defined as cases with no identifiable focus where the bacterial organism was isolated only from blood. A clinical diagnosis with a focal lesion such as 'meningitis', 'pneumonia', 'arthritis', 'osteomyelitis', 'peritonitis', or 'deep tissue abscess' was defined according to the bacterial organism isolated from the corresponding body fluid such as cerebrospinal fluid, pleural fluid, joint fluid, bone aspirate, or abscess, or the bacterial organism isolated only from blood with clinical manifestations compatible with the diagnosis.
Target organisms were limited to eight major pediatric bacterial pathogens, namely S. pneumoniae, S. aureus, H. influenzae, Neisseria meningitidis, S. agalactiae, Streptococcus pyogenes, Listeria monocytogenes, and Salmonella species. These eight organisms were found to be responsible for 90%-95% of invasive bacterial infection other than urinary tract infections among infants and children in Korea older than 3 months of age in previous studies (10, 11).
Clinical specimens were collected and processed by standard methods at each of the participating hospitals. Blood specimens were initially inoculated in brain-heart infusion broth and tetrathionate broth and processed using an automated culture system such as BACTEC or BacT/ALERT. The culture media was subcultured on chocolate agar and blood agar plates when turbidity was evident and, in some hospitals, before discarding after 1 week of incubation. Blood agar and chocolate agar plates were used for the direct plating of cerebral, pleural, or other body fluids. Salmonella isolates were serogrouped using serogroup-specific typing sera.
Final outcomes were evaluated on discharge. The final outcome on discharge was categorized as follows: full recovery, recovery with sequelae, death, or hopeless discharge. Cases classified as 'transfer to another hospital' and 'discharge against medical advice, expected not to die' were considered missing data because the final outcome could not be determined. The case-fatality rate was calculated for each pathogen.
All statistics were calculated using SPSS version 12.0 (SPSS, Chicago, IL, USA). Pearson's chi-square test, Fisher's exact test, or the chi-square test for trends was used to compare the relative frequencies of bacterial organisms and to analyze temporal trends. All tests were two-tailed and differences were considered significant at P < 0.05.
A total of 768 episodes of invasive bacterial infections were identified during the study period. The number of cases in which the causative organism was detected only from the blood was 350. The number of cases in which the organism was detected from sterile body fluids other than blood was 287. Among these, 147 cases were diagnosed as meningitis. The number of cases in which the organism was detected from both blood and other sterile body fluids was 131. The male-female ratio was 1.4:1. Regardless of age and clinical diagnosis, S. aureus was the most frequently isolated organism (238 cases, 31.0%), followed by S. pneumoniae (179 cases, 23.3%), and S. agalactiae (145 cases, 18.9%). Salmonella species and H. influenzae accounted for 78 cases (10.2%) each. There were very few cases of N. meningitidis (16 cases) or L. monocytogenes (5 cases) infections. Of the S. aureus isolates, 25.2% were oxacillin resistant.
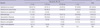
Age groups were stratified as follows: under 3 months, 3 to 23 months, 24 to 59 months, and 5 yr or older. The number of cases was highest in the under-3-months age group, with 285 cases (37%), followed by the 3-23 month age group with 199 cases (26%) and the 5 yr and older age group with 172 cases (22%). Patients under 5 yr of age accounted for 77% of all cases. The age-related distribution of causative bacterial organisms is shown in Table 1. The distribution of bacteria differed by age group, especially at < 3 months and ≥ 5 yr of age. S. agalactiae was most frequently isolated from infants less than 3 months of age and accounted for 48.1% of the cases in this age group, followed by S. aureus, which accounted for 37.2% of cases; these two organisms were responsible for 85.3% of all invasive bacterial infections identified in this age group. When this age group was divided by 1 week, separating neonatal infections into early and late onset infections (12), S. agalactiae accounted for 33.3% (28/84) of the early onset neonatal infections and 54.2% (109/201) of late onset neonatal infections, while S. aureus accounted for 56.0% (47/84) and 29.4% (59/201) of the early and late onset neonatal infections, respectively. Only 20.4% (28/137) of S. agalactiae infections were early neonatal infections.
