1. Lee CR, Lee JH, Park KS, Kim YB, Jeong BC, Lee SH. Global dissemination of carbapenemase-producing
Klebsiella pneumoniae: epidemiology, genetic Context, treatment options, and detection methods. Front Microbiol. 2016; 7:895. PMID:
27379038.
2. Chen YT, Lin JC, Fung CP, Lu PL, Chuang YC, Wu TL, et al. KPC-2-encoding plasmids from
Escherichia coli and
Klebsiella pneumoniae in Taiwan. J Antimicrob Chemother. 2014; 69:628–631. PMID:
24123430.
3. Adler A, Miller-Roll T, Assous MV, Geffen Y, Paikin S, Schwartz D, et al. A multicenter study of the clonal structure and resistance mechanism of KPC-producing
Escherichia coli isolates in Israel. Clin Microbiol Infect. 2015; 21:230–235. PMID:
25658543.
4. Piazza A, Caltagirone M, Bitar I, Nucleo E, Spalla M, Fogato E, et al. Emergence of
Escherichia coli Sequence Type 131 (ST131) and ST3948 with KPC-2, KPC-3 and KPC-8 carbapenemases from a Long-Term Care and Rehabilitation Facility (LTCRF) in Northern Italy. Adv Exp Med Biol. 2016; 901:77–89. PMID:
26810233.
5. Chavda KD, Chen L, Jacobs MR, Bonomo RA, Kreiswirth BN. Molecular diversity and plasmid analysis of KPC-producing
Escherichia coli. Antimicrob Agents Chemother. 2016; 60:4073–4081. PMID:
27114279.
6. Xu G, Jiang Y, An W, Wang H, Zhang X. Emergence of KPC-2-producing
Escherichia coli isolates in an urban river in Harbin, China. World J Microbiol Biotechnol. 2015; 31:1443–1450. PMID:
26149956.
7. Johnson TJ, Bielak EM, Fortini D, Hansen LH, Hasman H, Debroy C, et al. Expansion of the IncX plasmid family for improved identification and typing of novel plasmids in drug-resistant
Enterobacteriaceae. Plasmid. 2012; 68:43–50. PMID:
22470007.
8. He S, Chandler M, Varani AM, Hickman AB, Dekker JP, Dyda F. Mechanisms of evolution in high-consequence drug resistance plasmids. MBio. 2016; 7:e01987–e01916. PMID:
27923922.
9. Naas T, Cuzon G, Villegas MV, Lartigue MF, Quinn JP, Nordmann P. Genetic structures at the origin of acquisition of the β-lactamase
blaKPC gene. Antimicrob Agents Chemother. 2008; 52:1257–1263. PMID:
18227185.
10. Naas T, Cuzon G, Truong HV, Nordmann P. Role of IS
Kpn7 and deletions in
blaKPC gene expression. Antimicrob Agents Chemother. 2012; 56:4753–4759. PMID:
22733068.
11. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Twenty-sixth informational supplement, M100-S26. Wayne, PA: National Committee for Clinical Laboratory Standards;2016.
12. Kim MN, Yong D, An D, Chung HS, Woo JH, Lee K, et al. Nosocomial clustering of NDM-1-producing
Klebsiella pneumoniae sequence type 340 strains in four patients at a South Korean tertiary care hospital. J Clin Microbiol. 2012; 50:1433–1436. PMID:
22259206.
13. Chen L, Mediavilla JR, Endimiani A, Rosenthal ME, Zhao Y, Bonomo RA, et al. Multiplex real-time PCR assay for detection and classification of
Klebsiella pneumoniae carbapenemase gene (
blaKPC) variants. J Clin Microbiol. 2011; 49:579–585. PMID:
21123529.
14. Jeong S, Kim JO, Jeong SH, Bae IK, Song W. Evaluation of peptide nucleic acid-mediated multiplex real-time PCR kits for rapid detection of carbapenemase genes in gram-negative clinical isolates. J Microbiol Methods. 2015; 113:4–9. PMID:
25819308.
15. Jeong SH, Lee KM, Lee J, Bae IK, Kim JS, Kim HS, et al. Clonal and horizontal spread of the
blaOXA-232 gene among
Enterobacteriaceae in a Korean hospital. Diagn Microbiol Infect Dis. 2015; 82:70–72. PMID:
25702524.
