Abstract
Purpose
To compare the changes in activities of daily living (ADLs) in older adults with stroke in different modalities of long term care (LTC) services, which include home care and institutional care.
Methods
This is a comparative study using secondary data from the Korean national LTC insurance. Home care (HC) services users (n=3,494) and institutional care (IC) users (n=1,428) were extracted and compared in terms of ADLs and changes in ADLs to investigate the effects of HC and IC services in LTC.
Results
All of the ADLs and LTC services benefit levels for 2 years had improved in both HC and IC services. The ADLs of older adults with stroke who received HC improved, while those who received IC experienced deterioration. The LTC services benefit levels of the HC and IC groups were significantly different after 2 years.
Figures and Tables
Table 1
Baseline Characteristics according to Service Type (N=4,922)
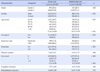
Table 2
Profiles of Activities of Daily Living according to Service Type (N=4,922)
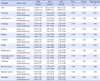
Table 3
Maintenance, Improvement and Worsening of Outcomes over Time according to Service Type (N=4,922)

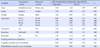
Table 4
Multiple Logistic Regression to Predict Change of Activities of Daily Living by 2009~2010 (N=4,922)
References
1. Statistics Korea. Trend of stroke prevalence. [Internet]. Daejeon: Statistics Korea;2015. cited 2016 July 20. Available from: http://kosis.kr/wnsearch/totalSearch.jsp.
2. Kim MH, Jung YH, Lee DH. Cardiovascular diseases prevention and control campaign, 2015. Public Health Wkly Rep. 2015; 8(39):925–928.
3. Kwon YD, Chang HJ, Choi YJ, Yoon SS. Nationwide trends in stroke hospitalization over the past decade. J Korean Med Assoc. 2012; 55(10):1014–1025. DOI: 10.5124/jkma.2012.55.10.1014.

4. Kim HS, Kim JM, Yim HS, Hong JS, Ha DS, Kwon JB. Efficient recycling based on research generated through the use of analysis of acute care stroke patients. Goyang: National Health Insurance Service Ilsan Hospital;2015. 12. Report No.: 2015-20-023.
5. Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ, et al. Informal care for stroke survivors: Results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2002; 33(4):1028–1033.
6. Kang EJ, Kim DJ, Sun YD, Yoon SS. Development of health care system for the elderly with medical expenditure analysis. Seoul: Korea Institute for Health & Social Affairs;2006. 12. Report No.: 2006-05.
7. Hyun KR, Lee SM. Effects on the functional status changes of LTC (Long Term Care) services. J Korean Gerontol Soc. 2012; 32(2):593–609.
8. Lee S, Kwak C. Effects of visiting nursing services in long-term care insurance on utilization of health care. J Korean Acad Community Health Nurs. 2016; 27(3):272–283. DOI: 10.12799/jkachn.2016.27.3.272.

9. National Health Insurance Service. Statistical yearbook of longterm care insurance for the elderly. Seoul: National Health Insurance Service;2015. p. 685.
10. Yoon JY, Lee JY. Development of outcome indicators of urinary incontinence for quality evaluation in long term care hospitals. J Korean Acad Nurs. 2010; 40(1):110–118. DOI: 10.4040/jkan.2010.40.1.110.

11. Mitchell JB. Patient outcomes in alternative long-term care setting. Med Care. 1978; 16(6):439–452.
12. Marek KD, Popejoy L, Petroski G, Mehr D, Rantz M, Lin WC. Clinical outcomes of aging in place. Nursing Research. 2005; 54(3):202–211.

13. Braun KL, Rose CL, Finch MD. Patient characteristics and outcomes in institutional and community long-term care. Gerontologist. 1991; 31(5):648–656.

14. Lee TW, Cho EH, Yim EH, Lee HS, Ko YK, Kim BN, et al. Activities of daily living in nursing home and home care settings: A retrospective 1-year cohort study. J Am Med Dir Assoc. 2015; 16(2):114–119. DOI: 10.1016/j.jamda.2014.07.013.

