Abstract
Posterior fossa epidural hematoma (EDH) is uncommon, but the related clinical deterioration can occur suddenly. Accompanying venous sinus injury and lacerations are associated with 40% to 80% mortality. The authors present one clinical case of a patient with posterior fossa EDH from transverse sinus bleeding. A 57-year-old male was injured after falling while working. He was taken to the hospital, where computed tomography scans of his brain revealed a right posterior temporal and cerebellar EDH with a right temporo-occipital fracture. He underwent a right parieto-occipital craniotomy, incorporating the fracture line. Longitudinal laceration of the right transverse sinus extending to the sigmoid sinus with profuse bleeding was identified. Four gauzes were inserted in the epidural space for tamponade of the injured sinus. Conventional angiography and coil embolization for the injured sinus were immediately performed. Subsequently, the patient was transferred to the operating room, wherein staff members removed the gauzes and remnant hematoma. Based on this experience, the authors recommend that for posterior fossa EDH from transverse sinus bleeding, bleeding control should be performed by gauze packing and endovascular treatment.
Epidural hematomas (EDH) are emergent neurosurgical challenges, and most of them are believed to be of arterial origin, mainly meningeal arteries. One report suggests that the source of bleeding was non-arterial in only 9.7% of all EDH cases, involving diploic veins in bone.6) However, certain anatomic areas are often associated with hematomas, especially following venous sinus injury, for example sagittal suture, and posterior fossa. Nearly 40% of hematomas were reported to be sinus origin, especially in case of EDHs derived from posterior fossa.2311)
The surgical technique for EDHs from sinus injuries often differs from that of EDHs of arterial origin. Failure to achieve adequate hemostasis can lead to massive bleeding and fatal exsanguination in addition to enormous damage to the patient's neural structures. Surgeons often prepare for massive transfusion and bleeding control measures including various hemostatic agents to manage suspected sinus injuries. However, failure of these countermeasures may result in fatal outcome.
