Dear Editor,
Several antibiotics are currently used for meningococcal prophylaxis, including ciprofloxacin, rifampin, and ceftriaxone. Ciprofloxacin, a fluoroquinolone, is often used in adults because of its convenient single-dose regimen. In contrast to an emerging trend worldwide, ciprofloxacin-resistant Neisseria meningitidis has not been reported in Korea [12]. We report the first instance of septicemia caused by meningococcus with decreased ciprofloxacin susceptibility in Korea.
A 20-yr-old female was admitted to the hospital with fever, rhinorrhea, sputum, and myalgia that started 24 hr before admission. The patient's initial vital signs included a temperature of 38.3℃, a blood pressure of 91/76 mm Hg, a pulse rate of 95 beats/min, and a respiratory rate of 20 breaths/min. Physical examination revealed a pinkish rash on the lower extremities. Laboratory testing showed a white blood cell (WBC) count of 7.5×109/L (70% neutrophils) and C-reactive protein levels of 10.98 mg/dL. We suspected an infectious disease with severe sepsis, and ceftriaxone was injected intravenously. About six hours later, the rash turned into multiple petechial lesions, sized from 1 mm to 5 mm, and was purpuric and non-blanching; a meningococcal infection was suspected. She was moved to the intensive care unit (ICU) and quarantined. She complained about a severe headache as well. Cerebrospinal fluid (CSF) analysis for the differential diagnosis of meningitis showed a WBC count of 16×106/L (18% polymorphonuclear neutrophils and 70% monocytes), a red blood cell (RBC) count of 3×106/L, and glucose and protein levels of 81 and 43 mg/dL, respectively.
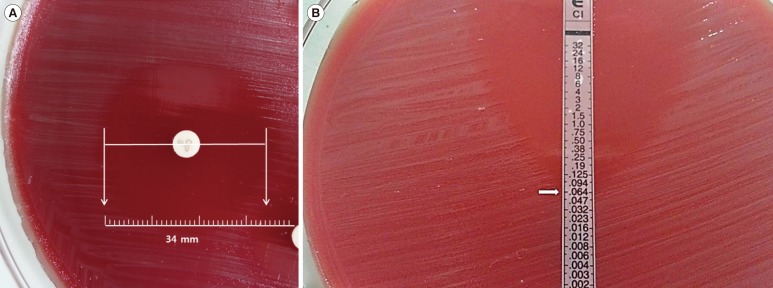
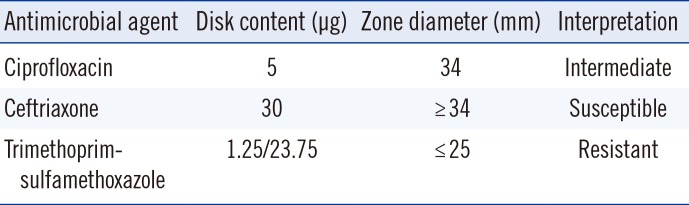
Blood culture showed gram-negative diplococci after two days of incubation. On the fourth day of hospitalization, the isolate was identified as N. meningitidis by using VITEK 2 system (bio-Mérieux, Marcy l'Etoile, France). Ciprofloxacin, ceftriaxone, and trimethoprim-sulfamethoxazole susceptibility testing was performed by using the disk diffusion method according to the CLSI guidelines [2]. Test results are shown in Table 1; ciprofloxacin susceptibility was intermediate with a zone diameter of 34 mm (Fig. 1A). We confirmed the minimum inhibitory concentration (MIC) via E-test (AB Biodisk, Solna, Sweden). Our results indicated an intermediate susceptibility of the isolate to ciprofloxacin at 0.06 µg/mL (Fig. 1B). Serogrouping by PCR was performed as described previously [3]. The crgA gene was used to identify N. meningitidis, while the orf-2 gene (serogroup A) and the siaD gene (serogroups B, C, Y, and W135) were used for serogroup prediction. PCR indicated this isolate belonged to serogroup B.
