Abstract
Nonconvulsive status epilepticus (NCSE) is an unusual complication in patients treated with cefepime. An 82-year-old woman on maintenance hemodialysis was given cefepime for pneumonia. Her level of consciousness decreased since the administration of cefepime, and she was diagnosed with NCSE based on electroencephalography (EEG) findings. After discontinuation of cefepime, improvement was seen both in the level of consciousness and EEG findings. Clinicians should be aware of cefepime-induced NCSE, particularly in patients with renal failure.
Nonconvulsive status epilepticus (NCSE) is becoming more frequent both in ambulatory patients with cognitive changes and in more critically ill patients. The degree of impairment of the consciousness level varies, ranging from mild confusion to coma. NCSE is a well-known but unusual complication in patients receiving intravenous cephalosporins, especially cefepime as the fourth-generation cephalosporin. Risk factors for NCSE are highdose parenteral administration and renal impairment.1 We report a case of cefepime-induced NCSE in a patient undergoing hemodialysis, even when the dose was adjusted for renal function.
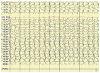
An 82-year-old woman on maintenance hemodialysis for end-stage renal disease, secondary to diabetes mellitus was admitted with a fever that developed a day ago. She had a history of hypertension, diabetes mellitus, hypothyroidism, and aplastic anemia. She had two events of uremic encephalopathy due to insufficient dialysis 3 and 6 months before. The initial laboratory findings were as follows : white blood cell count, 1.84 × 109/L; hemoglobin, 10.5 g/dL; platelet, 111 × 109/L; blood urea nitrogen, 32.6 mg/dL; creatinine, 3.40 mg/dL; sodium 138 mmol/L; calcium, 10.2 mg/dL; protein 5.6 g/dL; albumin 2.8 g/dL; C-reactive protein (CRP), 5.45 mg/dL; thyroid stimulating hormone, 4.81 mIU/L; and free T4, 1.19 ng/dL. There was a pneumonic consolidation on the right lower lung field on the plain chest radiograph. She had a fever of 38.0℃ and received intravenous ceftriaxone, 2 g once a day for pneumonia. The fever continued on the fifth day of hospitalization and administration of intravenous cefepime hydrochloride 2 g every 8 hours was initiated. The fever subsided on the eighth day, and there was no sign of infection with CRP of 0.23 mg/dL. However, the patient's level of consciousness gradually decreased to a state of semicoma. A brain magnetic resonance image revealed no structural lesions associated with the decreased consciousness (Fig. 1). Based on the previous history, daily intensive dialysis was started with the suspicion of uremic encephalopathy. Despite this intensive dialysis for 13 days, there was no improvement in the level of consciousness. A neurological examination showed that the brain stem sign including the Doll's eye was intact. On day 14, a 32 digital channel EEG was performed, and continuously generalized 2 Hz periodic epileptiform discharges were seen (Fig. 2). NCSE was diagnosed, and valproate sodium was administered. However, the EEG on day 15 still showed continuously generalized 2 Hz periodic epileptiform discharges. On day 17, cefepime was stopped under suspicion of cefepime-induced NCSE. On day 24, the patient's consciousness level showed improvement from semicoma to stupor. The EEG was repeated, and the background in the test consisted of symmetrically distributed delta and theta rhythms. On day 46, the level of consciousness recovered to a drowsy state and no definite interictal epileptiform discharge or focal slowing was observed in the EEG (Fig. 3). On day 47, the patient was alert, with intact comprehension and was capable of talking. Therefore, after excluding all other diseases that can cause neurological changes, it is reasonable to consider cefepime-induced NCSE since the level of consciousness improved after its discontinuation.
Altered consciousness in chronic kidney disease patients may have many different etiologies, including metabolic encephalopathy, hypertensive crisis, infectious causes and drug toxicity. NCSE should also be included in the differential diagnosis. NCSE can be defined as an EEG pattern characterized by repetitive generalized or focal spikes, sharp waves, spike-and-wave complexes at = 3/s and lasting = 30 minutes. 2 NCSE may result from several causes, including drugs like antibiotics. Diagnosis of NCSE should be considered in all patients with unexpected changes in consciousness levels, especially those receiving intravenous cephalosporins for impaired renal function.3 An urgent EEG should be considered. It is difficult to distinguish between NCSE and metabolic encephalopathy unless an EEG is performed. In our case, we could confirm the changes in EEG based on the clinical course of cefepime-induced NCSE. In a report by Fugate et al., EEG was performed in 17 out of 100 ICU patients with neurotoxicity after cefepime administration, and the findings included moderate or severe generalized slowing in 70.6%, triphasic waves in 47.1%, multifocal sharp waves in 29.4%, burst-suppression in 11.8%, non-reactive alpha in 5.8%, and NCSE in 5.8% of the patients.4
In our patient, symptoms developed 3 days after cefepime administration and the consciousness level improved 7 days after discontinuation of the drug. While the typical time period for encephalopathy, which is the period between the start of cefepime and neurologic manifestations, varies from 1 to 10 days, its resolution takes place within 2 to 7 days after stopping the antibiotic infusion.5
Cefepime is predominantly cleared from the body by renal secretion, and therefore, requires dose adjustment according to renal function. Cefepime-induced neurotoxicity has frequently been reported and is common in patients with renal impairment without adequate dose adjustment.3 In June 2012, the United States Food and Drug Administration released a cefepime-related safety announcement for patients with renal impairment because of the increased risk of seizure if the dose was not optimally adjusted for kidney function.6 Cephalosporins seem to inhibit gamma-amino-butyric acid (GABA) A-receptor function, resulting in cephalosporin- induced seizures.7 Renal failure is a risk factor for cephalosporin-induced seizures. This is because as the rate of clearance decreases, the concentration of the circulating drug increases, and the central nervous system penetration of the drug increases in the presence of uremia.8 Since the patient in this study had a previous history of uremic encephalopathy, it is presumed that she had uremic conditions at low dialysis efficiency. Because she received an adjusted dose of cefepime, it is presumed that the cefepime-induced NSCE was more likely to occur because of her uremic condition.
In summary, this is a case of cefepime-induced NCSE with periodic follow-up by EEG. With the increasing use of cefepime, clinicians should be aware of cefepime-induced NCSE, particularly in patients with renal failure. Increasing recognition and concern for antibioitics associated encephalopathy can lead to earlier discontinuation of causative medications, reducing time spent and unnecessary investigation and thereby improving outcomes in patients with encephalopathy.
Figures and Tables
Fig. 1
A brain magnetic resonance image revealed no structural lesions associated with the decreased consciousness.