We present a case of posterior fossa EDH with massive bleeding following transverse sinus injury. In the face of failure with conventional surgical techniques for direct hemostasis, we used a very old technique (gauze packing) combined with a new challenge (transvenous endovascular embolization of transverse sinus) to successfully control the bleeding.
A 57-year-old male construction worker was transferred to our trauma center after falling from a three-story building at work. Upon arrival, his Glasgow Coma Score was 8 (E1, V1, M5). He had anisocoria with left pupil measuring 4 mm and right pupil measuring 3 mm, both nonreactive to light. After initial resuscitation, computed tomography (CT) scan of whole body was performed. The brain CT showed right posterior temporal and cerebellar EDH with mass effect and shifting (Figure 1A), as well as right temporal and occipital bone fractures (Figure 1B).
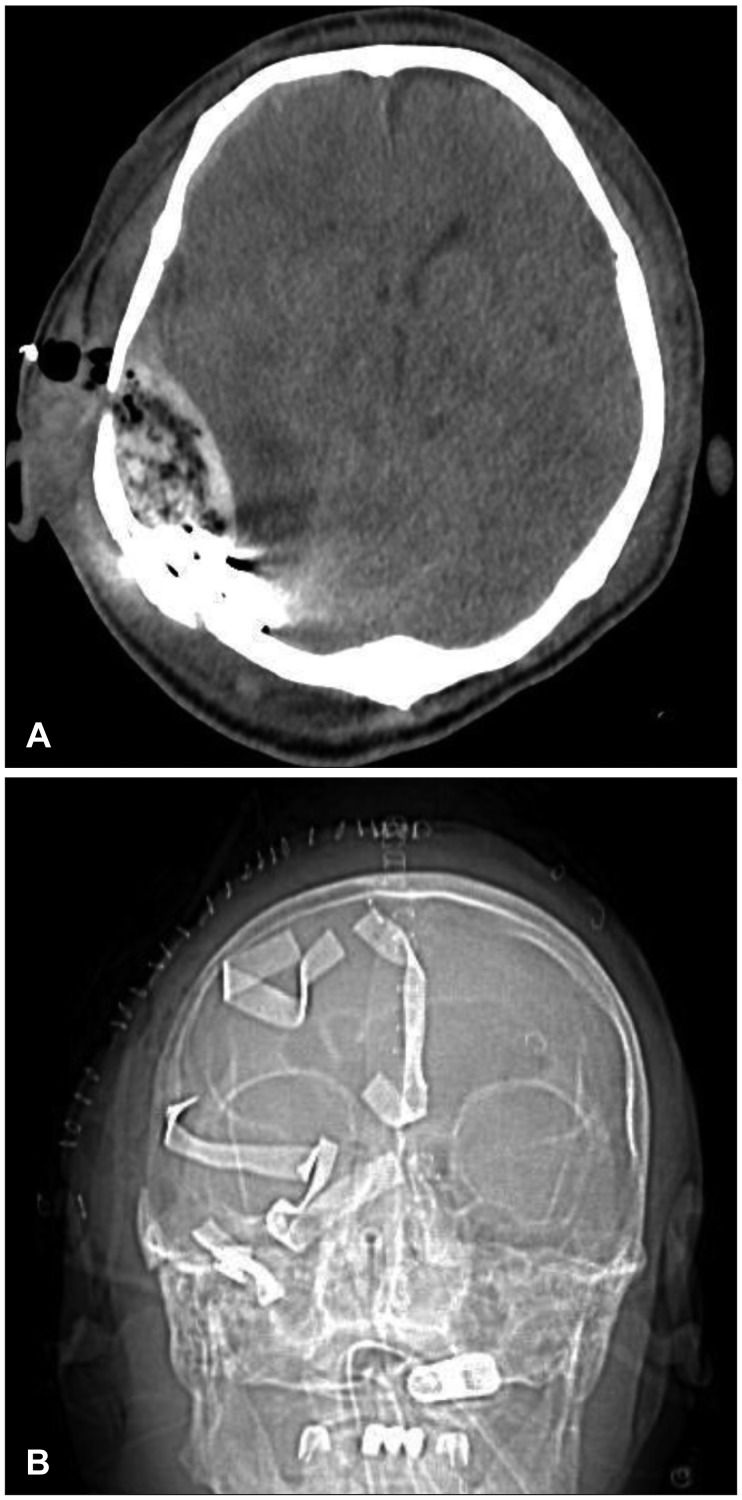
The patient was transferred to the operating room, where he underwent a right parieto-occipital craniotomy, incorporating the fracture line, exposing the right supra- and infratentorial region adjacent to the transverse sinus. A wide longitudinal laceration of the right transverse sinus extending to the right sigmoid sinus with massive bleeding was identified. Hemorrhage from sinus damage was not controlled despite multiple attempts using conventional methods including application of digital pressure with Gelfoam and Tachosil tamponade, proximal and distal ligation, tackup suturing, and a trial of direct repair. Few minutes after, the patient went into hemorrhagic shock rapidly. We inserted four 4×4 inch radiopaque gauze in the epidural space for tamponade. The bone flap was not replaced and the dura was left open. After closure of surgical wound, the patient was rushed back to intensive care unit (ICU) (Figure 2).
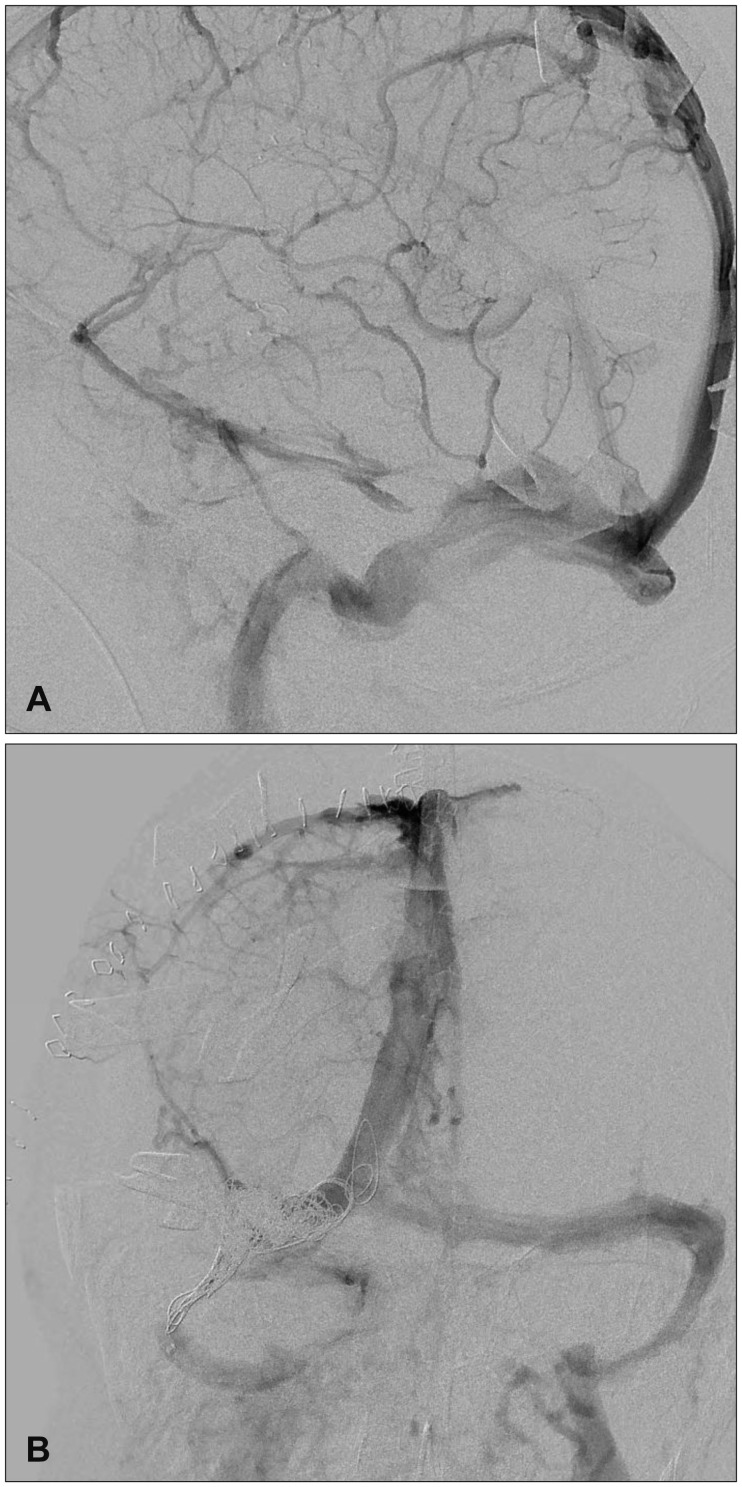
Three days after the operation, when his vital signs became stable, a conventional angiography showed patent distal flow of right transverse sinus with mild stenosis (Figure 3A). We suspected temporal closure of the severed vascular wall with packed gauze tamponade and blood clot formation.
