Abstract
Purpose
Endoscopic thyroidectomy using a cervico-axillary approach (CAA) provides optimal visualization with a smaller dissection plane. Despite the excellent cosmetic results and high patient satisfaction, the surgical and oncologic safety of CAA endoscopic surgery has not been fully established. The present study evaluated the feasibility, safety, and surgical outcomes of CAA endoscopic thyroidectomy.
Methods
From October 2009 to April 2012, 100 patients with papillary thyroid cancer underwent CAA endoscopic thyroidectomy. Patient demographics, pathologic features, and surgical outcomes including complications and recurrence were collected.
Results
CAA endoscopic thyroidectomy was successful in all patients, and none required conversion to open thyroidectomy. All patients underwent ipsilateral thyroid lobectomy with or without central compartment neck dissection. The mean tumor size was 1.0±0.6 cm (range, 0.5~1.6), and 35.0% of tumors showed extrathyroidal extension. The mean number of harvested lymph nodes was 4.1±4.4, and metastasis was found in 12.0% of patients. The mean surgical time was 175.2±50.4 min, mean intraoperative blood loss was 42.5±69.2 ml, and the mean hospital stay was 3.3±0.6 days. There were five cases of postoperative transient hypocalcemia and eight cases of vocal cord palsy. No permanent complication or postoperative bleeding was observed. Patients continued to be seen for a median period of 63.7 months, and no recurrence of thyroid cancer was seen.
The incidence of thyroid cancer has increased worldwide in the last two decades.(1) The National Cancer Information Center of Korea indicates that thyroid cancer is the most common cancer since 2009 and estimates 42,541 new cases in 2013.(2) Conventional open thyroidectomy is the treatment of choice for thyroid cancer; however, it may leave an undesirable scar in a highly visible area.(3) As the prognosis of thyroid cancer is excellent and most patients are young women, cosmetic issues are a concern for many patients.(4) Scarring can further decrease quality of life, and therefore considerable efforts have been made to minimize neck scars, including the development of endoscopic procedures.(56)
The first endoscopic neck surgery was described by Gagner(7) in 1996. After Huscher et al.(8) introduced endoscopic thyroid surgery in 1997, endoscopic procedures using various approaches have been developed. Endoscopic procedures offer many advantages including excellent cosmetic outcomes, magnified operative view, and decreased postoperative swallowing difficulties; therefore, endoscopic surgery is considered a good treatment option for benign thyroid disease.(3) In 2001, Miccoli et al.(9) performed endoscopic thyroidectomy for low-risk papillary thyroid carcinoma. To date, many pioneers have shown the safety and feasibility of endoscopic thyroid surgery for cancer.(41011)
We reported our initial experience with endoscopic thyroidectomy using a cervical approach in 2002.(12) After several cases of endoscopic thyroidectomy using a cervical approach, we developed the cervico-axillary approach (CAA) to obtain optimal visualization with a smaller dissection plane.(13) Despite the excellent cosmetic results and high patient satisfaction of CAA endoscopic thyroidectomy, the surgical and oncologic safety of CAA endoscopic surgery has not been fully established.(14) The aim of the present study was to evaluate the feasibility, safety, and surgical outcomes of CAA endoscopic thyroidectomy.
The institutional review board approved this study. One hundred patients with thyroid cancer underwent endoscopic thyroidectomy at a single hospital between October 2009 and April 2012. The indications of endoscopic thyroidectomy were as follows: (1) well-differentiated thyroid cancer without aggressive histology; (2) tumor size <2 cm; (3) absence of gross invasion to the adjacent tissue; and (4) no evidence of cervical lymph node metastasis by physical examination or image studies including ultrasonography and computed tomography. Informed consent was obtained from each patient. All patients chose this endoscopic procedure for cosmetic reasons.
