Abstract
Background
Low back pain is a frequent condition that results in substantial disability and causes admission of patients to neurosurgery clinics. To evaluate and present the therapeutic outcomes in lumbar disc hernia (LDH) patients treated by means of a conservative approach, consisting of bed rest and medical therapy.
Methods
This retrospective cohort was carried out in the neurosurgery departments of hospitals in Kahramanmaraş city and 23 patients diagnosed with LDH at the levels of L3−L4, L4−L5 or L5−S1 were enrolled.
Results
The average age was 38.4 ± 8.0 and the chief complaint was low back pain and sciatica radiating to one or both lower extremities. Conservative treatment was administered. Neurological examination findings, durations of treatment and intervals until symptomatic recovery were recorded. Laségue tests and neurosensory examination revealed that mild neurological deficits existed in 16 of our patients. Previously, 5 patients had received physiotherapy and 7 patients had been on medical treatment. The number of patients with LDH at the level of L3−L4, L4−L5, and L5−S1 were 1, 13, and 9, respectively. All patients reported that they had benefit from medical treatment and bed rest, and radiologic improvement was observed simultaneously on MRI scans. The average duration until symptomatic recovery and/or regression of LDH symptoms was 13.6 ± 5.4 months (range: 5−22).
Conclusions
It should be kept in mind that lumbar disc hernias could regress with medical treatment and rest without surgery, and there should be an awareness that these patients could recover radiologically. This condition must be taken into account during decision making for surgical intervention in LDH patients devoid of indications for emergent surgery.
Low back pain (LBP) is a frequent condition that results in substantial disability and causes admission of patients to neurosurgery clinics [1]. Radiating acute lumbar back pain can point out severe neurologic sequelae and indications such as tumor, infection, cauda equina syndrome, and fracture, which necessitate emergent surgical intervention, should be excluded [2]. If symptoms and signs consistent with these circumstances like urinary retention, fecal incontinence, or saddle anesthesia can be ruled out, a cycle of conservative treatment can be administered for six weeks [34]. If symptoms persistent over 6 weeks, or deterioration of neurologic function arises, there may be a need for radiologic imaging and further invasive procedures [234].
A majority of patients with an LDH display recovery with conservative management involving active lifestyle, non-steroidal anti-inflammatory drugs, systemic steroids, steroid injections, or physical therapy [56]. Moreover, no noteworthy difference could be observed between the therapeutic outcomes of conservative and surgical treatment after a period of 2 years [7]. Hence, the preference of the patient and severity of pain-related disability should be taken into account during determination of the therapeutic approach.
Acute LDH can predispose sufferers to serious pain that causes significant disability and functional limitation that usually responds well to conservative management [5]. Surgical treatment must be reserved for more severe and urgent conditions or cases refractory to medical treatment [78].
The aim of the present study was to evaluate and present our clinical outcomes with conservative treatment of LDH in patients suffering from LBP and sciatica.
This retrospective cohort was carried out in the neurosurgery departments of hospitals in Kahramanmaraş city following the approval of the local Institutional Review Board. Written informed consent was obtained from every patient.
A total of 23 patients complaining of LBP and sciatica were diagnosed as LDH between 2010 and 2015. Descriptive parameters, clinical and neurological examination findings, as well as radiological information derived from magnetic resonance imaging views were recorded. Clinical entities such as tumor, infection, cauda equina syndrome, and fracture, which require emergent surgical intervention, were not detected in any cases. Similarly, no patients suffered from urinary retention, fecal incontinence, or saddle anesthesia. Eleven patients who had not received medical treatment before were inappropriate for surgery. Inclusion criteria were age ≥ 18 years, radiating pain and/or paresis below knee level, and an LDH at the corresponding level and side which had been verified by MRI scan. Patients with a history of osteoporosis, immunosupression, chronic corticosteroid use, intravenous drug use, fever of unknown origin, history of cancer, unexplained weight loss, or progressive/disabling symptoms, associated with focal neurologic deficits, were excluded from the study.
Complaints, physical/neurologic examination findings, and radiologic data derived from lumbar MRI views at initial admission, were compared to those of the control.
Since bed rest is less effective than activity for sciatica, it was limited to omit muscular deconditioning [4].
Symptoms were considered as linked with sciatica from a LDH if pain was worse in the leg than in the low back, a characteristic dermatomal distribution, neurologic symptoms such as numbness, pain, sensation of cold, and pain aggravated with the Valsalva maneuver [9]. Moreover, less common symptoms like nonradiating pain and sensory/motor deficits were identified [9].