Considering the high risk of rebleeding upon retrieval of packed gauze, we decided to occlude the right transverse sinus using an endovascular technique. A guide-wire was positioned in the right internal jugular vein. After framing of a few detachable coils to prevent coil migration, the total obliteration of right transverse sinus was achieved using multiple pushable coils. Post-embolization angiogram showed no sign of the contrast leakage venous hypertension (Figure 3B).
The patient was subsequently transferred to the operating room. We removed packed gauzes and remnant hematoma, and performed duroplasty. Barbiturate coma treatment was weaned off 7 days after the second operation. A repeat CT scan showed no sign of venous hypertension (Figure 4). After lengthy ICU stay and vigorous rehabilitation, the patient was able to ambulate and was discharged with minimal neurologic deficit.
Although less common than subdural hematomas, EDHs found in 20% of all cases of severe traumatic brain injury and accounting for 14% to 39% of craniotomies of traumatic hemorrhagic lesions, are one of the most important focal brain injuries encountered by neurosurgeons.1314) The pathophysiology of EDH indicates their origin in the dural vessels or the skull following vascular injuries. They are often associated with overlying skull fractures. The classical EDH occurs beneath a temporo-parietal skull fracture as a result of damage to the middle meningeal artery.18) However, occasional non-arterial bleeding, including bleeding from venous dural sinuses, emissary veins, or venous lake within the dura matter, or even a rupture of arachnoid granulation, can be the primary source of the hematoma.920) Surgeons should be aware of the possibility of sinus bleeding when they encounter EDHs within the anatomical locations adjacent to major venous sinuses including vertex,1216) and posterior fossae.411) Other unusual preoperative CT findings indicate possible venous bleeding including bilateral EDHs,7) and hypodense lesions within hematoma.5)
Evacuation of hematoma from sinus injury may increase the risk of massive blood loss in a short period of time. Surgeons often alert anesthesiologists for massive transfusion, and may request local hemostatic agents. Various operative techniques have been used for the repair of injured sinus11) including ligation, digital pressure, Gelfoam tamponade, tissue-glue-coated collagen sponge,10) patch grafting and vein reconstruction.