The surgical technique of CAA endoscopic thyroidectomy was previously described.(13) In brief, the patient was placed in the supine position under general anesthesia. The neck was extended and the skin was prepared using routine procedures. A 2 cm-long skin incision was made in the axilla. Dissection was performed along the lateral border and above the fascia of the pectoralis major and deepened toward the neck over the clavicle. A 15 mm trocar for endoscopy was inserted and fixed at the axillary incision. Three trocars (5 mm) were inserted in the lateral neck, circumareolar area, and lateral chest wall (Fig. 1). After insufflation of carbon dioxide gas, the medial belly of the sternocleidomastoid muscle and the strap muscles were dissected and elevated with a tagging suture. The capsule of the thyroid lobe was dissected sharply using an endoscopic hook and ultrasonic shears. The superior and inferior thyroid arteries were identified and ligated with ultrasonic shears after detection of the recurrent laryngeal nerve (RLN). The ipsilateral thyroid lobe and isthmic portion were detached from the trachea and resected. When microscopic extrathyroidal extension was suspected, ipsilateral prophylactic central node dissection was performed. The specimen was placed in an endopouch and removed through the axillary wound (Fig. 2). A closed suction drain was placed on the side of the tumor, and the wounds were closed (Fig. 3).
The vocal cords were examined using direct laryngoscopy 2 weeks after surgery. RLN injury was defined as a postoperative laryngoscopic impairment of the motility of the vocal cords. Permanent RLN injury was defined as persistent impairment of vocal cord motility at 6 months after surgery; otherwise, it was considered transient. Serum levels of calcium, phosphorus, and ionized calcium were measured on postoperative day 1. Postoperative transient hypocalcemia was defined as a total serum calcium level lower than 8.0 mg/dl with symptoms of hypocalcemia. Hypopcalcemia was considered permanent in patients who required calcium and/or vitamin D supplementation for longer than 6 months after surgery.
All patients were followed up at 2 weeks, 3 months, 6 months, and annually thereafter. Patients were treated with levothyroxine for suppression of thyroid-stimulating hormone. Follow-up tests included clinical examinations for hypocalcemia, vocal cord motility, and a thyroid function test including thyroglobulin and thyroglobulin antibody. Ultrasonography for the detection of recurrence was performed annually. In cases where vocal cord injury was noted in the previous follow-up, the vocal cord was re-examined. In cases where hypocalcemia was noted in the previous examination, serum levels of calcium, phosphorus, and parathyroid hormone were also measured.
CAA endoscopic thyroidectomy was successful in all patients, and none required conversion to open thyroidectomy. All patients underwent ipsilateral thyroid lobectomy with or without central compartment neck dissection (Table 1). The mean age of the patients was 38.1±7.7 years (range, 23~61). The mean tumor size was 1.0±0.6 cm (range, 0.5~1.6). The ratio of minimal extrathyroidal extension was 35.0%. Twelve patients (12.0%) showed lymph node metastasis. The median follow-up period was 63.7 months (range, 0.7~88.4).
The data presented in Table 2 show the surgical outcomes of CAA endoscopic thyroidectomy. The mean operation time, defined as the time from skin incision to skin closure was 175.2±50.4 min. Blood loss was 42.5± 69.2 ml. The mean number of harvested LNs was 4.1±4.4. The mean hospital stay was 3.3±0.6 days. Postoperative transient hypocalcemia occurred in five patients (5.0%). All patients recovered from hypocalcemic symptoms at discharge. Laryngoscopic examination revealed that eight patients (8.0%) had unilateral vocal cord palsy, including three cases of hoarseness. After 3 months, the hoarseness improved in all patients, and no patient showed vocal cord palsy on laryngoscopic examination. There was no recurrence of thyroid cancer among the patients.
The present study showed that CAA endoscopic thyroidectomy can be safely performed in selected patients with thyroid cancer. Various endoscopic thyroidectomy techniques have been developed worldwide, including the transaxillary approach (TAA), bilateral axillo-breast approach (BABA), cervical approach, and transoral approach.(151617) The advantages of an endoscopic approach, such as a magnified view of thyroid anatomy and enhanced lighting of the operative field, enabled the early adoption and spread of endoscopic thyroidectomy. In Korea, TAA and BABA are the most popular endoscopic thyroid surgery procedures and over 1,000 cases have been reported.(18) Although these techniques show excellent surgical and cosmetic outcomes, the wide dissection plane remains a concern.(19)