S. pneumoniae, H. influenzae, and Salmonella species were isolated frequently in infants and children 3 months of age or older. S. pneumoniae was the most common bacterial agent responsible for invasive infections in infants and children aged 3 months to 5 yr, accounting for 45.3% (140/309) of cases. In contrast, S. pneumoniae was the third most common cause of bacterial infection in children older than 5 yr of age (16.3% of cases). H. influenzae was a significant cause of infections in children between 3 months and 5 yr of age and accounted for 21.0% of invasive infections that developed in this age group. H. influenzae infections were rare in children aged 5 yr or older. Salmonella species accounted for 15.2% of invasive infections in children aged 3 months or older. The percentage of S. aureus dropped to 14.2% in children between the ages of 3 months and 5 yr, and then increased sharply to 50.5% in children older than 5 yr.
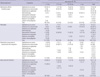
Among the 768 invasive bacterial infections identified, meningitis and bacteremia without localizing signs were the most frequent infections and accounted for 34.5% and 27.6% of all cases, respectively. Pneumonia with bacteremia or empyema accounted for 12.4% of infections. Arthritis and osteomyelitis accounted for 8.5% and 7.7% of infections, respectively. Deep abscess formation and peritonitis accounted for 2.0% and 0.4% of infections, respectively. Other diseases not assigned to one of the above clinical entities accounted for 7.0% of infections. Detailed age-specific distributions of causative organisms according to clinical features are presented in Table 2.
There were age-related differences in the distributions of causative bacterial organisms among patients with bacteremia without localizing signs, meningitis and pneumonia. Among patients with bacteremia without localizing signs, S. aureus was frequently isolated from infants less than 3 months of age and from children 5 yr of age or older. S. agalactiae was identified exclusively in infants less than 3 months old. S. pneumoniae and Salmonella species were consistently isolated from children 3 months of age or older. As for meningitis, most cases that developed in the younger-than-3-months age group were attributed to S. agalactiae (73.0%). However, in children aged between 3 months and 59 months, S. pneumoniae and H. influenzae were responsible for the majority of cases, accounting for 43.9% and 47.4% of infections, respectively. N. meningitidis was a significant cause of infection in the older-than-5-yr age group and was identified in 37.1% (13/35) of cases. Similarly, in cases with pneumonia, S. aureus and S. agalactiae were frequently identified in younger children while S. pneumoniae was more often identified in older children. In contrast, in deep tissue abscesses and bone and joint infections, S. aureus was the predominant organism across all age groups.
The different distributions of organisms according to age group (especially, under 3 months, 3-59 months, and over 5 yr) for most clinical diagnoses are illustrated in Fig. 1.
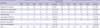
The relative frequency of bacterial organisms was analyzed on a yearly basis (Fig. 2). The study was divided into two periods; the five years until the year 2000 (first period), and the five years after 2000 (second period). The relative frequency of each bacterial organism during the first period was compared to the frequency during the second period (Table 3).
This analysis revealed a significant decline in invasive H. influenzae infections. During the first 5 yr of the study, 20.1% of all invasive bacterial infections were attributed to H. influenzae; however, only 4.5% were due to H. influenzae during the latter five years (P < 0.001). This change was significant from 2001. The decreased frequency of H. influenzae infections was accompanied by a relative increase in S. pneumoniae and S. aureus infections (P = 0.475, P = 0.002). The increase in S. agalactiae infections among infants less than 3 months of age during the study period was not significant (P = 0.130) based on a likelihood ratio for trends test.