Packing has been used to deal with severe intracranial hemorrhage probably since the earliest days of intracranial surgery.19) In the modern era of neurosurgery with its vast repertoire of surgical techniques, equipment, and materials, we rarely need this old technique. However, in certain circumstances packing can help when more modern and direct methods fail. For instance, packing may help if the patient sustains injuries to multiple organs with concomitant bleeding elsewhere in the body; severe coagulopathy resulting from massive blood loss; or anticoagulant therapy before the injury. Other instances include pediatric cases with very small systemic blood volume for even moderate loss of blood or when surgical visibility is poor because of complicated injury. Packing was primary our last option for uncontrollable bleeding.
The need for secondary operation and the possibility of infection, which was reported in 0% to 25% in the literature, 819) can be a cumbersome challenge. However, it could be the last resort when more common methods fail.
Reported acute complications of venous sinus occlusion include venous infarction, intracranial hemorrhage, edema, subarachnoid hemorrhage, rapidly progressive illness and coma.117) Fortunately, in our case, diagnostic angiography after gauze packing revealed patent collateral flow through contralateral sinus without evidence of venous hypertension. The authors reasoned that risk of rebleeding was significantly higher than risk of complications of venous sinus occlusion, so they decided to occlude the injured sinus.
The authors failed to find any report of management of injured sinus using endovascular methods. Most of cases involved management of coexisting vascular anomalies such as fistula.20) Traditionally, various techniques such as autologous vein transplants, artificial sinus prosthesis, balloon catheter, or T-drainage for interior splinting were used operatively to repair injured sinus.15) However, with the recent progress of angiographic techniques, endovascular treatment may be a viable treatment option. Further research is needed to assess efficacy of the treatment and possible complications including venous hypertension and infarction.
References
1. Alvis-Miranda HR, Milena Castellar-Leones S, Alcala-Cerra G, Rafael Moscote-Salazar L. Cerebral sinus venous thrombosis. J Neurosci Rural Pract. 2013; 4:427–438. PMID: 24347950.