In 2009, the CAA technique was developed to reduce the dissection plane, resulting in a less invasive procedure.(13) CAA endoscopic thyroidectomy minimizes muscle dissection for establishing a working space, which can reduce the risk of postoperative bleeding or discharge.(14) A smaller dissection plane also reduces postoperative pain and discomfort. Another advantage of CAA endoscopic thyroidectomy is that it provides an excellent surgical view and convenient manipulation of instruments. In the CAA procedure, the cervical compartment is adequately exposed using a tagging suture. This maneuver opens a larger space with a smaller dissection, resulting in better preservation of the RLN and parathyroid glands.
Endoscopic thyroidectomy is mainly used for the treatment of benign thyroid disease, and it is feasible for selected patients with thyroid cancer.(3) However, there is a debate regarding its surgical indications, including tumor size for endoscopic thyroidectomy. In a survey performed in Korea, 36.4% of surgeons reported performing endoscopic thyroidectomy for benign thyroid nodules with no size limit, whereas 36.4% responded that it is safe for thyroid nodules of up to 5 cm.(18) In thyroid cancer, 76.2% of experts responded that the procedure was appropriate for thyroid tumors smaller than 2 cm. This is partly because papillary thyroid tumors larger than 2 cm are associated with extensive lymph node metastasis and require meticulous dissection.(2021) In our group, CAA endoscopic thyroidectomy is applied for patients with thyroid carcinoma smaller than 2 cm.
Postoperative complications are an important factor for determining the safety and feasibility of a new surgical procedure. The incidence of transient hypocalcemia and RLN palsy was 5.0% and 8.0%, respectively, after CAA endoscopic thyroidectomy. There were no cases of permanent hypocalcemia and RLN palsy. A recent meta-analysis demonstrated that transient hypocalcemia and RLN palsy occurred in 0~25.2% and 8.6~31.4% of endoscopic thyroidectomies, respectively.(22) The reported incidence of transient hypocalcemia after open surgery also ranges from 10% to 15% and that of transient RLN palsy ranges from 0% to 15.4%.(23) Our present results were comparable with those of previous reports.
Recurrence is another issue in endoscopic thyroidectomy. Recurrence along the surgical access points after endoscopic or robotic thyroidectomy is an issue of concern.(2425) However, there are few reports on the recurrence rate after endoscopic thyroidectomy. In TAA endoscopic thyroidectomy, 2.7% (1/37) of patients experienced recurrence after 54.3 months of median follow-up.(11) Choi et al. reported a rate of recurrence of 2.0% (8/397) after 39.3 months in patients who underwent BABA endoscopic surgery for thyroid cancer.(4) The mortality rate was not reported in these studies. In the present study, no cases of recurrence were reported among 100 patients with a median follow-up of 63.7 months. Although the strict selection criteria of low-risk patients for endoscopic surgery may be one reason for this low recurrence rate, our data support the safety of CAA endoscopic thyroidectomy.
The present study has several limitations. First, as all patients underwent thyroid lobectomy, the rate of hypoparathyroidism may have been underestimated. Although the superior and inferior parathyroid glands were detected and saved in the operation video, and pathologic examination of specimens showed no parathyroid glands, transient hypoparathyroidism caused by ischemic change was not appropriately evaluated. Second, the number of patients and follow-up period may have been insufficient to determine the long-term prognosis. As the indications for endoscopic thyroidectomy were restricted to patients with low-risk thyroid cancer, the median follow-up period of 63.7 months was relatively short. Third, we did not include the candidates for subtotal or total endoscopic thyroidectomy in the present study. Although our initial successful experience with CAA endoscopic thyroid lobectomy led us to perform total thyroidectomy and expand the operative indications, the advantage of CAA endoscopic thyroidectomy including smaller dissection plane can be hampered by more extensive surgery. Further investigation to address the indications and long-term prognosis of CAA endoscopic thyroidectomy is warranted.
In conclusion, CAA endoscopic thyroidectomy is a feasible and safe procedure for low-risk thyroid cancer, with excellent cosmesis. It can be recommended as an alternative option for selected patients with low-risk thyroid cancer.
Figures and Tables
Table 1
Patient demographics and pathologic features
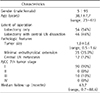
Table 2
Surgical and oncologic outcomes of CAA endoscopic thyroid lobectomy