Clinical outcome were available for 671 (87%) of the 768 cases. The overall case-fatality rate was 6.4% (43/671) regardless of the type of bacterial organism or clinical diagnosis. When the data were analyzed according to clinical diagnosis, meningitis showed the highest case-fatality rate (11.9%, 28/235), followed by bacteremia without localizing signs (5.6%, 10/180) and pneumonia (4.9%, 4/82). There was a slight but non-significant improvement in clinical outcomes over time. When the case fatality rate was analyzed according to age group, we found that the case fatality rate decreased with increasing age; infants less than 3 months of age showed the highest case-fatality rate (7.9%, 19/240), followed by the 3-23 month group (7.1%, 13/184), 24-59 month group (6.3%, 5/151), and children older than 5 years of age (3.3%, 5/151).
Among the bacterial organisms studied, N. meningitidis was associated with the highest case-fatality rate of 15.4% (2/13); however, the overall number of cases of N. meningitidis infection was relatively small. When bacterial organisms found in 50 or more cases were analyzed, we found that S. pneumoniae had the highest case-fatality rate of 12.4% (20/161) followed by S. agalactiae with a case fatality rate of 10.4% (13/125). S. aureus and Salmonella species had low case fatality rates of 3.0% (6/201) and 1.4% (1/69), respectively. No fatalities associated with H. influenzae infection were identified during the study period. Although not statistically significant, the case-fatality rates due to S. pneumoniae and S. agalactiae infections, which are associated with higher mortality, improved in the latter half of the study period from 16.1% and 14.6% to 9.1% and 4.4%, respectively.
In terms of the frequency of sequelae associated with meningitis cases, H. influenzae had a very high sequelae rate of 31.8% (21/66). Sequelae associated with meningitis caused by the other common infective organisms, namely S. pneumoniae, S. agalactiae, and S. aureus, showed similar trends compared to the case-fatality rates and were 47.8% (22/46), 34.8% (24/69), and 11.1% (1/9), respectively. The most common sequelae were hydrocephalus and paralysis. Long term sequelae such as developmental delay and cognitive impairment were not evaluated because of the retrospective nature of the study design.
The purpose of this study was to investigate the bacterial etiology of invasive infections in a pediatric population in Korea based on a retrospective multicenter review of hospital data. Although only 18 out of 89 university hospitals were included in this study, these hospitals have a nationwide distribution.
The distribution of causative bacteria responsible for invasive bacterial infections differs according to country and study period. Saarinen et al. reported in a Finnish study performed during the 1980s that S. agalactiae and S. aureus accounted for 31% and 15% of invasive infections among neonates younger than 1 month of age, while H. influenzae and S. pneumoniae accounted for 29% and 19% of infections among infants older than 1 month of age (9). During a similar period, S. pneumoniae was most frequently detected in Korean children older than 2 months of age, and accounted for 24% of infections, similar to the Finnish study (10). However, S. aureus and Salmonella species were more common in Korea than in Finland with a frequency of 24% and 23%, respectively, while H. influenzae was relatively less common, accounting for only 14% of infections in Korea. In addition, there were fewer N. meningitidis infections in Korea than in other countries (10).
It is well known that the distribution of causative bacterial organisms changes with time. We detected significant changes in bacterial etiology in Korea compared to previous studies (10). Previously, Nam et al. (10) reported on the distribution of the bacterial pathogens responsible for invasive infections among immunocompetent children aged 2 months to 15 yr between 1986 and 1995. These authors found that S. aureus, S. pneumoniae, Salmonella species, and H. influenzae were responsible for the majority of invasive infections and accounted for 24%, 24%, 23%, and 14% of infections, respectively (10). Several previous studies performed in Korea reported that the estimated incidence of neonatal S. agalactiae infection was much lower than in other developed and developing countries, due to the low prevalence of S. agalactiae colonization in pregnant women (13, 14). Some notable findings of our study compared to previous studies are as follows. First, our data show that the proportion of S. pneumoniae and S. aureus infections increased, but the proportion of Salmonella species and H. influenzae infections decreased sharply in children older than 3 months of age. Second, the proportion of S. agalactiae infections was much higher than expected from previous reports.
