Abstract
We report a rare case of arachnoid granulations mimicking multiple osteolytic bone lesions. A 66-yearold woman was admitted to a local clinic for a regular checkup. Upon admission, brain CT showed multiple osteolytic lesions in the occipital bone. These needed to be differentiated from multiple osteolytic bone tumor. Subsequent brain MRI revealed that the osteolytic lesions were isointense to cerebrospinal fluid, hyperintense on T2-weighted image, hypointense on T1-weighted image, and with subtle capsules around the osteolytic lesions that were visible after gadolinium injection. A bone scan revealed no radiotracer uptake. The lesions were in both the transverse sinuses and the torcular herophili. With typical radiological appearances of the lesions, the osteolytic lesions were diagnosed as multiple arachnoid granulations. No further treatment was planned. A 1-year follow-up brain CT scan revealed no change. We should consider the possibility of arachnoid granulations when multiple osteolytic lesions are observed in the occipital bone.
Arachnoid granulations are growths of the arachnoid membrane into the dual sinuses that absorb cerebrospinal fluid (CSF) and drain it into the venous system [1]. Their corresponding lesions are usually located in the parasagittal area along the superior sagittal sinus, and occasionally at the transverse sinus. When the lesions grow beyond the inner table of the skull and involve the outer table, osteolytic lesions can be mistaken for tumorous lesions such as multiple myelomas, metastases, hemanigomas, dermoids, or epidermoids [234]. The accurate diagnosis of normal arachnoid granulations through radiologic findings may reduce rates of false diagnosis and unnecessary surgical biopsies.
We report a rare case of normal arachnoid granulations mimicking multiple osteolytic bone lesions in the occipital bone.
A 66-year-old woman was referred to our hospital for surgical treatment from a local clinic with a diagnosis of malignant bone tumors. She had originally visited the clinic for a regular checkup. She had been initially diagnosed with malignant bone tumors in the occipital bone, such as multiple myeloma and metastases. She had no symptoms of headache before admission. Laboratory and neurological examinations showed no significant findings. An X-ray examination of the skull revealed multiple osteolytic lesions in the middle as well as in both lateral parts of the occipital bone without apparent sclerotic margins (Fig. 1). Brain CT from a local clinic revealed multiple 2 mm to 19 mm osteolytic lesions in the occipital bone around both the transverse sinuses and the torcular herophili, with sharp margins and no calcifications (Fig. 2). The lesions involved both the inner and outer bone tables. The osteolytic lesions should be differentiated from tumorous lesion like multiple myelomas, bone metastases, hemangiomas, dermoids, and epidermoids. Subsequently, brain MRI revealed that the osteolytic lesions were isointense to CSF, hyperintense on T2-weighted image, hypointense on T1-weighted image, and with subtle capsules around the osteolytic lesions that were visible after gadolinium injection (Fig. 3). Fluid attenuated inversion recovery imaging showed complete suppression and diffusion-weighted imaging (DWI) showed no restricted diffusion. Laboratory examination revealed no evidence for the presence of multiple myelomas such as Bence-Jones protein and excretion of immunoglobulin elements. Chest-abdomen-pelvis CT revealed no evidence of primary tumor of metastases. A whole body bone scan with 99mTc-hydroxy diphosphonate (HDP) showed no increased radiotracer uptake (Fig. 4). With typical radiological appearances of the lesions, the osteolytic lesions were diagnosed as multiple arachnoid granulations. No further treatment was planned. A 1-year follow-up brain CT scan revealed no change. The patient provided written informed consent for this study.
Arachnoid granulations are growths of the arachnoid membrane into the dural sinuses that increase in number and enlarge with age, probably due to CSF pressure [1]. They are known to be involved in the absorption and drainage of CSF. Arachnoid granulations occur close to the venous sinuses near the superior sagittal sinus, where there is a weakness of the dural mater. They can be mistakenly regarded as arachnoid herniations secondary to CSF pulsation through dural defects into the sinus [5]. Most of the arachnoid granulations were indentified in the superior sagittal sinus and transverse sinus [46]. Giant arachnoid granulations have also been reported in the transverse sinus, which is far from the midline [47]. The role of arachnoid granulations in the posterior fossa remains unclear. Arachnoid granulations are indentified as impressions on the inner table of the skull. They sometimes grow beyond the inner table of the skull and expand into the diploic space and finally involve the outer table, mimicking osteolytic lesions [2]. As in our case, this is not easy to distinguish from multiple osteolytic bone tumors. However, arachnoid granulations are commonly differentiated from other diseases by indentifying intra-arachnoid granulation fluid isoattenuated to CSF on all sequences. Arachnoid granulations typically range from 2 mm to 8 mm in size but may grow with age [4]. The transverse diameters of the bone defects in our patient ranged from 2 mm to 19 mm, involving both the inner and outer tables. Giant arachnoid granulations ranging from 10 mm to 19 mm have recently been reported [6].
Multiple osteolytic lesions in the skull are likely to be mistaken for malignant disease. Discussing the typical radiological findings of arachnoid granulations are of great help in differentiating arachnoid granulations from other diseases, which can reduce unnecessary examinations such as surgical biopsies. In our case, arachnoid granulations are well-demarcated ovoid shape. Haroun et al. [8] suggested that the identification of arachnoid granulations could be facilitated by their characteristic appearance: round or oval shape, well-defined outlines, and homogenous intensity. Trimble et al. [4] suggested that the conventional diagnostic criterion for arachnoid granulations have included CSF-like attenuation on brain CT or fluid that parallels all MR images. Many osteolytic diseases such as multiple myelomas, metastases, meningiomas, arachnoid cysts, dermoids, epidermoids, and hemangiomas are included in differential diagnosis. Arachnoid granulations do not enhance strongly and uniformly like typical neoplasms do, differentiating them from multiple myelomas, metastases, and meningiomas. Arachnoid granulations also do not have MR signal intensities like fat, differentiating them from dermoids and hemangiomas. In DWI, all arachnoid granulations were isointense signals, which was higher than those of arachnoid cysts and lower than those of epidermoids [69]. Arachnoid granulations mainly involve the inner table, while a few cases may involve the outer table. Dermoids and epidermoids often involve both the inner and outer tables, and hemangiomas are mainly located in the intradiploic space [7]. In our study, a bone scan with 99mTc-HDP demonstrated hypovascularity and low metabolic activity in arachnoid granulations as a way to help distinguish them from other diseases [10].
As was the case in our patient, asymptomatic arachnoid granulations incidentally found do not require treatment. However, arachnoid granulations can grow to fill and dilate the dural sinuses, sometimes causing symptoms of increased intracranial pressure from venous hypertension secondary to partial sinus occlusion. In patients with idiopathic intracranial hypertension, arachnoid granulations should be ruled out as the cause [311]. Additionally, giant arachnoid granulations occasionally cause osteolysis and subperiosteal hemorrhage [12]. The accurate diagnosis of arachnoid granulations presented with multiple osteolytic lesions was achieved through X-ray scanning, CT, MRI, bone scans, laboratory testing, and follow up imaging, without pathological examination. Precise review of MR images in particular can lead to the correct diagnosis of arachnoid granulations.
We report a rare case of normal arachnoid granulations mimicking multiple osteolytic bone lesions in the occipital bone. In the differential diagnosis of multiple osteolytic lesions in the occipital bone, arachnoid granulations with signal intensities similar to those of CSF should be considered.
Figures and Tables
Fig. 1
Lateral (A) and Townes (B) skull X-rays show multiple osteolytic lesions in the occipital bone without apparent sclerotic margins.
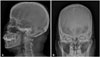
Fig. 2
Brain CT scans on soft-tissue windows (A) and bone windows (B) show multiple osteolytic lesions in the occipital bone around both the transverse sinuses and the torcular herophili, involving both the inner and outer tables.
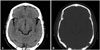
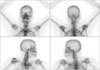
Fig. 3
Brain MRI images reveal a high signal intensity on T2-weighted image (A), a low signal intensity on T1-weighted image (B) and subtle capsules around lesions that are visible after gadolinium injection (C), complete suppression on fluid attenuated inversion recovery image (D), and no restricted diffusion on diffusion-weighted imaging (E).