Physical examination involved a complete examination of the pelvis and lower extremities as well as neurologic assessment. Thus, not only sensation, strength, and reflexes were evaluated; but also the Laségue (straight-leg-raise) test was utilized to diagnose an underlying LDH. In spite of its low specificity, the Laségue test is a sensitive diagnostic tool for ruling in LDH [10].
The Laségue test was performed in a supine position to enhance its sensitivity [1]. A positive result was defined as radiating pain encountered at 30° to 70° of hip flexion and a smaller angle was interpreted as a more remarkably positive result. In the crossed Laségue test, which is more specific for LDHs, presence of radiating pain in the affected leg is assessed while the contralateral, uninvolved leg is lifted. Impairments of great toe dorsiflexion and ankle plantar flexion may reflect an LDH at the levels of L4-L5 and L5-S1, respectively [10111213].
The evaluation of MRI views was carried out by the same radiologist, who had an experience of 10 years in musculoskeletal system radiology. The radiologist was blinded to the clinical data and therapeutic outcomes of the study.
Conservative management comprised the prescription of effective NSAIDs and muscle relaxants according to prevailing guidelines. Nonsteroidal anti-inflammatory drugs and muscle relaxants were given in the form of tablets (twice daily) and gels (once a day) for a period of 4 to 10 weeks. In 5 patients, hospitalization and introduction of intravenous tramadol (100 mg, twice daily) (Contramal®, Abdi İbrahim, Istanbul, Turkey) and pethidine hydrochloride (50 mg, twice daily) (Aldolan®, Liba Laboratories, Istanbul, Turkey) were introduced due to intractable pain (Table 1). Patients were advised to stay as active as possible and to resume daily activities if feasible. If patients had considerable fear of movement, guidance was provided by the neurosurgeon (IA).
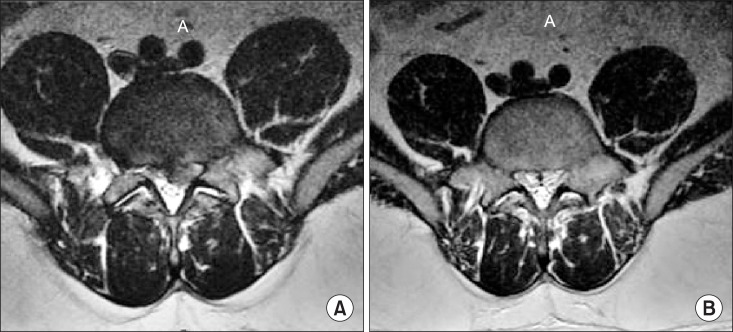
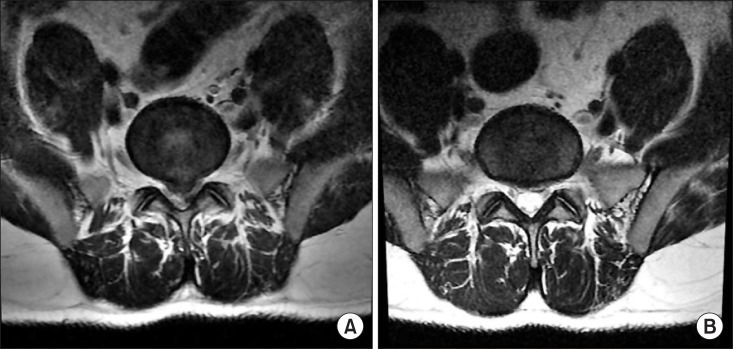
An outline of descriptive, clinical, and radiologic findings before and after medical teratment and bed rest are presented in Table 1. Five cases with neurologic deficits that did not have sufficient benefit from previous medical and physical treatment, and the remaining 7 patients without neurologic deficits, declined surgery. The average age was 38.4 ± 8.0 (range: 27-53) and the chief complaint was LBP and sciatica radiating to one or both lower extremities. One patient had an LDH at the level of L3-L4, thirteen patients had LDHs at the level of L4-L5, and 9 patients had a disc herniation at the level of L5-S1. In 23 patients, the Laségue test and neurologic examination revealed mild neurological deficits. Physical treatment was administered in 5 patients and 7 patients had received irregular courses of medical treatment including NSAIDs and muscle relaxants. All patients reported that they had substantial benefit from medical treatment and bed rest. They were able to perform their daily activities without any restriction after conservative treatment. The average duration until symptomatic recovery and regression of LDH-associated symptoms was 13.6 ± 5.4 months (range: 5-22). Fig. 1 demonstrate the sagittal MRI views of the patient who reported recovery at the 7th month after treatment. Fig. 2 represent the axial MRI views of the same patient before and after treatment, respectively. Similarly, Fig. 3 is the sagittal MRI views of another LDH patient before and after treatment. This patient reported a complete disappearance of complaints at 16th month and Fig. 4 represents the axial MRI views of the same patient before and treatment.
The present study attempted to present our clinical outcomes with conservative management of LDHs in patients with LBP and sciatica. Analysis of our data revealed that medical treatment and bed rest with close follow-up may be a promising therapeutic option in selected LDH cases devoid of indications for emergent surgical intervention.
The burden of LBP on patients and society is substantial, and it ranks first as the disease with the most years lived with disability. The vast majority of patients suffering from LBP seek medical care. Most of the episodes are temporary, and tend to resolve without treatment even in the presence of specific underlying causes such as LDH. There are high direct and indirect costs at tirbuted to healthcare utilization and loss of productivity. Even though conservative treatment, including a “wait and see policy”, constitutes the first step, surgical intervention can be unavoidable with certain indications [14].
Lumbar disc hernia is a frequent cause of LBP, and nonoperative care of an LDH consists of various methods such as lumbar support, bed rest, oral non-steroidal anti-inflammatory medications, muscle relaxants, physical therapy, epidural steroid injections, behavioural therapy and spinal manipulation. Different levels of success rates have been reported with this wide spectrum of therapeutic modalities [15].
In the vast majority of LDH patients, sciatica seems to improve in 6 weeks and may recover by 12 weeks after the onset of conservative management [3]. Some of these nonsurgical treatment modalities have proven effective in alleviation of LDH symptoms and should be regarded as first-line, particularly in the initial 6 weeks of conservative management. Bed rest must be advised in conjunction with maintenance of an active life style [4].