Before the drug susceptibility results were available, the patient's close contacts received ciprofloxacin chemoprophylaxis. However, because the results indicated decreased ciprofloxacin susceptibility, chemoprophylaxis was repeated by using a single 250 mg intravenous dose of ceftriaxone.
Clinical guidelines for the management of bacterial meningitis in adults in Korea recommend rifampin, ciprofloxacin, and ceftriaxone for meningococcal chemoprophylaxis of close contacts [4]. Rifampin, ciprofloxacin, and ceftriaxone are 90-95% effective in reducing the nasopharyngeal carriage of N. meningitidis and are considered acceptable antimicrobial drugs for chemoprophylaxis [5].
However, N. meningitidis has developed a resistance against several penicillin and chloramphenicol agents used in chemoprophylaxis. Similarly, sulfonamides and tetracycline can no longer be used for this purpose. Rifampin has been licensed for meningococcal chemoprophylaxis, so has been the drug of choice. However, rifampin-resistant N. meningitidis has been reported, and cases of rifampin-resistant N. meningitidis infection, although rare, have been associated with chemoprophylaxis failure [6].
Ciprofloxacin is used for prophylaxis treatment of large numbers of close-contact individuals, such as military personnel or students residing in dormitories. As opposed to rifampin, ciprofloxacin is administered as a single dose and does not interact with oral contraceptives. Ciprofloxacin is also more readily available. In addition, reports of ciprofloxacin-resistant N. meningitidis are rare. There has been one report about the antimicrobial susceptibility of N. meningitidis isolates in Korea, and all 11 meningococcal isolates from 2002 to 2003 were susceptible to ciprofloxacin, rifampin, and cefotaxime [1].
However, the use of fluoroquinolones, one of the most commonly prescribed classes of broad-spectrum antibiotics, probably facilitated the emergence of ciprofloxacin-resistant strains. Chemoprophylaxis failure is possible even with ciprofloxacin. Recently, decreased ciprofloxacin susceptibility has been reported in France, Australia, Spain, India, Hong Kong, and the United States [7]. In those cases, a second chemoprophylaxis treatment other than ciprofloxacin was administered to close contacts. To our knowledge, this is the first reported case of meningococcus having decreased ciprofloxacin susceptibility in Korea.
References
1. Bae SM, Kang YH. Serological and genetic characterization of meningococcal isolates in Korea. Jpn J Infect Dis. 2008; 61:434–437. PMID: 19050348.
2. Clinical and Laboratory Standard Institute. Performance standard for antimicrobial susceptibility testing. Twenty-second Informational supplement, Document M100-S22. Wayne, PA: Clinical and Laboratory Standards Institute;2012.
3. Taha MK. Simultaneous approach for nonculture PCR-based identification and serogroup prediction of Neisseria meningitidis. J Clin Microbiol. 2000; 38:855–857. PMID: 10655397.
4. The Korean Society of Infectious Diseases. The Korean Society for Chemotherapy. The Korean Neurological Association. The Korean Neurosurgical Society. The Korean Society of Clinical Microbiology. Clinical practice guidelines for the management of bacterial meningitis in adults in Korea. Infect Chemother. 2012; 44:140–163.
5. Gaunt PN, Lambert BE. Single dose ciprofloxacin for the eradication of pharyngeal carriage of Neisseria meningitidis. J Antimicrob Chemother. 1988; 21:489–496. PMID: 3132442.

6. Mounchetrou Njoya I, Deghmane AE, Taha MK, Isnard H, Parent du Châtelet I. A cluster of meningococcal disease caused by rifampicin-resistant C meningococci in France, April 2012. Euro Surveill. 2012; 17:pii=20254.

7. Wu HM, Harcourt BH, Hatcher CP, Wei SC, Novak RT, Wang X, et al. Emergence of ciprofloxacin-resistant Neisseria meningitidis in North America. N Engl J Med. 2009; 360:886–892. PMID: 19246360.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download