DISCUSSION
It is important to promote compliance with preventive behaviors of individuals in community for preventing outbreak and infection control. This study identified the level of compliance with respiratory infection preventive behaviors and its related factors in community dwelling elderly as high risk population at a critical time of respiratory infection control. The results of this study may be useful for developing specific interventions to improve compliance as prevention measure for older people in community-based approach. In addition, previous studies have focused mainly on the vaccination rate, which is a pharmaceutical intervention, but this study is differentiated from other studies in that it deals with several major non-pharmaceutical preventive behaviors against respiratory infections. Also, since the specific compliance with each behavior was examined, the results are expected to serve as a basis in understanding the problems of the target group and developing appropriate promotion strategies. Above all, it is meaningful that this study paid attention to social welfare facilities, a blind spot in the management of infectious diseases which has not yet been actively dealt with in studies in Korea, and this study targeted the elderly using a senior center at potential risk of infection transmission because where social contact and activities of many elderly people occur.
In this study, we investigated the vaccination rate of older people as one of their health related characteristics. As a result, 65.0% of the participants responded that they had received pneumococcal vaccination and 83.0% responded that they had received influenza vaccination. The results are consistent with a prior study which reported that the influenza vaccination rate in older people in Korea is over 80.0%[
9], but they are somewhat different from the results of other previous studies [
1019] which reported that the pneumococcal vaccination rate was 19.3% in 2011 [
19] and 56.3% in 2015[
10]. These discrepancies in the study results can be attributed to the differences in the time of survey. In Korea, the free pneumococcal immunization program for older people aged 65 years and over has been implemented since 2013, which is thought to explain the fact that the pneumococcal vaccination rate in this study investigated in 2017, seems to be higher than the vaccination rate reported in the previous study. In a previous study, most elderly people did not receive pneumococcal vaccines because they didn't know about the vaccination well [
19]. In a similar vein, the univariate analysis of this study showed that the level of knowledge related to respiratory infection and preventive behaviors was higher in participants who were vaccinated against pneumococcal disease. As a result of the free immunization program as cost support, active provision of information through the public health center and the mass media is thought to have contributed to the improvement of pneumococcal vaccination rate. However, since it is still lower than the influenza vaccination rate, considering the fact that the advice of healthcare providers affects vaccination rate, professional advice and active promotion by the healthcare providers in community institutions such as senior centers are expected to contribute to the prevention of respiratory infections and health promotion in older people.
The mean score for knowledge of respiratory infection and preventive behaviors was 7.52 points, and older people using a senior center had correct knowledge about only half of 13 items. Particularly, the scores of general knowledge and knowledge of preventive behaviors were low. The responses of the items about general knowledge showed that many people incorrectly knew that ‘influenza and the cold are the same disease and influenza is just severe type of a cold’ and many respondents also had the misinformation that ‘a person who have received vaccines does not get pneumonia or influenza’. The respondents showed a lack of knowledge about the correct method of hand washing among the items on preventive behaviors. It is important to perform hand washing with proper method, duration, and frequency as recommended [
2]. Although the survey was conducted by the self-report method in this study, only 6.0% of the participants reported that they wash their hands using soap for at least 30 seconds 8 times or more a day. Compared with a Thailand study of various age groups in which compliance with hand washing using soap was 33.5% [
23], and a study conducted in Korean which reported compliance with hand washing was 15.9% in adults [
12], the compliance with hand washing among elderly people in this study was rather lower. These results indirectly show that although elderly people know the conventional wisdom that they should wash their hands and self-report that they frequently wash their hands, but they do not practice hand washing with proper way because of lack of knowledge about recommended method. Although the Korea Centers for Disease Control and Prevention (KCDC) has been providing information through various strategies to raise public awareness such as ‘1830 hand washing’, it might be an ineffective way to improve knowledge and compliance with health behaviors in the older population in view of study results [
2]. Therefore, behavior change strategies are needed to help to get correct knowledge and this can be linked to compliance with health behaviors.