Non-steroidal anti-inflammatory drugs (NSAIDs) including acetaminophen and muscle relaxants are useful for treatment of nonspecific LBP. Efficacy of these medications for LBP associated with LDHs has not been extensively studied [1617]. Despite the controversial conclusions drawn from relevant literature [18], our results support that NSAIDs can be useful in relief of LDH symptoms. However, effectivities of NSAIDs and muscle relaxants remain to be elucidated in further controlled trials on larger series. We did not administer systemic ste roids, since they are not superior to placebo in LBP due to the LDHs [19]. Similarly, physical therapy was not performed in our series because its role and the cost-effectivity of physical therapy in these circumstances is under debate [20].
Emergent surgery is indicated in patients with epidural abscesses, cauda equine syndrome, or severe and progressive neurologic deficits. Patients without improvement at the end of 6 weeks of conservative treatment need assessment for surgery following radiologic imaging. Patients with persistent neurologic deficits, severe sciatica with a positive Lasegue test, and confirmation of LDH at the nerve root, in accordance with the clinical findings, are suitable candidates for surgery. The goal of surgical treatment is to alleviate the compression over the nerve root and to relieve the irritation from the LDH [8]. In selected cases, surgical discectomy seems to provide faster symptomatic relief and recovery from disability compared to conservative treatment in the first 2 years after surgery [68]. However, the outcomes are similar for conservative and surgical treatment after 2 years [68]. The ideal time for surgery also remains obscure, but a course of conservative treatment for at least 6 weeks is recommended before surgery [7].
It must be noted that our series consisted of relatively younger patients with mild symptoms, and all patients were unwilling for any surgical intervention. Therefore, selection of therapeutic approach must be made with respect to the preference of the patient, physical examination findings, and clinical/radiologic features.
In accordance with a publication by Rhee et al. [21], our results confirm that lumbar disc herniation may reabsorb with time, and symptomatic recovery may occur in many patients after a course of conservative management only. Surgical treatment should be maintained for patients with clinical findings well-correlated with radiologic data and it must be declared that results of surgery and conservative treatment in terms of pain and disability will be similar. On the other hand, patients who decline surgical treatment and prefer conservative treatment must be aware of the fact that their symptomatic recovery will be slower in the beginning.
In the literature, a correlation could not be established between physical examination findings and the size of the herniated disc on MRI scans [22]. Clinical improvement is mostly linked with radiologic regression of the disc [23]. Nevertheless, longitudinal studies focusing on conservatively managed LDH patients did not indicate a direct relationship between clinical and radiologic improvements [24]. Clinical improvement may occur either without any notable morphological changes or symptomatic recovery may precede the radiologic alterations. This finding may be attributed to the gradual diminution of the pressure applied by the herniated disc on the adjacent neural structures and the progressive recovery of the inflammatory reaction [25]. The only remarkable prognostic finding in MRI views of patients with acute LBP was the presence of disc herniation [26]. Although noteworthy structural alterations may occur in the appearance of disc hernations during follow-up, there were not any certain changes on MRI sections that are likely to modify the patient care [22].
Main limitations of the present study include small sample size, lack of a control group, and data derived from the experience of a single institution. Social, ethnic, and environmental factors may have unignoreable impacts on clinical outcomes. Furthermore, the relationship between the resolution of symptoms, and the regression of the herniation by MRI has not been examined. Finally, to compare the outcomes of the non-operative group with a comparable cohort of patients who underwent surgery, looking at clinical outcomes, cost, return to employment etc. would be also benefitical. Thus, extrapolation and generalization from this data must be made with caution.
To conclude, it is thought that with medical treatment and rest, lumbar disc hernias could both recover clinically and show spontaneous regression radiologically. These patients should be followed up closely to avoid more severe and complicated neurological outcomes.
ACKNOWLEDGEMENTS
The authors declare no competing interest. No financial support was received for this paper.
References
1. Gregory DS, Seto CK, Wortley GC, Shugart CM. Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician. 2008; 78:835–842. PMID: 18841731.
2. Dawson E, Bernbeck J. The surgical treatment of low back pain. Phys Med Rehabil Clin N Am. 1998; 9:489–495. PMID: 9894129.