S. aureus colonizes 50% of the general population at least once in their lifetime and causes a variety of diseases across all ages (15). S. aureus has been reported to be the dominant neonatal pathogen in western countries and in Korea (1, 13, 16). S. aureus causes the majority of skin, soft tissue, bone, and joint infections. Bacteremic infections caused by S. aureus are frequently nosocomial but in a pediatric study, about half of these infections were community-acquired and common in infants younger than 1 yr of age (17). Pneumonia due to S. aureus is common in early infancy (18). Generally, the frequencies of S. aureus infections in different age groups found in our study are consistent with those reported in previous studies. Although we could not determine the absolute increase in the incidence rate of S. aureus infections in our study, we did observe an increase in the relative proportion of S. aureus infections during the study period. This finding may be due either to the relative decrease in the number of H. influenzae infections or an increase in the number of nosocomial infections (19). However, considering that the subjects included in our study were apparently immunocompetent infants and children, the proportion of S. aureus nosocomial infections in our study was likely very small.
S. agalactiae remains the most important pathogen responsible for neonatal invasive infections in developed countries, despite the great improvements achieved by maternal antimicrobial prophylaxis programs. Furthermore, although maternal screening programs have reduced early onset S. agalactiae infections, late onset infections have not been prevented (20). In this study, the proportion of S. agalactiae infections among infants less than 3 months of age was high throughout the study period, ranging from 30% to 65% of cases, and appears to have increased slightly since the late 1990s. This is a significant finding, because S. agalactiae was not previously regarded as an important organism associated with neonatal infections in Korea. Previous Korean studies on the etiology of neonatal invasive infections reported that the most prevalent organisms were E. coli in the 1960s, S. aureus in the 1970s, and S. aureus and S. epidermidis since the 1980s (16). A recent study also reported that S. aureus and coagulase-negative staphylococci were the most frequently detected pathogens among neonates; S. agalactiae was identified in only 0.4% of cases (13). In contrast, we reported in a previous study that S. agalactiae and S. aureus were the most frequent organisms and accounted for 38% and 19% of invasive infections that occurred in infants less than 3 months of age, respectively, consistent with the results of the current study (11). This discrepancy may partly be due to differences in case definitions. In the prior Korean studies, cases with a single positive blood culture result with clinical features suggesting sepsis were included and all neonatal infections were enrolled, including infections in premature babies, patients with congenital anomalies, and patients in the intensive care unit. However, in the current study, only infections from previously healthy full-term neonates were analyzed. For a more accurate description of the epidemiology of neonatal infections, further studies that specifically target this age group are required. Based on our findings, we conclude that S. agalactiae infections are as prevalent as S. aureus infections in healthy Korean neonates.
S. pneumoniae is the major etiologic agent of invasive bacterial infections in children. In this study, S. pneumoniae accounted for 45% of infections that occurred among children aged between 3 months and 5 yr of age, consistent with the findings of previous studies. With the reduction in the number of H. influenzae infections, S. pneumoniae was the predominant pathogen associated with meningitis, bacteremia without localizing signs, and pneumonia in this age group during the study period. In addition to the large number of cases, its severity, measured as the case-fatality rate, and residual sequelae make S. pneumoniae an important bacterial pathogen and target for a vaccination program. Furthermore, S. pneumoniae has a high rate of resistance to antibiotics in Korea (21). As noted from the experience of other countries, S. pneumoniae infections can be dramatically reduced with universal vaccination using a 7-valent pneumococcal conjugate vaccine. Data from the Active Bacterial Core surveillance (ABCs) showed a rapid decline in the incidence of invasive pneumococcal infections from 87.4 per 100,000 children younger than 5 yr of age in 1999 to 21.2 in 2005 (22, 23). The pneumococcal conjugate vaccine was introduced in Korea in 2003. By 2007, only 12.5% of Korean children had completed the primary series of pneumococcal conjugate vaccinations (unpublished data). Therefore, the proportion of S. pneumoniae infections in this study represents the pre-vaccination era incidence of S. pneumoniae infections.