2. Bor-Seng-Shu E, Aguiar PH, de Almeida Leme RJ, Mandel M, Andrade AF, Marino R Jr. Epidural hematomas of the posterior cranial fossa. Neurosurg Focus. 2004; 16:ECP1.

3. Bozbuğa M, Izgi N, Polat G, Gürel I. Posterior fossa epidural hematomas: observations on a series of 73 cases. Neurosurg Rev. 1999; 22:34–40. PMID: 10348205.

4. Braff SB, Khoshyomn S, D'Angelo WF, Tranmer BI, Wilson JT. Traumatic transverse sinus laceration. Pediatr Neurosurg. 2004; 40:143–144. PMID: 15367807.

5. Chee CP, Habib ZA. Hypodense bubbles in acute extradural haematomas following venous sinus tear. A CT scan appearance. Neuroradiology. 1991; 33:152–154. PMID: 2046901.
6. Cordobés F, Lobato RD, Rivas JJ, Muñoz MJ, Chillon D, Portillo JM, et al. Observations on 82 patients with extradural hematoma. Comparison of results before and after the advent of computerized tomography. J Neurosurg. 1981; 54:179–186. PMID: 7452331.
7. Frank E, Berger TS, Tew JM Jr. Bilateral epidural hematomas. Surg Neurol. 1982; 17:218–222. PMID: 7079941.

8. Freeman JL, Winston KR, Byers JT, Beauchamp K. Damage-control neurosurgery: Packing to halt relentless intracranial bleeding. J Trauma Acute Care Surg. 2015; 79:865–869. PMID: 26496114.
9. Gallagher JP, Browder EJ. Extradural hematoma. Experience with 167 patients. J Neurosurg. 1968; 29:1–12. PMID: 5674087.
10. Gazzeri R, Galarza M, Fiore C, Callovini G, Alfieri A. Use of tissue-glue-coated collagen sponge (TachoSil) to repair minor cerebral dural venous sinus lacerations: technical note. Neurosurgery. 2015; 11(Suppl 2):32–36. PMID: 25584959.
11. Jang JW, Lee JK, Seo BR, Kim SH. Traumatic epidural haematoma of the posterior cranial fossa. Br J Neurosurg. 2011; 25:55–61. PMID: 20925589.

12. Kumar J, Prakash A, Harsh V, Kumar A. Vertex extradural hematoma: A diagnostic dilemma. Asian J Neurosurg. 2017; 12:718–720. PMID: 29114292.

13. Leitgeb J, Mauritz W, Brazinova A, Majdan M, Wilbacher I. Outcome after severe brain trauma associated with epidural hematoma. Arch Orthop Trauma Surg. 2013; 133:199–207. PMID: 23161150.

14. Li LM, Kolias AG, Guilfoyle MR, Timofeev I, Corteen EA, Pickard JD, et al. Outcome following evacuation of acute subdural haematomas: a comparison of craniotomy with decompressive craniectomy. Acta Neurochir (Wien). 2012; 154:1555–1561. PMID: 22752713.

15. Meier U, Gärtner F, Knopf W, Klötzer R, Wolf O. The traumatic dural sinus injury--a clinical study. Acta Neurochir (Wien). 1992; 119:91–93. PMID: 1481760.
16. Schöggl A, Reddy M, Saringer W, Matula C. An unusual management of an open compound depressed skull fracture with venous sinus involvement. A case report. J Neurosurg Sci. 1999; 43:311–314. PMID: 10864395.
17. Siddiqui FM, Kamal AK. Complications associated with cerebral venous thrombosis. J Pak Med Assoc. 2006; 56:547–551. PMID: 17183989.
18. Winston KR, Byers JT, Freeman J, Beauchamp K. Packing to tamponade severe intracranial hemorrhage in pediatric patients. Pediatr Neurosurg. 2015; 50:63–67. PMID: 25824532.

19. Wong GK, Poon WS, Yu SC, Zhu CX. Transvenous embolization for dural transverse sinus fistulas with occluded sigmoid sinus. Acta Neurochir (Wien). 2007; 149:929–935. PMID: 17700989.

20. Yilmazlar S, Kocaeli H, Dogan S, Abas F, Aksoy K, Korfali E, et al. Traumatic epidural haematomas of nonarterial origin: analysis of 30 consecutive cases. Acta Neurochir (Wien). 2005; 147:1241–1248. PMID: 16133767.