3. Saal JA, Saal JS. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study. Spine(Phila Pa 1976). 1989; 14:431–437. PMID: 2718047.

4. Hagen KB, Hilde G, Jamtvedt G, Winnem M. Bed rest for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2004; CD001254. PMID: 15495012.

5. Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:586–597. PMID: 12353946.

6. Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006; 296:2441–2450. PMID: 17119140.

7. Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007; 356:2245–2256. PMID: 17538084.

8. Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev. 2007; CD001350.

9. Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002; 72:630–634. PMID: 11971050.

10. Kerr RS, Cadoux-Hudson TA, Adams CB. The value of accurate clinical assessment in the surgical management of the lumbar disc protrusion. J Neurol Neurosurg Psychiatry. 1988; 51:169–173. PMID: 3346682.

11. Vroomen PC, Van Hapert SJ, Van Acker RE, Beuls EA, Kessels AG, Wilmink JT. The clinical significance of gadolinium enhancement of lumbar disc herniations and nerve roots on preoperative MRI. Neuroradiology. 1998; 40:800–806. PMID: 9877135.

12. Jackson RP, Cain JE Jr, Jacobs RR, Cooper BR, McManus GE. The neuroradiographic diagnosis of lumbar herniated nucleus pulposus: II. A comparison of computed tomography (CT), myelography, CT-myelography, and magnetic resonance imaging. Spine (Phila Pa 1976). 1989; 14:1362–1367. PMID: 2694389.

13. Modic MT, Ross JS, Obuchowski NA, Browning KH, Cianflocco AJ, Mazanec DJ. Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history. Radiology. 1995; 195:429–435. PMID: 7724762.