References
1. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.

2. Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of Cancer Incidence and Mortality in Korea, 2016. Cancer Res Treat. 2016; 48:451–457.

3. Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, et al. Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg. 2011; 253:1060–1066.
4. Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, et al. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc. 2012; 26:948–955.

5. Lee S, Kim HY, Lee CR, Park S, Son H, Kang SW, et al. A prospective comparison of patient body image after robotic thyroidectomy and conventional open thyroidectomy in patients with papillary thyroid carcinoma. Surgery. 2014; 156:117–125.

6. Lee J, Kwon IS, Bae EH, Chung WY. Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab. 2013; 98:2701–2708.

7. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; 83:875.

8. Huscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc. 1997; 11:877.

9. Miccoli P, Berti P, Raffaelli M, Conte M, Materazzi G, Galleri D. Minimally invasive video-assisted thyroidectomy. Am J Surg. 2001; 181:567–570.

10. Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, et al. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol. 2009; 100:477–480.

11. Lee H, Lee J, Sung KY. Comparative study comparing endoscopic thyroidectomy using the axillary approach and open thyroidectomy for papillary thyroid microcarcinoma. World J Surg Oncol. 2012; 10:269.

12. Moon BI, Yi NJ. Supraclavicular endoscopic thyroidectomy. J Minim Invasive Surg. 2002; 5:175–180.
13. Lee A, Jang J, Lim W, Moon BI. Comparison of endoscopic thyroidectomy versus conventional thyroidectomy in patient satisfaction with cosmestic result. Korean J Endocr Surg. 2010; 10:170–175.

14. Park YM, Lim WS, Moon BI. Comparison study endoscopic thyroidectomy versus robot-assisted thyroidectomy by a cervico-transaxillary approach. Korean J Endocr Surg. 2012; 12:264–270.

15. Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg. 2007; 31:601–606.

16. Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J. Endoscopic thyroidectomy by the axillary approach. Surg Endosc. 2001; 15:1362–1364.

17. Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008; 22:1871–1875.

18. Park KN, Cho SH, Lee SW. Nationwide multicenter survey for current status of endoscopic thyroidectomy in Korea. Clin Exp Otorhinolaryngol. 2015; 8:149–154.

19. Inabnet WB 3rd. Robotic thyroidectomy: must we drive a luxury sedan to arrive at our destination safely? Thyroid. 2012; 22:988–990.

20. Ito Y, Fukushima M, Higashiyama T, Kihara M, Takamura Y, Kobayashi K, et al. Tumor size is the strongest predictor of microscopic lymph node metastasis and lymph node recurrence of N0 papillary thyroid carcinoma. Endocr J. 2013; 60:113–117.

21. Chai YJ, Suh H, Woo JW, Yu HW, Song RY, Kwon H, et al. Surgical safety and oncological completeness of robotic thyroidectomy for thyroid carcinoma larger than 2 cm. Surg Endosc. 2016; in press.
22. Li Y, Zhou X. Comparison between endoscopic thyroidectomy and conventional open thyroidectomy for papillary thyroid microcarcinoma: a meta-analysis. J Cancer Res Ther. 2016; 12:550–555.

23. Randolph GW. Surgery of the thyroid and parathyroid glands. 2nd ed. Philadelphia: Elsevier Saunders;2013.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download