Abstract
Background
The C-arm fluoroscope is known as the most important equipment in pain interventions. This study was conducted to investigate the completion rate of education on radiation safety, the knowledge of radiation exposure, the use of radiation protection, and so on.
Methods
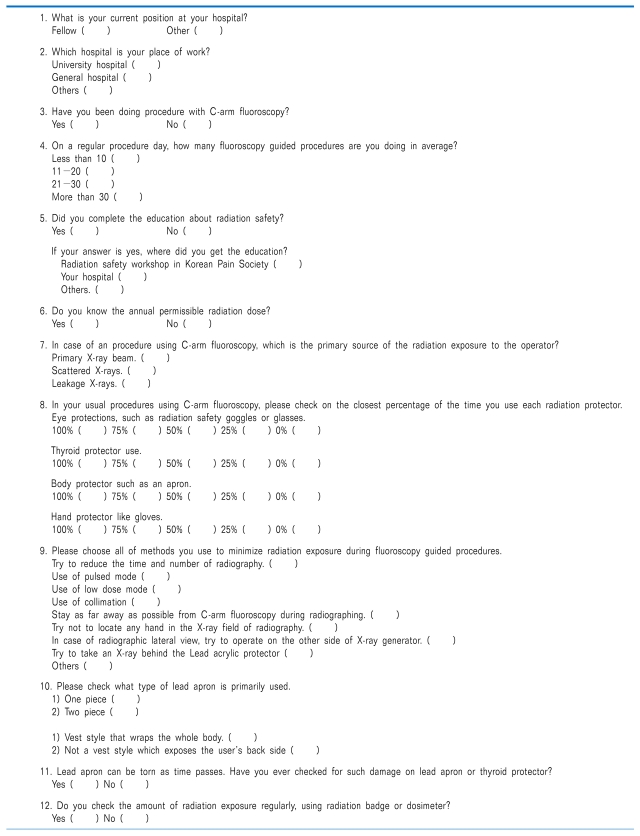
Unsigned questionnaires were collected from the 27 pain physicians who applied for the final test to become an expert in pain medicine in 2011. The survey was composed of 12 questions about the position of the hospital, the kind of hospital, the use of C-arm fluoroscopy, radiation safety education, knowledge of annual permissible radiation dose, use of radiation protection, and efforts to reduce radiation exposure.
Results
In this study, although most respondents (93%) had used C-arm fluoroscopy, only 33% of the physicians completed radiation safety education. Even though nine (33%) had received education on radiation safety, none of the physicians knew the annual permissible radiation dose. In comparing the radiation safety education group and the no-education group, the rate of wearing radiation-protective glasses or goggles and the use of radiation badges or dosimeters were significantly higher in the education group. However, in the use of other protective equipment, knowledge of radiation safety, and efforts to reduce radiation exposure, there were no statistical differences between the two groups.
Radiological methods such as X-ray or CT have been widely used for precise pain management and effective treatment. The C-arm fluoroscope, in particular, is known as the most important equipment in various pain interventions [1]. However, radiation exposure is inevitable when using C-arm fluoroscopy, and doctors are not exempt from this [2].
Many approaches and types of equipment to reduce the radiation exposure produced by C-arm fluoroscopy have been tested in the medical field, and an annual workshop on radiation safety is offered by the Korean Pain Society. Among pain physicians, however, it seems that some are indifferent to radiation exposure.
In Korea, radiation safety education has not been mandatory for pain physicians, and the attention given to radiation safety may be less than that given to the C-arm guided procedure.
This study was conducted to investigate the completion rate of radiation safety education, the knowledge of radiation and protection from fluoroscopic exposure, the use of radiation protective equipment, and the efforts to reduce radiation exposure among applicants to become pain medicine experts.
Unsigned questionnaires were collected from the 27 pain physicians who applied the final test for the expert of pain medicine in 2011. The survey was composed of 12 questions about applicant's hospital position, type of hospital, use of C-arm fluoroscopy, average number of fluoroscopic procedures per day, radiation safety education, knowledge of annual permissible radiation dose [3], use of radiation protection, and efforts to reduce radiation exposure (Appendix).
Each answer was analyzed, and a comparison was made between the education group, who received training in radiation safety, and the no-education group, who received no education about radiation safety.
The comparison between the two groups was analyzed by the chi-square test. Statistical significance was accepted for P values under 0.05.
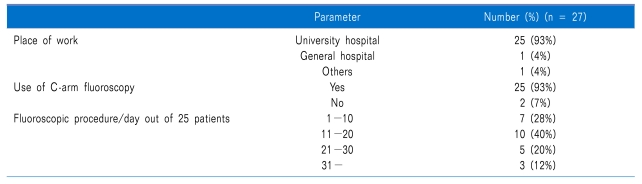
The work place of the respondents was a university hospital for 25 subjects (93%), general hospital for 1 subject (4%), and local clinic for 1 subject (4%); 24 subjects (89%) held the position of fellow, while 3 subjects (11%) were not fellows. Twenty-five subjects (93%) had used C-arm fluoroscopy for interventions. Among these, the number of fluoroscopic procedures per day was under 10 for 7 subjects (28%), between 11 and 20 for 10 subjects (40%), between 21 and 30 for 5 subjects (20%), and over 31 for 3 subjects (12%) (Table 1).
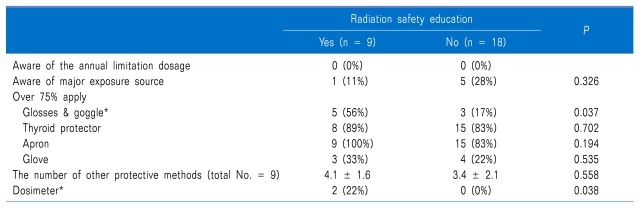
Nine respondents (33%) had received radiation safety education. Five (19%) attended the radiation safety workshop at the annual meeting of the Korean Pain Society, and five (19%) were educated in their hospital. One physician was trained at both the workshop of the Korean Pain Society and the hospital (Table 2).
