Abstract
Background
Methods
Results
References
Fig. 1
Correlations and difference plots of HbA1c measurements between different analyzers. (A) G11vr vs G8vr in samples without flags, (B) G11vr vs G11st in samples without flags, (C) G11vr vs G8st in samples without flags, (D) G11vr vs G8vr in samples with flags, (E) G11vr vs G11st in samples with flags, (F) G11vr vs G8st in samples with flags.
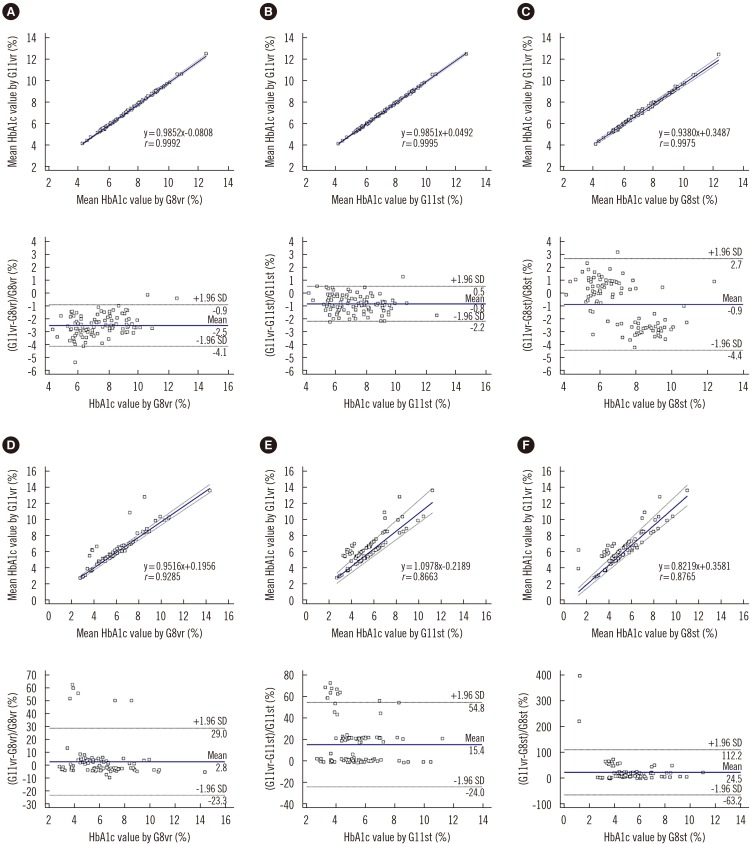
Fig. 2
Box-and-whisker plot of the differences between each analyzer and HPLC-MS HbA1c results for 15 known Hb variants. The central box represents the interquartile range, and the middle line indicates the median (G11vr, 0.2; G8vr, −0.5; G11st, −1.3; G8st, −1.2). A line extends from the minimum to the maximum value, excluding single outlier in G8st, which is displayed as a separate point for G8st.
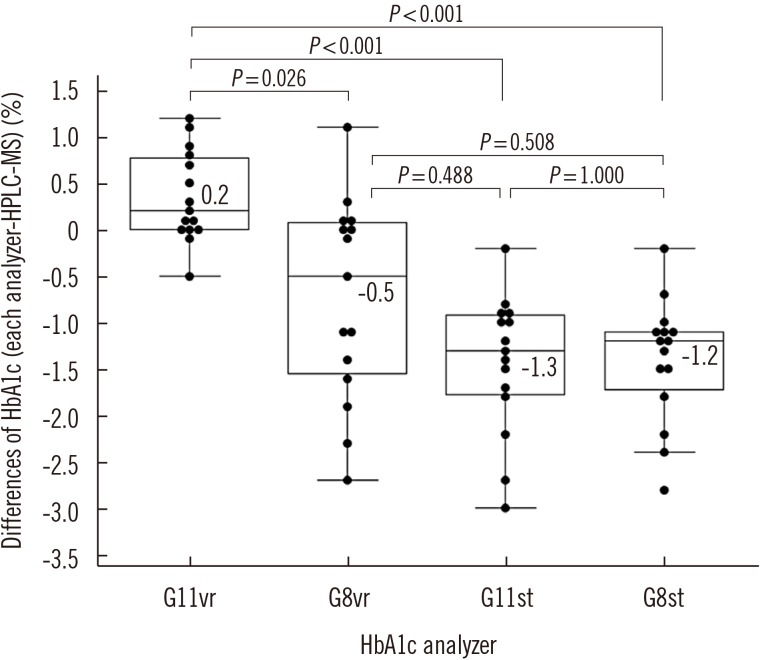
Fig. 3
Chromatograms of the three samples with known Hb-variant. The black part in the chromatogram represents the HbA1c region. (A) Sample B-4 (Hb G-Coushatta): (B) Sample B-8 (Hb G-Coushatta): (C) Sample B-9 (Hb Queens [α]).
