Abstract
Background
The physician's hands are close to the X-ray field in C-arm fluoroscopy-guided pain interventions. We prospectively investigated the radiation attenuation of Proguard RR-2 gloves.
Methods
In 100 cases, the effective doses (EDs) of two dosimeters without a radiation-reducing glove were collected. EDs from the two dosimeters-one dosimeter wrapped with a glove and the other dosimeter without a glove- were also measured at the side of the table (Group 1, 140 cases) and at a location 20 cm away from the side of the table (Group 2, 120 cases). Mean differences such as age, height, weight, radiation absorbed dose (RAD), exposure time, ED, and ratio of EDs were analyzed.
Results
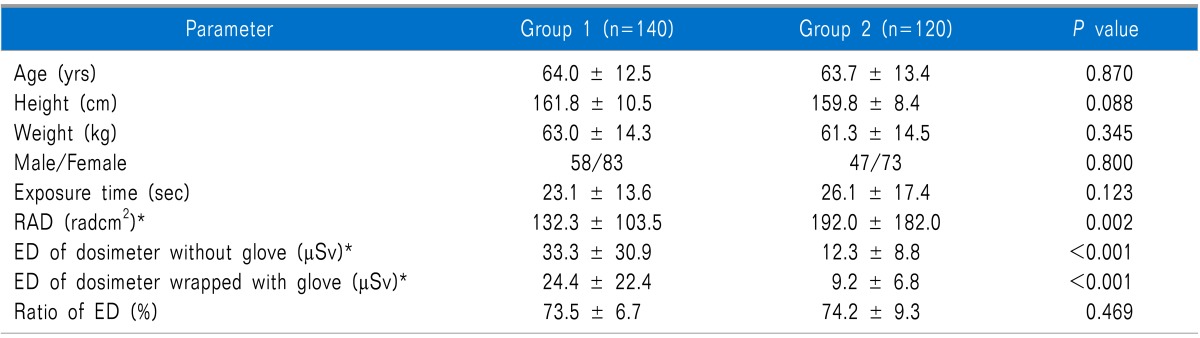
In the EDs of two dosimeters without gloves, there were no significant differences (39.0 ± 36.3 µSv vs. 38.8 ± 36.4 µSv) (P = 0.578). The RAD (192.0 ± 182.0 radcm2) in Group 2 was higher than that (132.3 ± 103.5 radcm2) in Group 1 (P = 0.002). The ED (33.3 ± 30.9 µSv) of the dosimeter without a glove in Group 1 was higher than that (12.3 ± 8.8 µSv) in Group 2 (P < 0.001). The ED (24.4 ± 22.4 µSv) of the dosimeter wrapped with a glove in Group 1 was higher than that (9.2 ± 6.8 µSv) in Group 2 (P < 0.001). No significant differences were noted in the ratio of EDs (73.5 ± 6.7% vs. 74.2 ± 9.3%, P = 0.469) between Group 1 and Group 2.
There are several radiation protective utilities, including caps, eyewear, thyroid shields, aprons, gloves, lead barriers, and table-side lead drapes. In previous studies, radiation-protective aprons and thyroid shields have been found to be the most widely used utilities for radiation safety [1,2]. However, the physician's hand is very close to the direct X-ray field in C-arm fluoroscopy-guided pain interventions. In some cases such as cervical nucleoplasty or cervical discography, the hand or fingers can be located on the direct X-ray field. Therefore, radiation protection of the hand is necessary [3]. According to the instructions on the package of Proguard RR-2 gloves (Emerson & Co, Genoa, Italy), the attenuation properties of the gloves are 31-55% (the attenuation properties are changed by peak kilovoltages [kVp]; for example, there is 55% attenuation at 60 kVp and 31% attenuation at 120 kVp) in primary X-ray beams. However, pain physicians do not use the gloves only in primary X-ray beams. Therefore the attenuation rate does not exactly describe the radiation-protective efficiency for pain physicians. In C-arm fluoroscopy-guided pain interventions, there have been no previous studies of the radiation-protective efficiency of radiation-reducing gloves. The pain physician can be exposed to radiation of primary X-ray beams by having his hand in the X-ray field or may be exposed to scatter radiation from the patient even by not having his hand in the X-ray field [3,4]. The most significant source of radiation exposure for the pain physician is scatter radiation [1,4,5]. We prospectively investigated the scatter radiation attenuation of Proguard RR-2 gloves.