References
3. Fernández-Torre JL, Martínez-Martínez M, González-Rato J, Maestro I, Alonso I, Rodrigo E, et al. Cephalosporin-induced nonconvulsive status epilepticus: clinical and electroencephalographic features. Epilepsia. 2005; 46:1550–1552.

4. Fugate JE, Kalimullah EA, Hocker SE, Clark SL, Wijdicks EF, Rabinstein AA. Cefepime neurotoxicity in the intensive care unit: a cause of severe, underappreciated encephalopathy. Crit Care. 2013; 17:R264.

6. U.S. Department of Health and Human Services. FDA Drug Safety Communication: cefepime and risk of seizure in patients not receiving dosage adjustments for kidney impairment [Internet]. Rockville (MD, USA): FDA;c2016. accessed 2016 Jan 19. Available from: https://www.fda.gov/Drugs/DrugSafety/ucm309661.htm.
7. Sugimoto M, Uchida I, Mashimo T, Yamazaki S, Hatano K, Ikeda F, et al. Evidence for the involvement of GABA(A) receptor blockade in convulsions induced by cephalosporins. Neuropharmacology. 2003; 45:304–314.

8. Schliamser SE. Neurotoxicity of beta-lactam antibiotics. Experimental kinetic and neurophysiological studies. Scand J Infect Dis Suppl. 1988; 55:1–61.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download