Among the older people using a senior center who participated in this study, only 12.0% responded that they always adhere to cough etiquette. This result is slightly different from that of a previous study which reported that compliance with cough etiquette was 30.9% in 1,000 people aged 13 years or older [
13]. However, the results in this study is similar to that of Nasreen et al. [
24] which found that 7.7% adhered to cough etiquette in a proper way among people aged 1 to 83 years old through direct observation by visiting schools and homes. Korea has experienced an outbreak of MERS, and the incidence of tuberculosis and associated mortality are the highest among OECD countries. Recently, there has been massive promotion about cough etiquette to increase the public awareness about it. However, the results of this study revealed that the compliance with cough etiquette was very low among older people. In a previous study, the main reason for not complying with cough etiquette was that ‘I don't have a habit of cough etiquette’ (72.3%) [
13], confirming the importance of the habitual practice of health behaviors. Health behaviors are difficult to become habitual in a short period, so long-term plans for the habituation of correct cough etiquette is required.
In this study, 51.0% of the participants responded that they brushed their teeth more than three times a day. This was slightly higher than reported by a previous study [
14]. However, only 36.0% of the participants said that they brushed their teeth for more than 3 minutes, 62.0% did not practice dental cleaning using a interdental brush or tooth floss. Many older people performed oral hygiene behaviors for a shorter time than recommended or did not perform required essential oral hygiene behaviors. If the plaque is not properly removed by toothbrushing and interdental cleaning, it will increase the risk of oral disease, and this may lead directly to general diseases such as pneumonia. Therefore, there is a need to implement education to provide elderly using a senior center with information about the proper brushing technique and the types, effects, and uses of oral hygiene products.
Univariate analysis showed significant differences in the rate of compliance with hand washing and cough etiquette according to marital status, living arrangement, and smoking status. Married people had a higher level of compliance than people who were widowed, and this finding is consistent with a prior study by Song and Yang [
2] which reported that compliance was higher in married people. However, this study has limitations in interpretation of the findings because only two of the participants were unmarried. In order to consistently explain the relationship between marital status and preventive behaviors, further research is needed. When considered with the result that household size was positively correlated with compliance with hand washing and cough etiquette, the finding that compliance was higher in those who live with three-generation or with the spouse and children may be explained that an individual who live with more family has more opportunity to acquire health information and to perform self-care through the family dynamics, and there is an effect of monitoring the health behavior among the family members [
2]. A higher compliance in smokers was inconsistent with the results of Lee and Suh [
10] that showed that pneumococcal vaccination rate was higher in non-smokers. This can be interpreted as a solution to the cognitive conflict to compensate for the negative consequences of health risk behaviors by implementing other health behaviors [
25]. In this way, compliance with respiratory infection preventive behaviors were found to be different according to the characteristics of individuals. Especially, older people living alone may have poor compliance with health behavior. The number of elderly people living alone is expected to increase in the future [
26], so support and management for them are needed.
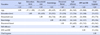
In order to identify the factors influencing compliance with respiratory infection preventive behaviors, stepwise regression analysis was performed, and the results showed that self-efficacy was the most significant factor in the two models for hand washing and cough etiquette (β=.46,
p<.001) and for oral hygiene (β=.25,
p=.011). In this study, we attempted to examine perceived threat and self-efficacy in the modified health belief model as major variables, but only self-efficacy was found to be a significant factor. This is similar to the results of a meta-analysis study of the health belief model [
27], in which perceived susceptibility and perceived severity constituting perceived threat were somewhat less influential in explaining health behaviors except medication adherence. However, perceived threat may be influenced by situational contexts, so it may be helpful to understand relationship between perceived threat and preventive behaviors if additional survey and research are conducted in autumn and winter, when respiratory infectious diseases are more common, rather than in summer. On the other hand, people with higher level of self-efficacy have good compliance with respiratory infection preventive behaviors. This result is consistent with a study in Hong Kong which showed a high correlation between self-efficacy and preventive behaviors [
17]. Self-efficacy is an important theoretical concept in the disease prevention and health promotion of older people, and interventions including strategies to enhance self-efficacy have been reported to have positive effect on compliance with health behaviors [
28]. These findings suggest that strategies to improve self-efficacy should be considered when developing interventions to promote respiratory infection preventive behaviors in Korean older people.