We performed a prospective study regarding the radiation-protective efficiency of radiation-reducing gloves in C-arm fluoroscopy-guided pain interventions from March to June of 2013. Two dosimeters (PDM-127, Hitachi Aloka Medical, Ltd., Tokyo, Japan, and PDM-227, Hitachi Aloka Medical, Ltd.) were used to estimate the effective dose (ED). C-arm fluoroscopy-guided pain interventions included medial branch block, facet joint injection, transforaminal epidural steroid injection, root block, interlaminar epidural steroid injection, caudal epidural steroid injection, sympathetic ganglion block, and radiofrequency treatment, among others.
First, we compared the radiation-protective efficiency of the two dosimeters. The two dosimeters, without wrapping of a radiation-reducing glove, were placed beside the table (Fig. 1). The dosimeters were maintained the same distance from the center of the X-ray field. In 100 cases of C-arm fluoroscopy-guided procedure, the EDs of the two dosimeters were collected.
To investigate the radiation-protective efficiency of the gloves, new radiation-reducing gloves were used in this study. The wrist area of a new glove was cut into a 9 by 6 cm rectangle. The cut piece was wrapped around one of the dosimeters to investigate the radiation-protective efficiency of the glove. Only one layer of the piece totally covered the radiation sensor of the dosimeter. The EDs from the two dosimeters were measured at the side of the table (Group 1) and at a location 20 cm away from the side of the table (Group 2) (Fig. 1, 2). The distance from the center of the X-ray field to the dosimeter was 28 cm in Group 1 and 48 cm in Group 2. To maintain the same distance from the center of the X-ray field to the dosimeter, the dosimeters were moved in the cephalic or caudal direction with C-arm fluoroscopy. In Group 1, the PDM-127 dosimeter was wrapped with a radiation-reducing glove in 70 procedures and the PDM-227 dosimeter was wrapped with a glove in an additional 70 procedures. In Group 2, the PDM-127 dosimeter was wrapped with a glove in 60 procedures and the PDM-227 dosimeter was wrapped with a glove in an additional 60 procedures. EDs from the dosimeters, exposure times, and the radiation absorbed doses (RADs) from the C-arm fluoroscope (OEC 9800 Plus, GE Healthcare, Salt Lake City, UT, USA), as well as the ratio of the ED from the dosimeter wrapped with a glove to the ED from the dosimeter without a glove were collected in each procedure. Data regarding patients' age, height, weight, and sex were collected by review of medical records.
According to the instructions, the accuracy of the PDM-127 and PDM-227 dosimeters is within ± 10% from 10 µSv to 1 Sv. Therefore, the maximum discrepancy of two dosimeters can be 20%. In our 30 cases of pilot study, the ratio of the EDs was 73.1% in Group 1 and 74.4% in Group 2. We suggested that the ratio of the EDs was the same between Group 1 and Group 2 and the difference of the ratio of EDs from the dosimeters between the two groups was within 20%. To obtain 90% power for analysis, 83 cases were required in each group.
The mean differences in data such as age, height, weight, RAD, exposure time, ED, and ratio of EDs were analyzed using the Student's t-test. The male/female ratio was analyzed by the chi-square test. To investigate the RAD-adjusted comparison, the ED and the ratio of EDs were evaluated by analysis of covariance (ANCOVA). Statistical significance was defined as P < 0.05.