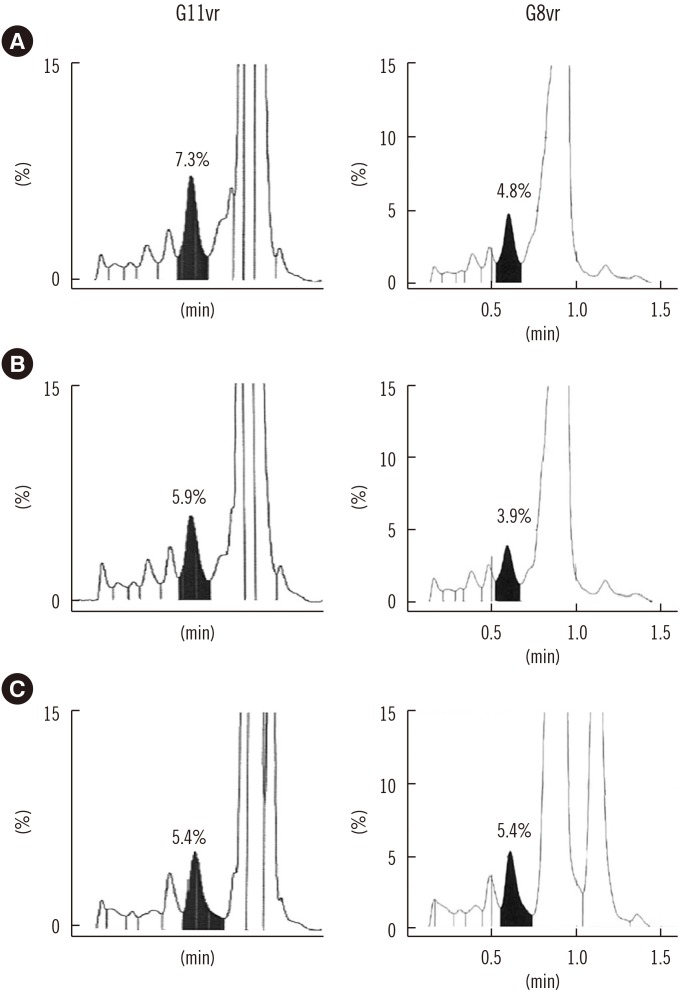
Fig. 4
Turnaround times from sample mounting to result reporting. Turnaround times for one sample (A), 10 samples (B), and 30 samples (C) on the different analyzers. No flagged sample was detected.
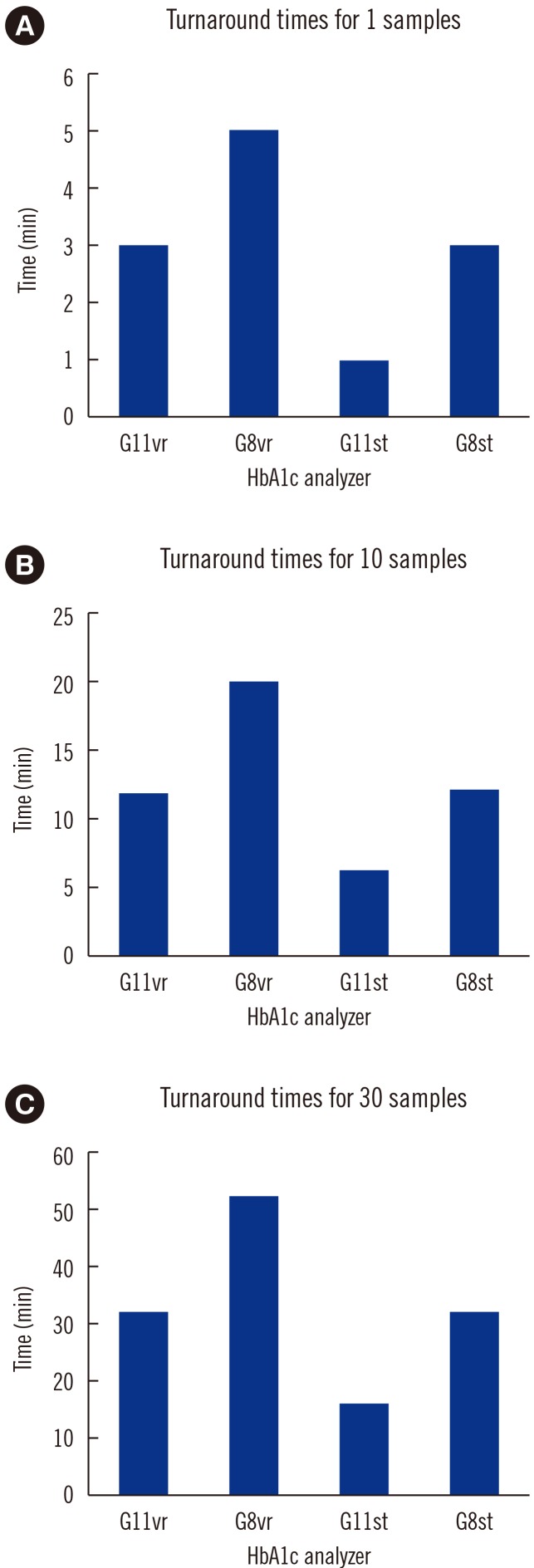
Table 1
Comparison of HbA1c concentrations in six samples with Hb variants
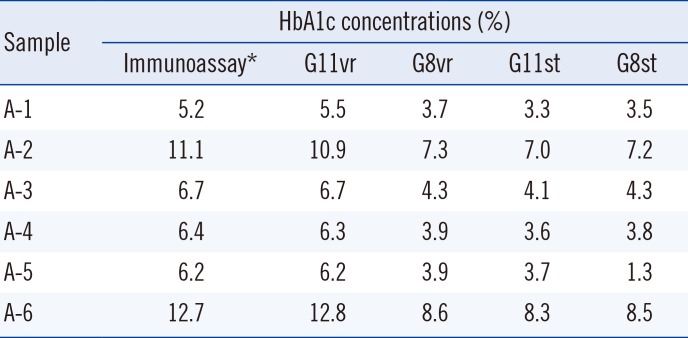
*Cobas Integra 800 (Roche Diagnostics, Basel, Switzerland).
Abbreviations: HbA1c, glycated Hb; G11vr, HLC-723 G11 Variant Mode (Tosoh Bioscience, Inc., Tokyo, Japan); G8vr, HLC-723 G8 Variant Mode (Tosoh Bioscience); G11st, HLC-723 G11 Standard Mode (Tosoh Bioscience); G8st, HLC-723 G8 Standard Mode (Tosoh Bioscience).
Table 2
