INTRODUCTION
Osteocalcin, a bone-derived protein secreted by osteoblasts, is a bone formation marker, also known as a marker for bone turnover. It has been used clinically to assess the effectiveness of osteoporosis treatments.
Recently, it has been discovered that osteocalcin also acts as a hormone to control glucose and energy metabolism on pancreatic β-cells and adipose and muscle tissues.[
1]
In one animal experiment, genetically modified mice were not able to secrete osteocalcin while exhibiting decreased β-cell proliferation, glucose intolerance and insulin resistance.[
2] When recombinant osteocalcin was injected into the wild-type mice, an increase in pancreatic β-cell proliferation, insulin secretion and a reduction in body fat were observed.[
3] In addition, in a cross-sectional and a prospective study involving human subjects, serum osteocalcin concentration was observed to be inversely correlated to fasting blood glucose, insulin resistance, and body fat mass.[
45]
Moreover, osteocalcin has been receiving much attention for being an indicator of cardiovascular diseases. Recent studies have reported that serum osteocalcin concentration may be associated with calcification of the coronary arteries and the aorta, thickness of the intima-media of the carotid artery, and formation of atherosclerotic plaques in the carotid artery.[
6789] Although these studies have shown that osteocalcin concentration in the blood may be independently correlated with increased risk of cardiovascular diseases, the results lack consistency; there have been other reports suggesting no relation of osteocalcin to the incidence of cardiovascular diseases.[
10]
With the recent and rapid development of multidetector computed tomography (MDCT), coronary computed tomography (CT) angiography through MDCT has been widely used to detect the presence of atherosclerotic plaques in the coronary arteries and to assess the degree of stenosis.
This study investigates the relationship between serum osteocalcin level and insulin resistance measured by using the homeostasis model assessment of insulin resistance (HOMA-IR) index, as well as the relationship between the presence of atherosclerotic plaques in the coronary arteries by using coronary CT angiography and osteocalcin concentration.
METHODS
1. Study subjects
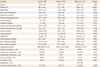
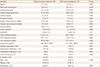
We retrospectively collected study subjects aged over 20 years who had simultaneously undergone coronary CT angiography and blood test including serum osteocalcin, glucose, insulin, calcium, phosphorus, lipids and alkaline phosphatase (ALP) for routine health check-up from January 2012 to December 2015. A total of 98 people (24 men and 74 women) who visited a health promotion center voluntarily included as subjects. Their medical records were investigated in a retrospective manner.
Subjects were excluded if their medical records and questionnaires indicated that they were taking medications or health supplements that could affect their bone and mineral metabolism, such as hormones, osteoporosis medications, or calcium and vitamin D supplements. They were also excluded if they were taking heparin or warfarin, which could affect vitamin K metabolism. Subjects who had any of the following were also excluded: thyroid diseases, parathyroid diseases, abnormal calcium and bone metabolism, autoimmune diseases, renal, cardiovascular, cerebrovascular diseases, and malignant tumors.
2. Questionnaire and body measurement
Based on the questionnaire results and medical records, we investigated if the subjects were taking any medications for diabetes, high blood pressure, and hyperlipidemia. We also looked at histories of smoking or menopause. Subjects were deemed as post-menopausal if they had not menstruated for the past 12 months.
The subjects had a cuff of an appropriate size wrapped around their upper arms, and a mercury sphygmomanometer was used to measure their systolic and diastolic blood pressure, while sitting on a chair in a relaxed state.
Subjects took off their clothes and shoes, and changed into examination gowns. Their heights were measured to the nearest 0.1 cm and their weights to the nearest 0.1 kg, by using a Fatness Measuring system (Fanics, Busan, Korea). Body mass index (BMI) was measured by dividing the body mass (kg) by the square of the body height (m2).
3. Blood test
Blood sample was collected after the subjects fasted for 12 hr. The concentrations of calcium, phosphorus, glucose, and lipids and ALP concentration were measured by using an automatic chemical analyzer (AU-5400; Olympus Optical Co, Tokyo, Japan). Insulin concentration was measured through radioimmunoassay (RIA) by using a human insulin specific RIA kit (Linco Research Inc., St. Charles, MO, USA).