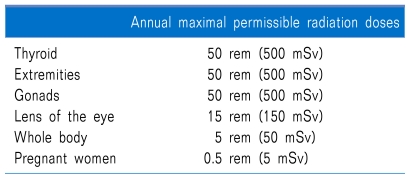
None of the respondents knew the annual permissible radiation dose (Table 3). Also, only 6 people (22%) knew accurately that the most important cause of exposure for physicians is scattered X-ray, among the three types of radiation exposures (primary X-ray beam, scattered X-ray, and leakage X-ray) [4].
The rate of use of radiation protection devices such as goggles or glasses, thyroid protectors, aprons, and gloves is summarized in Fig. 1. Regarding the percentage of time respondents used protective equipment, for glasses or goggles, 2 people (7%) used them 100% of the time, 6 people (22%) used them 75% of the time, 8 people (30%)used them 50% of the time, 1 person (4%) used them 25% of the time, and 10 people (37%) never used them. In the case of thyroid protectors, 16 people (59%) used them 100% of the time, 7 people (26%) 75% of the time, 1 person (4%) 50% of the time, 1 person (4%) 25% of the time, and 2 people (7%) 0% of the time. For body protectors, such as aprons, 22 people (82%) wore them 100% of the time, 2 people (7%) wore them 75% of the time, and 3 people (11%) wore them 50% of the time, In the case of hand protectors such as gloves, 3 people (11%), used them 100% of the time, 4 people (15%) 75% of the time, 5 people (19%) 50, 3 people (11%) 25% of the time, and 12 people (44%) never used them.
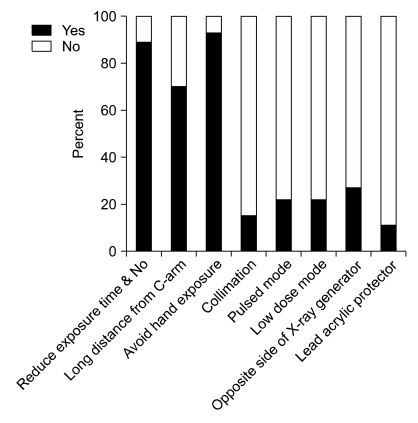
In terms of attempts to reduce radiation exposure, 24 subjects (89%) attempted to reduce the time and frequency of fluoroscopy use, 6 subjects (22%) used pulsed mode, 6 subjects (22%) used low-dose mode, 4 subjects (15%) used collimation, 19 subjects (70%) kept apart from C-arm fluoroscopy when performing procedures, 7 subjects (26%) performed interventions on the opposite side of the X-ray generator in cases of lateral view, and 3 subjects (11%) took shots behind a lead acrylic protector. Twenty-five subjects (93%) particularly attempted to reduce exposure of their hands within the C-arm fluoroscopic radiation field (Fig. 2).
The most common type of apron was one piece, used by 23 subjects (85%), while a two piece type was worn by 4 subjects (15%). Among the one-piece types, 14 people (52%) used the type of vest that completely wrapped around the body and 9 people (33%) used the type that could not protect their back.
Only 3 subjects (11%) had experience with checking atorn apron or thyroid shield by fluoroscopy. A radiation badge or dosimeter was used by only 2 subjects (7%).
Nine people (33%, education group) received an education about radiation safety and 18 people (67%, no-education group) did not. In comparing the two groups, the rate of wearing radiation-protective glasses or goggles and the use of a radiation badge or dosimeter were significantly higher in the education group (Table 2). However, in the use of other protective equipment, knowledge of radiation safety, and efforts to reduce radiation exposure, there were no statistical significances between the two groups.
The amount of radiation absorbed by an individual's tissues corresponds with the risk of developing biologic effects [5]. The biologic effects of radiation are a concern at any level of exposure and can result in erythema, cataracts, and cancer [6]. Among these, the most important risk of prolonged exposure to low-dose ionizing radiation is cancer [7,8]. Therefore, precautions should be taken to reduce exposure as much as possible in most pain physicians.
The amount of radiation exposure is proportional to the duration of exposure and inversely proportional to the square of the distance from the radiation source [9]. Decreased exposure can also be accomplished by increased shielding with a gown, thyroid protector, gloves and glasses; beam collimation; and using the low-dose option available on some C-arm fluoroscopy units [10]. In this study, although most respondents (93%) had used C-arm fluoroscopy, the number of fluoroscopic procedures per day was found to be under 30 in 22 people (88%). Pain physicians have to recognize that the risk of radiation exposure increases with the number of procedures. However, only 33% of the physicians completed radiation safety education. In particular, none of the subjects knew the annual permissible radiation dose. In addition, only 6 people (22%) knew that the most important cause of exposure to physicians is scattered X-rays. Even in the education group (33%), a fair number of respondents did not have exact knowledge about radiation exposure, and only 2 respondents (7%) had checked their personal amount of radiation exposure using a radiation badge or dosimeter. These findings mean that most respondents took no interest in their level of radiation exposure.
