1. Miller EL, Murray L, Richards L, Zorowitz RD, Bakas T, Clark P, Billinger SA. American Heart Association Council on Cardiovascular Nursing and the Stroke Council. Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: a scientific statement from the American Heart Association. Stroke. 2010; 41:2402–2448.
2. Centers for Disease Control and Prevention (US). Traumatic brain injury in the united states: a report to congress. Atlanta, GA: Centers for Disease Control and Prevention;1999.
3. Testa JA, Malec JF, Moessner AM, Brown AW. Outcome after traumatic brain injury: effects of aging on recovery. Arch Phys Med Rehabil. 2005; 86:1815–1823.

4. Huang ME, Cifu DX, Keyser-Marcus L. Functional outcome after brain tumor and acute stroke: a comparative analysis. Arch Phys Med Rehabil. 1998; 79:1386–1390.

5. van Mierlo ML, van Heugten CM, Post MW, Hajós TR, Kappelle LJ, Visser-Meily JM. Quality of life during the first two years post stroke: the Restore4Stroke cohort study. Cerebrovasc Dis. 2016; 41:19–26.

6. Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009; 338:b375.

7. Young FB, Weir CJ, Lees KR. GAIN International Trial Steering Committee and Investigators. Comparison of the National Institutes of Health Stroke Scale with disability outcome measures in acute stroke trials. Stroke. 2005; 36:2187–2192.

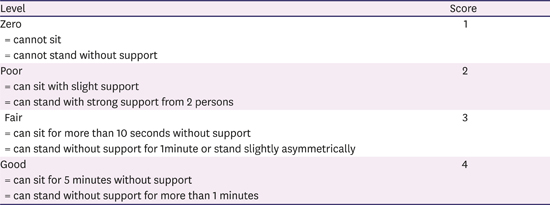
8. Benaim C, Pérennou DA, Villy J, Rousseaux M, Pelissier JY. Validation of a standardized assessment of postural control in stroke patients: the Postural Assessment Scale for Stroke Patients (PASS). Stroke. 1999; 30:1862–1868.
9. Veerbeek JM, Kwakkel G, van Wegen EE, Ket JC, Heymans MW. Early prediction of outcome of activities of daily living after stroke: a systematic review. Stroke. 2011; 42:1482–1488.
10. Mutai H, Furukawa T, Araki K, Misawa K, Hanihara T. Factors associated with functional recovery and home discharge in stroke patients admitted to a convalescent rehabilitation ward. Geriatr Gerontol Int. 2012; 12:215–222.

11. Ng YS, Stein J, Salles SS, Black-Schaffer RM. Clinical characteristics and rehabilitation outcomes of patients with posterior cerebral artery stroke. Arch Phys Med Rehabil. 2005; 86:2138–2143.

12. Oneş K, Yalçinkaya EY, Toklu BÇ, Cağlar N. Effects of age, gender, and cognitive, functional and motor status on functional outcomes of stroke rehabilitation. NeuroRehabilitation. 2009; 25:241–249.
13. Ostwald SK, Swank PR, Khan MM. Predictors of functional independence and stress level of stroke survivors at discharge from inpatient rehabilitation. J Cardiovasc Nurs. 2008; 23:371–377.

14. Abdul-sattar AB, Godab T. Predictors of functional outcome in Saudi Arabian patients with stroke after inpatient rehabilitation. NeuroRehabilitation. 2013; 33:209–216.

15. Bagg S, Pombo AP, Hopman W. Effect of age on functional outcomes after stroke rehabilitation. Stroke. 2002; 33:179–185.

16. Black-Schaffer RM, Winston C. Age and functional outcome after stroke. Top Stroke Rehabil. 2004; 11:23–32.

17. Denti L, Agosti M, Franceschini M. Outcome predictors of rehabilitation for first stroke in the elderly. Eur J Phys Rehabil Med. 2008; 44:3–11.
18. O'Brien SR, Xue Y. Inpatient rehabilitation outcomes in patients with stroke aged 85 years or older. Phys Ther. 2016; 96:1381–1388.
19. Mayo NE, Wood-Dauphinee S, Ahmed S, Gordon C, Higgins J, McEwen S, Salbach N. Disablement following stroke. Disabil Rehabil. 1999; 21:258–268.
20. Massucci M, Perdon L, Agosti M, Celani MG, Righetti E, Recupero E, Todeschini E, Franceschini M. Italian Cooperative Research (ICR2). Prognostic factors of activity limitation and discharge destination after stroke rehabilitation. Am J Phys Med Rehabil. 2006; 85:963–970.

21. Wagle J, Farner L, Flekkøy K, Bruun Wyller T, Sandvik L, Fure B, Stensrød B, Engedal K. Early post-stroke cognition in stroke rehabilitation patients predicts functional outcome at 13 months. Dement Geriatr Cogn Disord. 2011; 31:379–387.

22. Han TR, Kim JH, Seong DH, Chun MH. The correlation of the mini-mental state examination (MMSE) and functional outcome in the stroke patients. J Korean Acad Rehabil Med. 1992; 16:118–122.
23. Jakavonytė-Akstinienė A, Dikčius V, Macijauskienė J. Prognosis of treatment outcomes by cognitive and physical scales. Open Med (Wars). 2018; 13:74–82.
24. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198.
25. Bunevičius R. Protinės būklės mini tyrimas. Biol Psychiatry Psychopharmacol. 2000; 2:13.
26. Verheyden G, Nieuwboer A, De Wit L, Feys H, Schuback B, Baert I, Jenni W, Schupp W, Thijs V, De Weerdt W. Trunk performance after stroke: an eye catching predictor of functional outcome. J Neurol Neurosurg Psychiatry. 2007; 78:694–698.

27. Alexander NB, Galecki AT, Nyquist LV, Hofmeyer MR, Grunawalt JC, Grenier ML, Medell JL. Chair and bed rise performance in ADL-impaired congregate housing residents. J Am Geriatr Soc. 2000; 48:526–533.

28. Cabanas-Valdés R, Bagur-Calafat C, Girabent-Farrés M, Caballero-Gómez FM, Hernández-Valiño M, Urrútia Cuchí G. The effect of additional core stability exercises on improving dynamic sitting balance and trunk control for subacute stroke patients: a randomized controlled trial. Clin Rehabil. 2016; 30:1024–1033.

29. Moore S, Brunt D. Effects of trunk support and target distance on postural adjustments prior to a rapid reaching task by seated subjects. Arch Phys Med Rehabil. 1991; 72:638–641.
30. Duarte E, Marco E, Muniesa JM, Belmonte R, Diaz P, Tejero M, Escalada F. Trunk control test as a functional predictor in stroke patients. J Rehabil Med. 2002; 34:267–272.

31. Hsieh CL, Sheu CF, Hsueh IP, Wang CH. Trunk control as an early predictor of comprehensive activities of daily living function in stroke patients. Stroke. 2002; 33:2626–2630.

32. Franchignoni FP, Tesio L, Ricupero C, Martino MT. Trunk control test as an early predictor of stroke rehabilitation outcome. Stroke. 1997; 28:1382–1385.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download