Osteocalcin concentration was measured under electrochemiluminscence immunoassay (ECLIA) by using a N-MID osteocalcin kit (Roche Diagnostics, Mannheim, Germany). By using fasting plasma glucose and insulin as indicators of insulin resistance, the HOMA-IR ([Fasting insulin (µIU/mL)×fasting plasma glucose (mmol/L)] / 22.5) was calculated.[
11]
4. Coronary CT angiography
Using a 128 channel dual-source coronary CT angiography (Somatom Definition®; Siemens Healthcare, Forchheim, Germany), coronary angiography was performed. A standard protocol for coronary angiography (128×0.6 mm slice collimation, 0.28 sec rotation time, 120 kVp tube voltage, 320 mA tube current) was followed.
A dual injector (Medrad, Pittsburgh, PA, USA) was used to inject a nonionic contrast agent (Iomeron 400, 400 mg/Ml; Braccon, Milan, Italy), and images were obtained. Segment thickness and intervals were set at 0.75 mm and 0.5 mm, respectively for image reformatting. An experienced radiology specialist checked for the presence of atherosclerotic plaques in the coronary arteries with the naked eye after the images were reformatted in three-dimensional Workstation. Subjects were diagnosed with atherosclerotic plaques in the coronary arteries if plaques were detected in CT-angiograms.
5. Statistics
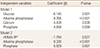
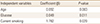
The mean, standard deviation or proportions (%) were calculated according to the characteristics of the variables. The interquartile range (25%-75%) was indicated for variables that were not normally distributed. Variables that were determined to be non-normally distributed after a Kolmogorov-Smirnov test were log-transformed before analysis. The Independent t-test, χ2 test, or the Mann–Whitney U-test were used depending on the characteristics of the variables to analyze for the differences between men and women. To study the correlation between serum osteocalcin levels and other variables, the Pearson correlation coefficient was used. To look for an independent relationship between serum osteocalcin concentration and other variables, a stepwise multiple regression analysis was performed; serum osteocalcin levels was the dependent variable, and other parameters were the independent variables.
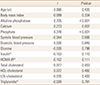
To compare the variables between subjects with and those without arteriosclerotic plaques in the coronary arteries, independent t-test, χ2 test, and Mann–Whitney U-test were performed. Logistic regression analysis was used, with the presence of atherosclerotic plaques set as the dependent variable. For the statistical analyses, the MedCalc version 16.4.3 Program (MedClac Software, Mariakerke, Belgium) was used, and the level of significance was set at below 0.05.
DISCUSSION
Osteocalcin concentrations reflect the rate of bone formation and the treatment for osteoporosis such as bisphosphonate change the osteocalcin levels.[
12] ALP is also a useful index for monitoring changes in bone turnover.[
13] Plasma ALP concentration mostly originates from the bones and the liver and especially bone-specific ALP reflects osteoblast activity.[
14]
In this study, serum osteocalcin levels showed a significant correlation with ALP, calcium, and phosphorus concentration. This is a predictable result, considering osteocalcin is a bone turnover marker.
Although there was no significant difference in serum osteocalcin levels between men and women, significantly higher osteocalcin levels were observed in postmenopausal women than premenopausal women. A previous study showed decreased osteocalcin concentration with increased age, but osteocalcin levels showed an increasing trend in postmenopausal women and men over the age of 70.[
15]
On multiple regression analysis, serum osteocalcin level showed negative correlation with fasting blood glucose and HOMA-IR after adjusting for age, sex, and menopausal status and this correlation was independent with ALP, calcium, and phosphorus concentration. This result shows that osteocalcin might be related to glucose metabolism and insulin resistance independently from its role as a bone turnover marker that reflects the rate of bone formation.