Furthermore, many respondents exposed themselves to radiation without any significant protective gear when they used C-arm fluoroscopy for interventions. They generally wore aprons, but radiation-protective eyewear, gloves, or thyroid shields were not frequently worn.
Fourteen people (52%) responded that they wore an apron of the vest type that completely wraps around the body. Unlike this type, the kind of apron that is not a vest but that is open at the back cannot block out radiation that comes through the back. In addition, even if they are the same 0.3 mm lead equivalent, the vest type of apron has double layers in the front, giving the effect of 0.6 mm lead equivalent. The non-vest type, however, only shows as much protective effect as 0.3 mm lead equivalent. Therefore, it can be said that the vest type has a better protective effect than the non-vest type. For example, 0.5 mm of lead, which is the amount normally used in a lead apron, could block 90% of radiation exposure [11].
The International Council on Radiation Protection set an annual permissible radiation dose to reduce the amount of scattered radiation [12,13]. It recommended not to exceed this limit of radiation exposure, and many countries have applied this limit to radiation fields (Table 3) [13]. The annual allowance of whole radiation exposure is 50 mSv, but exposure is limited to an amount not to exceed 20 mSv/year on average over 5 years in Europe, and, regulations limit exposure to only 10 mSv/year over a person's entire life in the USA [14]. So, pain physicians who use C-arm fluoroscopy over a 5-year period need to monitor and control their radiation exposure to maintain levels less than 10 mSv/year.
The continuing increase in the worldwide use of X-ray imaging is creating new challenges for occupational radiation protection of medical staff [15]. Patients' treatment is important, but it is prudent for physicians to have more awareness and concern about radiation safety and its threats, which have been easily ignored, to promote their own and their patients' safety. In comparison between the education group and the no-education group, only two practices (using glasses or goggles and checking a dosimeter) showed statistically significant differences (Table 2), and the others did not. Therefore, even in the education group, the practices learned in the education were not employed.
Radiation safety education must become more practical, and it should be made a mandatory part of fellowship training. If the education is included in the cadaver workshop of the Korean Pain Society, at least, the attendees can gain some knowledge about radiation safety. Additionally, academic advisors must train fellows not only to learn fluoroscopic procedures but also to take an interest in radiation safety, exposure, and protection.
In this study, the respondents knew very little about radiation safety and had a low level of interest in their radiation exposure. In general, except aprons and thyroid protectors, the use of each type of protective equipment was low frequency. Even participants in the education group seem not to put the education they received about radiation safety into practice. To make fluoroscopy use safer, education about, attention to, and practices of radiation safety should be required of all pain physicians.
References
1. Behrend M, Rosenthal R. Acquisition of spine injection skills using a beef injection simulator. Pain Physician. 2007; 10:591–598. PMID: 17660859.
2. Koyama M, Takizawa K, Kobayashi K, Sasaka K, Hoshikawa Y, Nakaji S, et al. Initial experience of percutaneous vertebro-plasty using single-plane C-arm fluoroscopy for guidance. Radiat Med. 2005; 23:256–260. PMID: 16012401.
3. Theocharopoulos N, Damilakis J, Perisinakis K, Manios E, Vardas P, Gourtsoyiannis N. Occupational exposure in the electrophysiology laboratory: quantifying and minimizing radiation burden. Br J Radiol. 2006; 79:644–651. PMID: 16641414.