In the regression model for hand washing and cough etiquette, age was a significant factor. As age was increased, compliance with hand washing and cough etiquette was decreased. This finding is consistent with a study in UK [
29] which found that compliance with recommended preventive behaviors was lower in older adults than those aged 18~24 at the novel influenza A (H1N1) outbreak in 2009. This might be due to the fact that younger people have higher goals to achieve through health behaviors or that younger people have more experience about health education or exposure to health information in light of a negative correlation between age and education level found in this study.
In the regression model for oral hygiene, education level and cancer diagnosis were significant factors. Participants with high education level or without cancer are more likely to compliant oral hygiene. This result is consistent with that of a previous study conducted in Hong Kong which reported that as the education level was higher, the level of compliance with preventive behaviors against severe acute respiratory syndrome was increased [
17]. These findings may be explained by the fact that older people with higher education level may have more favorable living conditions for performing health promotion activities or have more opportunities to receive information about the importance or effects of oral hygiene. In addition, compliance was higher in people without cancer than those with cancer. This result is consistent with a prior study which reported that older people without cancer were more likely to perform health promotion behaviors such as sleeping and exercise [
30]. Cancer patients are required to perform oral hygiene because of compromised immune function and a high risk of respiratory infections due to chemotherapy and hospitalization. Considering that there may be differences in physical and psychosocial function between cancer patients and general older people, other approaches recommending methods that are easy to perform or suitable for cancer patients are required.
According to the Korean National Statistical Office, the proportion of older women among people aged 65 and over was 57.5% in 2017 [
26]. In this study, 86.0% of the participants were older women, and the participants were selected from the older people using a senior center in a region. For this reason, there are limitations on the generalization of this study findings to the entire older population in Korea. In addition, in this study, the environmental status such as hand sanitizers, paper towels, and posters promoting respiratory infection preventive behaviors was not considered. Thus, further studies are required to investigate the environment or supplies of senior centers in Korea by evaluation methods. Moreover, the compliance with respiratory infection preventive behaviors were measured by self-report in this study, compliance with hand washing or cough etiquette may have been over-reported in socially desirable direction, and thus caution is needed in interpretations of the results.
CONCLUSION
The purpose of this study was to investigate the level of compliance with respiratory infection preventive behaviors and the related factors among older people using a senior center. The study results showed that compliance with hand washing, cough etiquette, and oral hygiene were low in older people using a senior center. Therefore, it is necessary to promote hand washing, cough etiquette, and oral hygiene behaviors for prevention of infectious diseases of elderly people using senior centers.
In order to explore the measures to promote the behaviors, stepwise regression analysis was conducted to identify the related factors. As a result, for hand washing and cough etiquette, the regression model with self-efficacy for respiratory infection preventive behavior and age showed the explanatory power of 24.0% and was statistically significant. For oral hygiene, the regression model with self-efficacy, educational level, and cancer diagnosis showed the explanatory power of 14.0% and was statistically significant. In two models, self-efficacy for respiratory infection preventive behavior was the most influential factor. The results of this study suggest that differentiated approach should be applied considering the characteristics such as age and education level and that it is necessary to develop programs based on self-efficacy. In addition, in future studies, it is necessary to conduct research on the qualitative aspects of respiratory infection preventive behaviors concerning whether preventive behaviors are properly performed among elderly people based on the results of previous studies and the fact that the participants of this study showed lack of knowledge about the recommended methods of preventive behaviors.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download