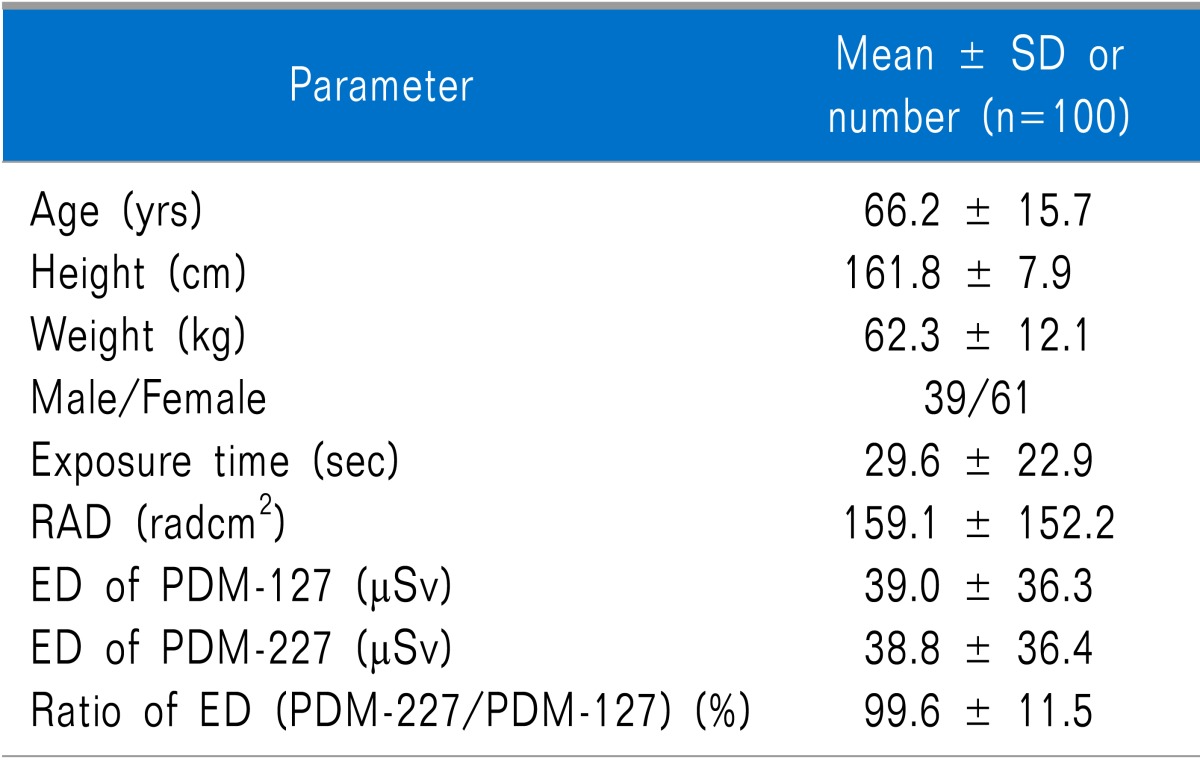
Data were collected from 360 cases of C-arm fluoroscopy-guided pain interventions. In 100 cases related to the EDs of two dosimeters without radiation-reducing gloves, there were no significant differences between the ED of PDM-127 (39.0 ± 36.3 µSv) and the ED of PDM-227 (38.8 ± 36.4 µSv) (P = 0.578). The patients' data in the 100 cases is indicated in Table 1.