H. influenzae was an important cause of invasive bacterial infections such as meningitis, pneumonia, epiglotitis, arthritis, and cellulitis in infants and young children before an effective vaccine was introduced. Although few studies on the disease burden associated with H. influenzae infections in Eastern Asian countries in the pre-vaccination era are available, it has been assumed that the incidence of H. influenzae infections was slightly lower in these countries than in the United States or European countries (5, 24). In a compilation of seven studies, H. influenzae was the etiologic agent in only 30% of bacterial meningitis infections among Korean children (24). Nam et al. also reported that H. influenzae infections accounted for only 13.9% of all invasive infections that occurred in children older than 2 months of age. Nevertheless, H. influenzae was a more common cause of bacterial meningitis than S. pneumoniae in the pre-vaccination era in Korea (5, 10).
In many developed countries where H. influenzae conjugate vaccine is routinely given to all infants, the incidence of H. influenzae invasive infections has declined dramatically (25). In Korea, H. influenzae conjugate vaccine has been available since 1996. H. influenzae vaccine has not been included in the National Immunization Program to date; it is available as an optional vaccine, and there has been a gradual increase in its use. Kim et al. estimated the vaccine uptake rate to be 16% in Jeollabuk-do in 2002 (5); in a recent nationwide surveillance study, the vaccine uptake rate was estimated to be 65.2% in 2007 (unpublished data). In this study, H. influenzae infections comprised 10.2% of all invasive bacterial infections and 38.9% of meningitis infections that occurred in children 3 months of age or older. These findings are consistent with data from the pre-vaccination era. However, a vaccination effect was observed when the results were analyzed by dividing the study period into two parts. In the first half of the study period, H. influenzae infections accounted for 20.1% (56/279) of all invasive infections and 54.2% (45/83) of meningitis infections in children 3 months of age or older. However, this dropped to 4.5% (22/489) of all invasive infections and 19.7% (13/66) of all meningitis infections in the latter half of the study period. Therefore, a vaccination effect is evident in Korea.
Salmonella species are one of the most important water- and food-borne pathogens in developing countries. With improvements in hygiene in developed countries, Salmonella infections have decreased although in some countries, an increase in Salmonella bacteremia has been reported (26). In this study, Salmonella infections decreased from 23% in the ten years prior to 1996 to 10% between 1996 and 2005 (10); however, a constant rate of infection was observed during the study period. This observed decrease was probably due to improvements in hygiene since the study period investigated by Nam et al. (10). However, Salmonella species were still very commonly isolated in bacteremia without localizing signs in children 3 months of age or older; 21% of the infections in this age group were attributed to this organism. Of 78 Salmonella isolates, serogroup data was available for 70. Among these, 33 isolates were S. typhi and another 3 isolates were S. paratyphi. Although S. typhi and S. paratyphi may cause extra-intestinal salmonellosis, the proportions of these two isolates were quite high compared to the findings reported by other countries (27, 28). Among non-typhoid salmonellosis cases, serogroups B and D were most frequently isolated and accounted for 17% and 16% of all Salmonella isolates for which serogroup data was available.