15. Park CJ. Cost-effectiveness analysis of long-term care services: care in institution vs in-home care. J Welf Aged. 50:145–172.
16. You HJ, Lee HY, Kim KA, Jo JH, Kim DH. Strengthening longterm care facility services expertise. Seoul: National Health Insurance Service;2013. 11. 30. Report No.: 2013-12.
17. Kown JH, Han EJ, Lee JS. Long-term care services payroll management improvement. Research Report. Seoul: National Health Insurance Corporation;2009. 12. Report No.: 2009-33.
18. Lee TW, Yim EH, Cho EH, Chung JN. Cognitive function, behavioral problems, and physical function in long-term care insurance beneficiaries with dementia in south Korea: Comparison of home care and institutional care services. J Am Geriatr Soc. 2014; 62(8):1467–1475. DOI: 10.1111/jgs.1294.

19. Lee K, Cho E. Activities of daily living and rehabilitation needs for older adults with a stroke: A comparison of home care and nursing home care. Jpn J Nurs Sci. 2016; 7:1–9. DOI: 10.1111/jjns.12139.

20. Kane RL, Chen Q, Finch M, Blewett L, Burns R, Moskowitz M. Functional outcomes of posthospital care for stroke and hip fracture patients under medicare. J Am Geriatr Soc. 1998; 46(12):1525–1533.

21. Kane RL, Chem Q, Blewett LA, Sangl J. Do rehabilitative nursing homes improve the outcomes of care? J Am Geriatr Soc. 1996; 44(5):545–554.

22. Mun BM, Lee YS, Lee BH. The relationship between the patient's health beliefs and the implementation of functional movement rehabilitation and ability to perform ADL in stroke patients. J Korea Acad Ind Coop Soc. 2012; 13(7):3057–3064. DOI: 10.5762/KAIS.2012.13.7.3057.

23. Hwang HJ, Lee KY, Kim SH. Physical and emotional status of nursing home residents: long-term care of older people via Incheon nursing home network study. J Korean Geriatr Soc. 2010; 14(3):139–146. DOI: 10.4235/jkgs.2010.14.3.139.
24. Boyd M, Broad JB, Kerse N, Foster S, von Randow M, Lay-Yee R, et al. Twenty-year trends in dependency in residential aged care in Auckland, New Zealand: A descriptive study. J Am Med Dir Assoc. 2011; 12(7):535–540. DOI: 10.1016/j.jamda.2011.01.014.

25. Hwang EH, Jung DY, Kim MJ, Kim KH, Shin SJ. Comparison of frequency and difficulty of care helper jobs in long term care facilities and client homes. J Korean Public Health Nurs. 2012; 26(1):101–112. DOI: 10.5932/JKPHN.2012.26.1.101.

26. Jette DU, Warren RL, Wirtalla C. Rehabilitation in skilled nursing facilities: Effect of nursing staff level and therapy intensity on outcomes. Am J Phys Med Rehabil. 2004; 83(9):704–712.
27. Lee JS, Han EJ, Lee HY, Lee JS. The report on incentives institution improvement measurements for improving the quality of long-term care services. Seoul: National Health Insurance Service;2012. 11. 30. Report No.: 2012-17.
28. Lee MK, Kim EK. Relationship between resource utilization and long-term care classification level for residents in nursing homes. J Korean Acad Nurs. 2010; 40(6):903–912. DOI: 10.4040/jkan.2010.40.6.903.

29. Yang YA, An SJ, Park YH, Park BR, Heo J, Park JS, et al. A study of visiting rehabilitation service and implementation method. J Korean Assoc Occup Ther Policy Aged Ind . 2011; 3(1):59–70.
30. Lee S, Kwak C. Effects of Visiting Nursing Services in Long-term Care Insurance on Utilization of Health Care. J Korean Acad Community Health Nurs. 2016; 27(3):272–283. DOI: 10.12799/jkachn.2016.27.3.272.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download