References
1. Kan P, Stevens EA, Couldwell WT. Incidental giant arachnoid granulation. AJNR Am J Neuroradiol. 2006; 27:1491–1492.
2. Branan R, Wilson CB. Arachnoid granulations simulating osteolytic lesions of the calvarium. AJR Am J Roentgenol. 1976; 127:523–525.

3. Watane GV, Patel B, Brown D, Taheri MR. The significance of arachnoid granulation in patients with idiopathic intracranial hypertension. J Comput Assist Tomogr. 2018; 42:282–285.

4. Trimble CR, Harnsberger HR, Castillo M, Brant-Zawadzki M, Osborn AG. “Giant” arachnoid granulations just like CSF?: NOT!! AJNR Am J Neuroradiol. 2010; 31:1724–1728.

5. Amlashi SF, Riffaud L, Morandi X. Intracranial hypertension and giant arachnoid granulations. J Neurol Neurosurg Psychiatry. 2004; 75:172–174.
6. Leach JL, Meyer K, Jones BV, Tomsick TA. Large arachnoid granulations involving the dorsal superior sagittal sinus: findings on MR imaging and MR venography. AJNR Am J Neuroradiol. 2008; 29:1335–1339.

7. Ikushima I, Korogi Y, Makita O, et al. MRI of arachnoid granulations within the dural sinuses using a FLAIR pulse sequence. Br J Radiol. 1999; 72:1046–1051.

8. Haroun AA, Mahafza WS, Al Najar MS. Arachnoid granulations in the cerebral dural sinuses as demonstrated by contrast-enhanced 3D magnetic resonance venography. Surg Radiol Anat. 2007; 29:323–328.

9. Koshikawa T, Naganawa S, Fukatsu H, Ishiguchi T, Ishigaki T. Arachnoid granulations on high-resolution MR images and diffusion-weighted MR images: normal appearance and frequency. Radiat Med. 2000; 18:187–191.
10. Lu CX, Du Y, Xu XX, et al. Multiple occipital defects caused by arachnoid granulations: emphasis on T2 mapping. World J Radiol. 2012; 4:341–344.

11. Kiroglu Y, Yaqci B, Cirak B, Karabulut N. Giant arachnoid granulation in a patient with benign intracranial hypertension. Eur Radiol. 2008; 18:2329–2332.

12. VandeVyver V, Lemmerling M, De Foer B, Casselman J, Verstraete K. Arachnoid granulations of the posterior temporal bone wall: imaging appearance and differential diagnosis. AJNR Am J Neuroradiol. 2007; 28:610–612.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download