In this study, the pathogens associated with a high case fatality rate were S. pneumoniae, S. agalactiae, and N. meningitidis with fatality rates of 12.4%, 10.4%, and 15.4%, respectively. The case fatality rate due to invasive pneumococcal infections was comparable to the 13.0% reported by Nam et al. (10) and the 12.0% reported by Lee et al. (11). However, the case fatality rates were slightly worse than those reported by ABCs for S. pneumoniae, S. agalactiae, and N. meningitidis of 9.3%, 9.5%, and 13.7%, respectively. The overall case fatality rate (11.9%) due to meningitis was slightly better than that reported by Nam et al. (14.3%) a decade earlier and that reported by Lee et al. (18%) for a single tertiary center. This difference may be due to improved management over time and patient selection bias. However, when analyzed by organism, the case fatality rate of pneumococcal versus non-pneumococcal meningitis was 26.7% vs 4.5%. Although case fatality rate due to pneumococcal meningitis improved in the latter half of the study period from 31.8% to 21.7%, this fatality rate is still significantly higher than that of developed countries (29). The case fatality rates due to invasive pneumococcal infections other than meningitis were low at 4.9%. The reason for the higher fatality rate due to pneumococcal meningitis in Korea is unclear. However, this finding highlights the importance of implementation of pneumococcal conjugate vaccination in Korea. The case fatality rate of bacteremia without localizing signs was 5.9%. All mortalities due to this clinical entity were attributed to three organisms: S. pneumoniae, S. aureus, and S. agalactiae. The case fatality rate due to infection by S. pneumoniae, S. aureus, and S. agalactiae was 9.7%, 4.6%, and 11.1%, respectively. The case fatality rate due to other clinical entities was 2.0%.
This study had several limitations. We targeted only eight bacterial organisms. However, in a previous study that we performed at the Seoul National University Hospital and published in 2005, we showed that these eight organisms accounted for 88% of all invasive bacterial infections (11). Therefore, by focusing on these eight bacterial organisms, most of the invasive bacterial infections were likely included in our analysis. Nevertheless, Gram-negative bacteria and bacteria with low pathogenicity such as coagulase-negative staphylococci are relatively important organisms in neonates, thus our study results might have been skewed by focusing only on eight bacterial organisms. In addition, because we included hospital-acquired infections in our study in contrast to previous studies, the possibility of bias cannot be ruled out. The retrospective design of the study may also have resulted in a bias. A selection bias might also have been introduced by doctors requesting laboratory tests for office patients; however, cases with mild illness such as occult bacteremia, where the attending doctor might not perform cultures, were excluded from this study. Because S. pneumoniae is the most common cause of occult bacteremia (30), the proportion of S. pneumoniae might have been underestimated. Variations in laboratory protocols for detection of bacteria in the participating hospitals could also have affected our results. Earlier cases might have been missed because of missing medical record information. For a more accurate description of the distribution and etiology of invasive bacterial infections in Korea, further well-designed prospective studies are needed.
In conclusion, the relative importance of H. influenzae and Salmonella species as invasive pathogens in Korean children is decreasing compared to S. pneumoniae and S. aureus. In contrast to previous studies, invasive S. agalactiae infections were as common as S. aureus infections in young infants. Future health policies need to focus on S. pneumoniae and S. agalactiae infections because these infections are both common and severe.
Figures and Tables
Fig. 1
Distribution of causative bacterial organisms in invasive infections in immunocompetent Korean children between 1996 and 2005 according to age group and clinical spectrum.

Fig. 2
Temporal changes in the relative proportions of the four most prevalent causative bacterial organisms of invasive infections in immunocompetent Korean children 3 months of age or older between 1996 and 2005.

AUTHOR SUMMARY
Etiology of Invasive Bacterial Infections in Immunocompetent Children in Korea (1996-2005): A Retrospective Multicenter Study
Joon-Ho Lee, Hye Kyung Cho, Kyung-Hyo Kim, Chang Hwi Kim, Dong Soo Kim, Kwang Nam Kim, Sung-Ho Cha, Sung Hee Oh, Jae Kyun Hur, Jin Han Kang, Jong Hyun Kim, Yun-Kyung Kim, Young Jin Hong, Eun Hee Chung, Soo-Eun Park, Young Youn Choi, Jung Soo Kim, Hwang Min Kim, Eun Hwa Choi, and Hoan Jong Lee
The aim of this study was to investigate distribution of 8 major causative organisms of childhood invasive infectious diseases by retrospective measure in 18 university hospitals during 1996-2005. S. agalactiae was frequent in meningitis, bacteremia and bone and joint infections of young infants (< 3 months). S. aureus was frequent in meningitis and bacteremia of young infants and bone and joint infections of all age groups. S. pneumoniae was frequent in meningitis, bacteremia and pneumonia of the elder patients (> 3 months) H. influenzae was frequent in meningitis in the first half of study period but significantly decreased during the latter half of the study period. Salmonella species were frequent in bacteremia and bone and joint infections of the elder patients. S. pyogenes, N. meningitidis and L. monocytogenes were less frequently identified.