FIGURE 1
The 57-year-old male admitted after falling from a three-story building. (A) The initial computed tomography scan showed right posterior temporal and cerebellar extradural haemorrhage with mass effect and shifting. (B) Right temporal and occipital bone fractures were showed.
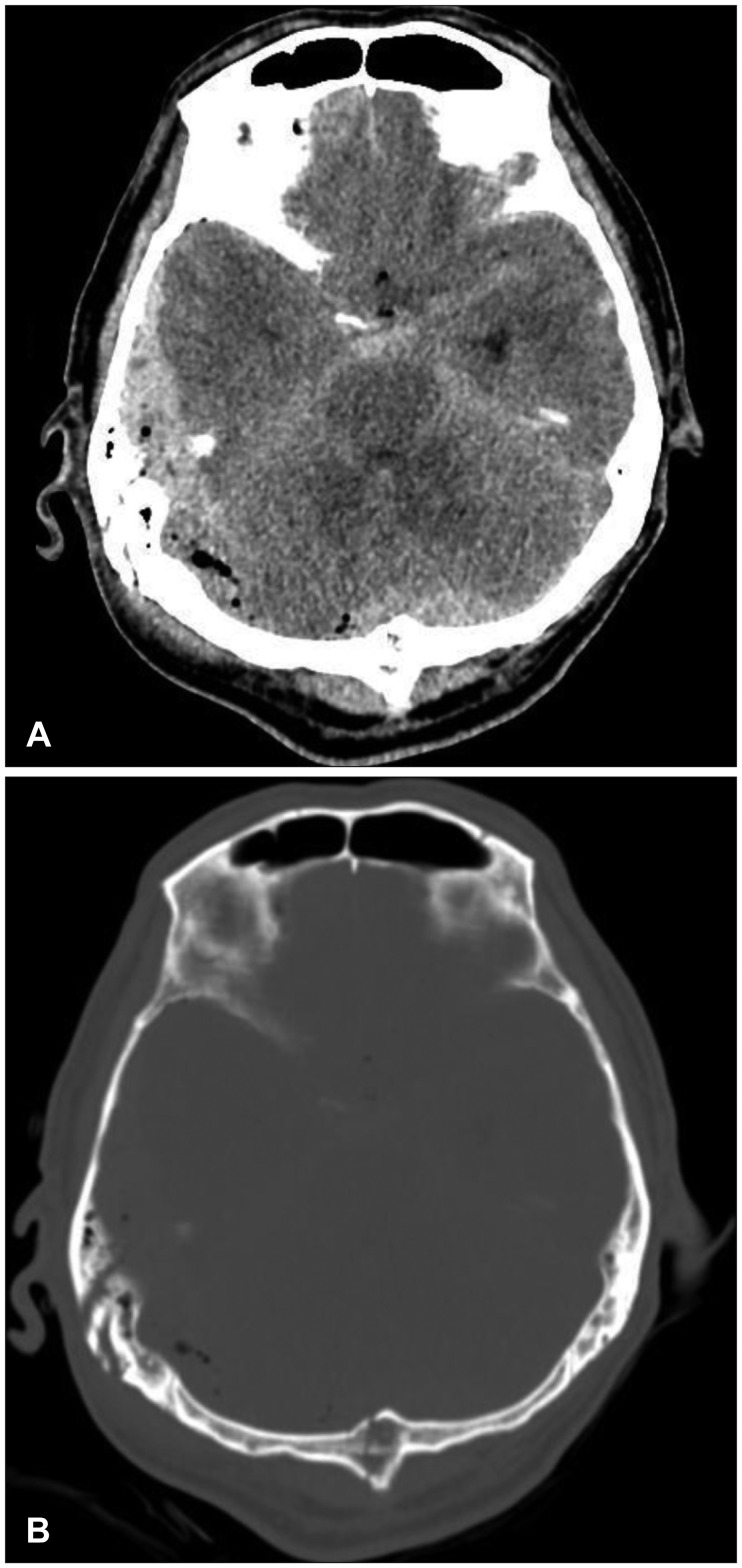
FIGURE 2
(A) Postoperative computed tomography scan confirmed radiopaque gauze in the epidural space. (B) Skull X-ray showed radiopaque gauze in the cranial space.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download