HbA1c concentrations by HPLC-MS, capillary electrophoresis (CE), and HPLC analyzers
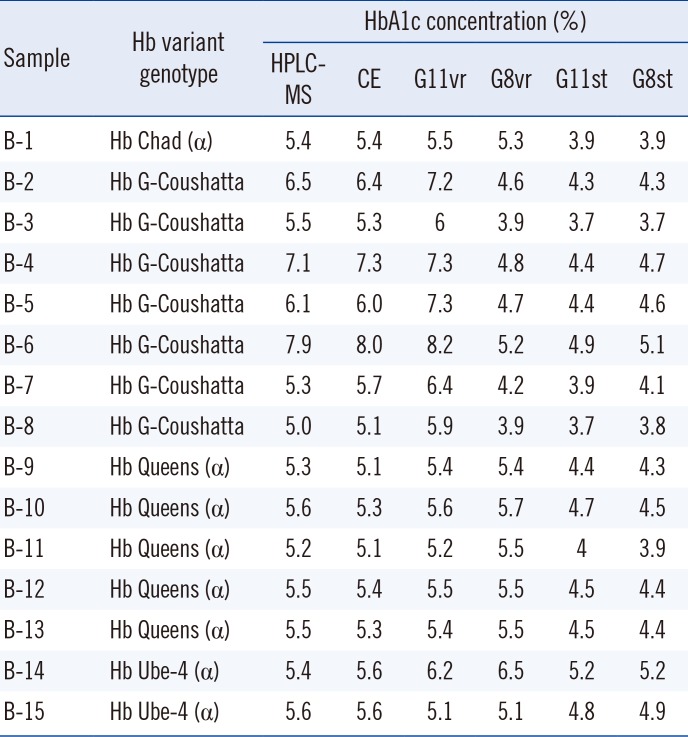
Abbreviations: HbA1c, glycated Hb; HPLC-MS, high-performance liquid chromatography-mass spectrometry (Shimadzu Nexera X2 UPLC; Shimadzu Co., Kyoto, Japan, and AB SCIEX 6500 Triple Quad, AB SCIEX, Framingham, MA, USA); CE, capillary electrophoresis [Sebia Capillarys 2 Flex Piercing Hemoglobin(E) kit (Sebia, Lisse, France)]; G11vr, HLC-723 G11 Variant Mode (Tosoh Bioscience, Inc., Tokyo, Japan); G8vr, HLC-723 G8 Variant Mode (Tosoh Bioscience); G11st, HLC-723 G11 Standard Mode (Tosoh Bioscience); G8st, HLC-723 G8 Standard Mode (Tosoh Bioscience).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download