References
1. McCracken GH Jr. Group B streptococci: the new challenge in neonatal infections. J Pediatr. 1973. 82:703–706.
2. Schuchat A, Hilger T, Zell E, Farley MM, Reingold A, Harrison L, Lefkowitz L, Danila R, Stefonek K, Barrett N, Morse D, Pinner R. Active Bacterial Core Surveillance Team of the Emerging Infections Program Network. Active bacterial core surveillance of the emerging infections program network. Emerg Infect Dis. 2001. 7:92–99.
3. Adams WG, Deaver KA, Cochi SL, Plikaytis BD, Zell ER, Broome CV, Wenger JD. Decline of childhood Haemophilus influenzae type b (Hib) disease in the Hib vaccine era. JAMA. 1993. 269:221–226.
4. Hsu K, Pelton S, Karumuri S, Heisey-Grove D, Klein J. Massachusetts Department of Public Health Epidemiologists. Population-based surveillance for childhood invasive pneumococcal disease in the era of conjugate vaccine. Pediatr Infect Dis J. 2005. 24:17–23.
5. Kim JS, Jang YT, Kim JD, Park TH, Park JM, Kilgore PE, Kennedy WA, Park E, Nyambat B, Kim DR, Hwang PH, Kim SJ, Eun SH, Lee HS, Cho JH, Kim YS, Chang SJ, Huang HF, Clemens JD, Ward JI. Incidence of Haemophilus influenzae type b and other invasive diseases in South Korean children. Vaccine. 2004. 22:3952–3962.
6. Shin S, Shin YJ, Ki M. Cost-benefit analysis of Haemophilus influenzae type B immunization in Korea. J Korean Med Sci. 2008. 23:176–184.
7. Choi E. Direct and indirect effects of pneumococcal protein conjugate vaccine. J Korean Med Assoc. 2008. 51:119–126.
8. Korean statistical information service. KOSIS. accessed on 18 Aug 2010. Available at http://kosis.kr/nsportal/index/index.jsp.
9. Saarinen M, Takala AK, Koskenniemi E, Kela E, Rönnberg PR, Pekkanen E, Kiiski P, Eskola J. Finnish Pediatric Invasive Infection Study Group. Spectrum of 2,836 cases of invasive bacterial or fungal infections in children: results of prospective nationwide five-year surveillance in Finland. Clin Infect Dis. 1995. 21:1134–1144.
10. Nam SG, Lee HJ. Etiology of invasive bacterial infections in apparently healthy children. Korean J Infect Dis. 1998. 30:227–234.
11. Lee JH, Song EK, Lee JA, Kim NH, Kim DH, Park KW, Choi EH, Lee HJ. Clinical entities and etiology of invasive bacterial infections in apparently healthy children. Korean J Pediatr. 2005. 48:1193–1200.
12. Stoll BJ. Kligman RM, Behrman RE, Jenson HB, Stanton BF, editors. Infections of the neonatal infant. Nelson textbook of pediatrics. 2007. 18th ed. Philadelphia: Elsevier Saunders;794–811.
13. Kim KA, Shin SM, Choi JH. A nationwide survey on the causative organisms of neonatal sepsis in Korea. J Korean Pediatr Soc. 2002. 45:55–63.