14. Jacobs WC, Rubinstein SM, Koes B, van Tulder MW, Peul WC. Evidence for surgery in degenerative lumbar spine disorders. Best Pract Res Clin Rheumatol. 2013; 27:673–684. PMID: 24315148.

15. Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006; 443:183–197. PMID: 16462442.
16. van Tulder MW, Scholten RJ, Koes BW, Deyo RA. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2000; CD000396. PMID: 10796356.
17. van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Cochrane Back Review Group. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the cochrane collaboration. Spine (Phila Pa 1976). 2003; 28:1978–1992. PMID: 12973146.

18. Koes BW, Scholten RJ, Mens JM, Bouter LM. Efficacy of non-steroidal anti-inflammatory drugs for low back pain: a systematic review of randomised clinical trials. Ann Rheum Dis. 1997; 56:214–223. PMID: 9165992.

19. Finckh A, Zufferey P, Schurch MA, Balagué F, Waldburger M, So AK. Short-term efficacy of intravenous pulse glucocorticoids in acute discogenic sciatica. A randomized controlled trial. Spine (Phila Pa 1976). 2006; 31:377–381. PMID: 16481946.

20. Luijsterburg PA, Lamers LM, Verhagen AP, Ostelo RW, van den Hoogen HJ, Peul WC, et al. Cost-effectiveness of physical therapy and general practitioner care for sciatica. Spine (Phila Pa 1976). 2007; 32:1942–1948. PMID: 17700438.

21. Rhee JM, Schaufele M, Abdu WA. Radiculopathy and the herniated lumbar disc. Controversies regarding pathophysiology and management. J Bone Joint Surg Am. 2006; 88:2070–2080. PMID: 17036418.
22. Unlu Z, Tasci S, Tarhan S, Pabuscu Y, Islak S. Comparison of 3 physical therapy modalities for acute pain in lumbar disc herniation measured by clinical evaluation and magnetic resonance imaging. J Manipulative Physiol Ther. 2008; 31:191–198. PMID: 18394495.

23. Mochida K, Komori H, Okawa A, Muneta T, Haro H, Shinomiya K. Regression of cervical disc herniation observed on magnetic resonance images. Spine (Phila Pa 1976). 1998; 23:990–995. PMID: 9589536.

24. Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K. The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976). 1996; 21:225–229. PMID: 8720408.

25. Krause M, Refshauge KM, Dessen M, Boland R. Lumbar spine traction: evaluation of effects and recommended application for treatment. Man Ther. 2000; 5:72–81. PMID: 10903582.

26. Modic MT, Obuchowski NA, Ross JS, Brant-Zawadzki MN, Grooff PN, Mazanec DJ, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2005; 237:597–604. PMID: 16244269.