16. Harada K, Nakai Y, Kataoka Y. Mechanisms of resistance to cephalosporin and emergence of O25b-ST131 clone harboring CTX-M-27 β-lactamase in extraintestinal pathogenic
Escherichia coli from dogs and cats in Japan. Microbiol Immunol. 2012; 56:480–485. PMID:
22486529.
17. O'Hara JA, Hu F, Ahn C, Nelson J, Rivera JI, Pasculle AW, et al. Molecular epidemiology of KPC-producing
Escherichia coli: occurrence of ST131-fimH30 subclone harboring pKpQIL-like IncFIIk plasmid. Antimicrob Agents Chemother. 2014; 58:4234–4237. PMID:
24820082.
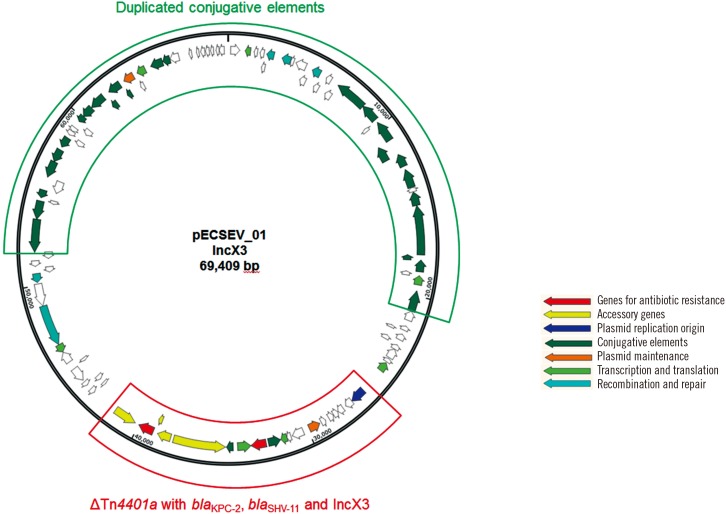
18. Kim JO, Song SA, Yoon EJ, Shin JH, Lee H, Jeong SH, et al. Outbreak of KPC-2-producing
Enterobacteriaceae caused by clonal dissemination of
Klebsiella pneumoniae ST307 carrying an IncX3-type plasmid harboring a truncated Tn
4401a. Diagn Microbiol Infect Dis. 2017; 87:343–348. PMID:
28185686.
19. Kassis-Chikhani N, Frangeul L, Drieux L, Sengelin C, Jarlier V, Brisse S, et al. Complete nucleotide sequence of the first KPC-2- and SHV-12-encoding IncX plasmid, pKpS90, from
Klebsiella pneumoniae. Antimicrob Agents Chemother. 2013; 57:618–620. PMID:
23089759.
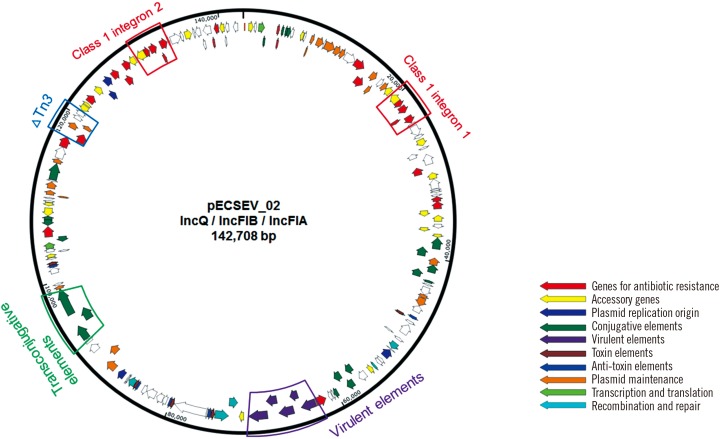
20. Plante I, Centrón D, Roy PH. Direct sequencing and PCR mapping of integrons reveals multiple class 1 integrons in the multiresistant strain
Enterobacter cloacae SCH88040794. FEMS Microbiol Lett. 2003; 221:59–62. PMID:
12694911.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download