14. Moon JH, Oh SH, Kim HW, Moon SJ, Choi TY. Neonatal sepsis and antimicrobial susceptibilities in the neonatal intensive care unit and nursery. Korean J Pediatr Infect Dis. 2002. 9:163–174.
15. Ammerlaan HS, Kluytmans JA, Wertheim HF, Nouwen JL, Bonten MJ. Eradication of methicillin-resistant Staphylococcus aureus carriage: a systematic review. Clin Infect Dis. 2009. 48:922–930.
16. Lee JH, Park JJ, Sung IK, Lee BC. Clinical observation in 40 cases with neonatal sepsis. J Korean Pediatr Soc. 1990. 33:1489–1494.
17. Suryati BA, Watson M. Staphylococcus aureus bacteraemia in children: a 5-year retrospective review. J Paediatr Child Health. 2002. 38:290–294.
18. Sattler CA, Correa AG. Feigin RD, Cherry JD, Demmler GJ, Kaplan SL, editors. Coagulase-positive staphylococcal infections (Staphylococcus aureus). Textbook of pediatric infectious diseases. 2004. 5th ed. Philadelphia: Elsevier Saunders;1099–1129.
19. Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998. 339:520–532.
20. Centers for Disease Control and Prevention (CDC). Perinatal group B streptococcal disease after universal screening recommendations-United States, 2003-2005. MMWR Morb Mortal Wkly Rep. 2007. 56:701–705.
21. Jang GC, Shin KM, Yong DE, Lee KW, Kim DS. Changing patterns of antibiotic-resistant rates and clinical features in pneumococcal infections. Korean J Pediatr Infect Dis. 2003. 10:81–86.
22. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Streptococcus pneumoniae, 1999. Centers for Disease Control and Prevention. accessed on 18 Aug 2010. Available at http://www.cdc.gov/abcs/survreports/spneu99.pdf.
23. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Streptococcus pneumoniae, 2005. Centers for Disease Control and Prevention. accessed on 18 Aug 2010. Available at http://www.cdc.gov/abcs/survreports/spneu05.pdf.
24. Lee HJ. Epidemiology of systemic Haemophilus influenzae disease in Korean children. Pediatr Infect Dis J. 1998. 17:9 Suppl. S185–S189.
25. Peltola H. Worldwide Haemophilus influenzae type b disease at the beginning of the 21st century: global analysis of the disease burden 25 years after the use of the polysaccharide vaccine and a decade after the advent of conjugates. Clin Microbiol Rev. 2000. 13:302–317.
26. Yagupsky P, Maimon N, Dagan R. Increasing incidence of nontyphi Salmonella bacteremia among children living in southern Israel. Int J Infect Dis. 2002. 6:94–97.
27. Ispahani P, Slack RC. Enteric fever and other extraintestinal salmonellosis in University Hospital, Nottingham, UK, between 1980 and 1997. Eur J Clin Microbiol Infect Dis. 2000. 19:679–687.
28. Vugia DJ, Samuel M, Farley MM, Marcus R, Shiferaw B, Shallow S, Smith K, Angulo FJ. Emerging Infections Program FoodNet Working Group. Invasive Salmonella infections in the United States, FoodNet, 1996-1999: incidence, serotype distribution, and outcome. Clin Infect Dis. 2004. 38:Suppl 3. S149–S156.
29. Arditi M, Mason EO Jr, Bradley JS, Tan TQ, Barson WJ, Schutze GE, Wald ER, Givner LB, Kim KS, Yogev R, Kaplan SL. Three-year multicenter surveillance of pneumococcal meningitis in children: clinical characteristics, and outcome related to penicillin susceptibility and dexamethasone use. Pediatrics. 1998. 102:1087–1097.
30. Alpern ER, Alessandrini EA, Bell LM, Shaw KN, McGowan KL. Occult bacteremia from a pediatric emergency department: current prevalence, time to detection, and outcome. Pediatrics. 2000. 106:505–511.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download