Fig. 1
The sagittal MRI views of an LDH patient before (A) and after treatment (B). The patient was free of symptoms at 7th month after treatment.
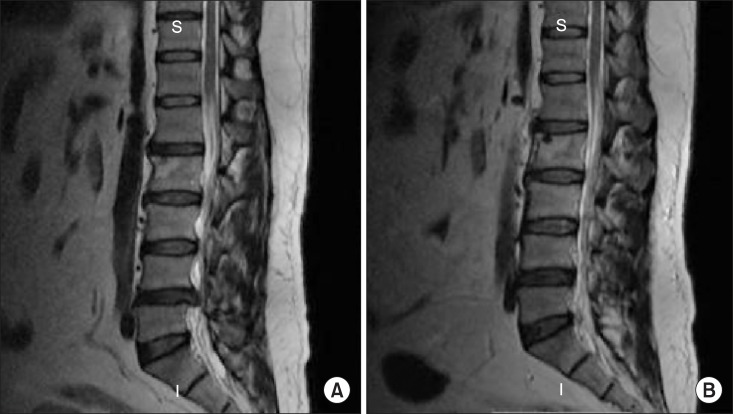
Fig. 3
The sagittal MRI views of another LDH patient before (A) and after treatment (B). The patient was free of symptoms at 16th month after treatment.
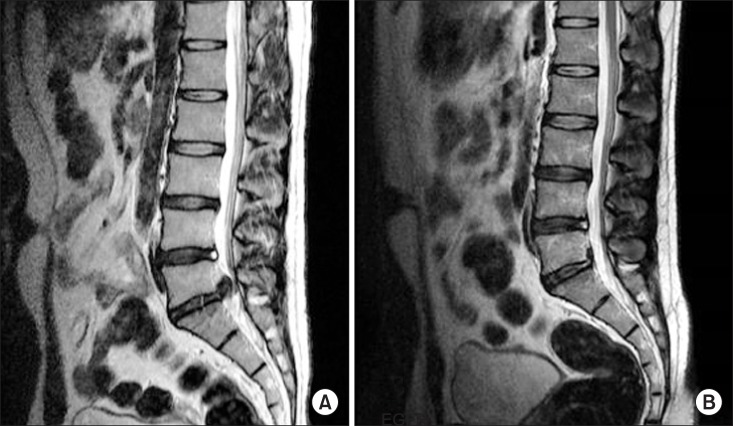
Table 1
An Overview of Descriptive, Clinical and Radiologic Data of Our Series
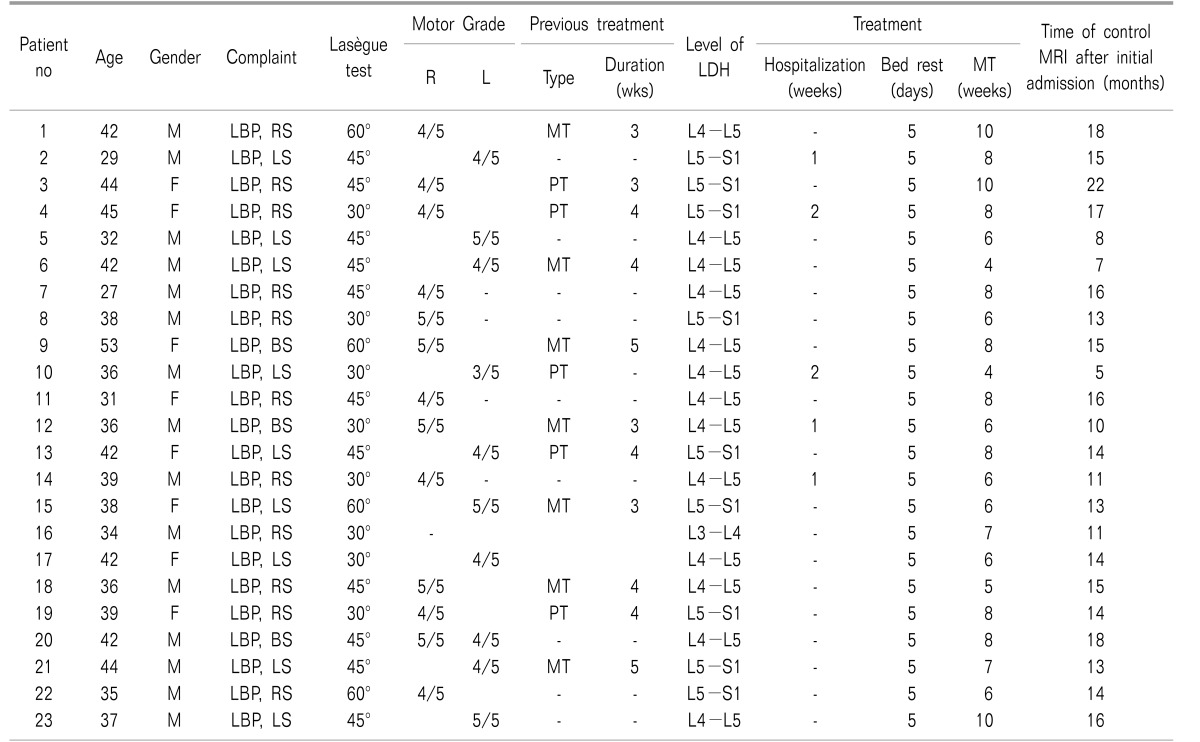
M: male, F: female, R: right, L: left, LBP: low back pain, RS: right sciatica, LS: left sciatica, BS: bilateral sciatica, L: left, MT: medical treatment, PT: physical treatment, LDH: lumbar disc hernia, MRI: magnetic resonance imaging. Hint: Laségue test result indicates the angle that provokes sciatica symptoms in response to the hip flexion at the same side.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download