4. Wagner M, Duwenkamp C, Ludwig W, Dresing K, Bott OJ. An approach to simulate and visualize intraoperative scattered radiation exposure to improve radiation protection training. Stud Health Technol Inform. 2010; 160:625–628. PMID: 20841762.
6. Andreassi MG. The biological effects of diagnostic cardiac imaging on chronically exposed physicians: the importance of being non-ionizing. Cardiovasc Ultrasound. 2004; 2:25. PMID: 15555078.

7. Limacher MC, Douglas PS, Germano G, Laskey WK, Lindsay BD, McKetty MH, et al. ACC expert consensus document. Radiation safety in the practice of cardiology. American College of Cardiology. J Am Coll Cardiol. 1998; 31:892–913. PMID: 9525565.
8. Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A. 2003; 100:13761–13766. PMID: 14610281.

9. Botwin KP, Freeman ED, Gruber RD, Torres-Rames FM, Bouchtas CG, Sanelli JT, et al. Radiation exposure to the physician performing fluoroscopically guided caudal epidural steroid injections. Pain Physician. 2001; 4:343–348. PMID: 16902680.
10. Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005; 13:69–76. PMID: 15712984.

11. Schueler BA. Operator shielding: how and why. Tech Vasc Interv Radiol. 2010; 13:167–171. PMID: 20723831.

12. Sinclair WK. Radiation protection recommendations on dose limits: the role of the NCRP and the ICRP and future developments. Int J Radiat Oncol Biol Phys. 1995; 31:387–392. PMID: 7836093.

13. Tenforde TS. Future role of the NCRP in radiation health protection. Health Phys. 2004; 87:312–318. PMID: 15303070.

14. Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010; 21:607–615. PMID: 20430294.

15. Le Heron J, Padovani R, Smith I, Czarwinski R. Radiation protection of medical staff. Eur J Radiol. 2010; 76:20–23. PMID: 20656429.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download