Many clinical studies have reported that a reduction in serum osteocalcin is related to increased incidences of high blood glucose, insulin resistance, obesity, metabolic syndrome and has important role in energy metabolism.[
4516171819] In this study, we found fasting blood glucose and insulin resistance were related to osteocalcin concentration. In contrast, BMI, history of diabetes, hyperlipidemia, high blood pressure, and plasma lipid concentration were not related to osteocalcin concentration. It is possible that there were not enough study subjects to reveal a correlation. Although both cardiovascular diseases and osteoporosis are diseases whose prevalence increases with age, bone mineral density was shown in previous studies to be inversely correlated to the advanced atherosclerosis and mortality, even after adjusting for age.[
2021]
Lately, osteocalcin has been gaining attention as a connecting factor between cardiovascular diseases and bone metabolism, and numerous cross-sectional studies and longitudinal studies have shown that a decrease in serum osteocalcin level is associated with increased rates of cardiovascular diseases. A prospective 10-year cohort study involving 774 men reported that the group with high serum osteocalcin concentration had the lowest rate of calcification in the abdominal aorta, and also the lowest death rate.[
22] In a cross-sectional study with 461 Chinese subjects, the group diagnosed with atherosclerotic plaques detected though angiography had increased osteocalcin concentration compared to the group without atherosclerotic plaques even after adjusting for cardiovascular risk factors.[
23]
A recent cross-sectional study with Korean subjects also reported that undercarboxylated osteocalcin concentrations, as well as the ratio between under-carboxylated osteocalcin and total osteocalcin concentration, were independently associated with known risk factors of cardiovascular diseases and bone density, and were negatively correlated with coronary calcification in men.[
6]
No definite mechanism shows a clear correlation between osteocalcin levels and cardiovascular diseases. However, cardiovascular calcification is one of the pathological changes of cardiovascular diseases, and an imbalance in osteocalcin concentration and cardiovascular mineralization may induce such changes.[
24] Some endothelial progenitor cells involved in ischemic tissue regeneration can secrete osteocalcin, and although a recent study has reported that osteocalcin-secreting endothelial progenitor cells are related to unstable coronary heart disease, the role of these cells in the occurrence of arteriosclerosis is still unclear.[
25]
In this study, the serum osteocalcin levels were not significantly different between subjects with and those without arteriosclerotic plaques in the coronary arteries.
The conflicting results of this study compared to the above mentioned studies may be caused from the difference of method to diagnose coronary atherosclerosis. In this study, we used coronary MDCT angiography to reveal relationship between the presence of coronary atherosclerotic plaques and osteocalcin concentration. MDCT can detect both calcified and non-calcified plaque compared to coronary calcification score as surrogate marker of atherosclerosis used in above mentioned similar study.[
6]
However, the limitations of this study could be the reason of the discordance. The limitations of this study are: 1) small sample size. 2) The limitations of retrospective analyses of medical records. 3) Possible existence of selection bias, as the subjects only included people who visited the health examination centers. 4) In this study, only the total osteocalcin concentration was measured, and the ratio of carboxylation of osteocalcin and the concentration of vitamin K were not taken into account; this may have contributed to the lack of significant differences in osteocalcin level according to the presence of coronary atherosclerotic plaques. In the blood, osteocalcin is found in two forms: carboxylated osteocalcin, which is mainly involved in bone mineralization, and undercarboxylated osteocalcin, which is mainly involved in energy metabolism and controlled by vitamin K concentration.[
2326] Osteocalcin reflects bone turnover and bone density; bone density and atherosclerosis share various mutual risk factors such as age, smoking, menopause, diet, exercise, and physical activity. It is possible that the data were not adjusted enough for these confounding variables; thus, we might not be able to observe any difference in osteocalcin concentration between the groups.
However, a few cohort studies have reported an absent correlation between osteocalcin and the incidence of cardiovascular diseases.[
10] Similarly, a cross-sectional study has reported that osteocalcin concentration in postmenopausal women was positively correlated with the prevalence of coronary atherosclerosis, contrary to the results of previous studies.[
27] There has also been a report that in both healthy men and premenopausal and postmenopausal women, osteocalcin has no independent correlation with the carotid intima-media thickness.[
28] Therefore, osteocalcin concentration may have a miniscule or limited impact on the development of atherosclerosis.
A prospective study that was carried out for five years and involved 3,522 elderly men reported that serum osteocalcin levels may be used to predict the mortality rate of cardiovascular diseases at both low and high concentrations, resulting in a U-shaped relationship.[
29] Another cohort study with 1,319 subjects reported that the higher the concentration of osteocalcin, the lower the risk for cardiovascular diseases in men, and the higher the risk in women.[
30] Therefore, the relationship between osteocalcin and cardiovascular disease risks may vary depending on gender, race, and the characteristics of a subject group.
In conclusion, serum osteocalcin level was inversely associated with fasting glucose level and insulin resistance measured by HOMA-IR, suggesting that osteocalcin is important for glucose metabolism. However, in this study, no significant difference was observed in the serum osteocalcin level according to the presence of coronary atherosclerotic plaques.
It would be necessary to assess the clinical significance of osteocalcin through large-scale prospective studies involving diverse groups of subjects.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download