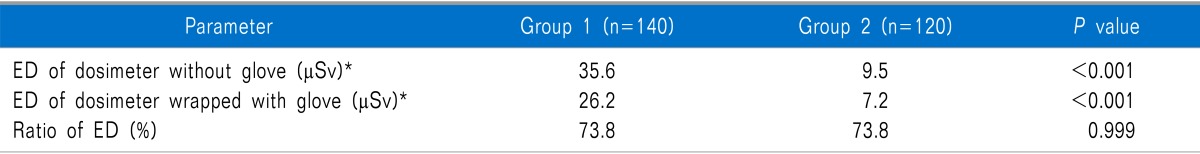
No significant differences were noted in the patients' demographic data (age [64 ± 12.5 vs. 63.7 ± 13.4 yrs, P = 0.870], height [161.8 ± 10.5 cm vs. 159.8 ± 8.4 cm, P = 0.088], weight [63.0 ± 14.3 kg vs. 61.3 ± 14.5 kg, P = 0.345] and male/female ratio [P = 0.800]), exposure time (23.1 ± 13.6 sec vs. 26.1 ± 17.4 sec, P = 0.123) and ratio of EDs (73.5 ± 6.7% vs. 74.2 ± 9.3%, P = 0.469) between Group 1 and Group 2 (Table 2). The RAD (192.0 ± 182.0 radcm2) in Group 2 was higher than that (132.3 ± 103.5 radcm2) in Group 1 (P = 0.002). The ED (33.3 ± 30.9 µSv) of the dosimeter without a glove in Group 1 was higher than that (12.3 ± 8.8 µSv) in Group 2 (P < 0.001). The ED (24.4 ± 22.4 µSv) of the dosimeter wrapped with a glove in Group 1 was higher than that (9.2 ± 6.8 µSv) in Group 2 (P < 0.001). The RAD-adjusted mean ED without a glove was 35.6 µSv (95% confidence interval [CI]: 32.3-39.0 µSv) in Group 1 and 9.5 µSv (95% CI: 5.9-13.2 µSv) in Group 2 (P < 0.001) (Table 3). The RAD-adjusted mean ED with a wrapped glove was 26.2 µSv (95% CI: 23.7-28.6 µSv) in Group 1 and 7.2 µSv (95% CI: 4.5-9.8 µSv) in Group 2 (P < 0.001). The RAD-adjusted ratio of the EDs was 73.8% (95% CI: 72.5-75.1%) in Group 1 and 73.8% (95% CI: 72.4-75.3%) in Group 2 (P = 0.999).
In this study, the mean ratio of the EDs was 73.5% in Group 1 and 74.2% in Group 2 (Table 2). This finding shows that Proguard RR-2 gloves decreased the scatter radiation by 26.5% in Group 1 and 25.8% in Group 2. In this study design, we wanted to know whether the different intensities of scatter radiation affect the radiation attenuation of the gloves or not. The distance from the center of the X-ray field to the dosimeter in Group 2 was 20 cm longer than that in Group 1. In our results, the mean ED from the dosimeter without a glove in Group 2 was 36.9% of that in Group 1. In spite of the decreased scatter radiation in Group 2, the radiation attenuation powers (ratio of EDs) of the gloves in Group 1 and Group 2 were not different. The RAD in Group 2 was higher than that in Group 1 (Table 2). These results suggested that the ratio of radiation attenuation by the Proguard RR-2 gloves is not significantly different by the different intensity of scatter radiation or the different RAD of C-arm fluoroscopy.
If the RADs were the same in the groups, the difference of the EDs between Group 1 and Group 2 might be higher. To remove the effect of different RADs in the groups, ANCOVA was used. The RAD-adjusted ED from the dosimeter without a glove in Group 2 was 26.7% of that in Group 1 (Table 3). This shows that a lengthened distance of only 20 cm from the side of the table can reduce the scatter radiation by 73.3%. In this study, a 20 cm longer distance (26.7% of radiation exposure at the side of the table) was a more effective method of radiation protection than the use of radiation-reducing gloves (73.8% of radiation exposure at the side of the table). The radiation is inversely proportional to the square of the distance from the radiation source [6]. Therefore, the method of pulling back the physician's hands can be a very effective and economic method of radiation safety. However, the method of pulling back the hands is not possible in some cases. In cases such as holding a needle during a procedure, the physician's hand is located in the primary X-ray field or near the X-ray field. In these cases, radiation-reducing gloves are a good choice for radiation safety for the physician's hands. Although radiation-reducing gloves are relatively expensive, the decrease of radiation exposure by the use of the gloves can be valuable for the physician's health. The use of radiation-reducing gloves and the location of the hand at 20 cm away from the side of the table can be more effective and can decrease the radiation exposure of the pain physician's hand by 20.2% (Table 3). Interestingly, the RAD-adjusted ratios of EDs from the dosimeters in Group 1 and Group 2 were almost the same, at 73.8% (Table 3). This means that if the RADs of the two groups were the same, the ratios of the EDs of the two groups-their distances from the radiation center to the dosimeter were different-were also the same.
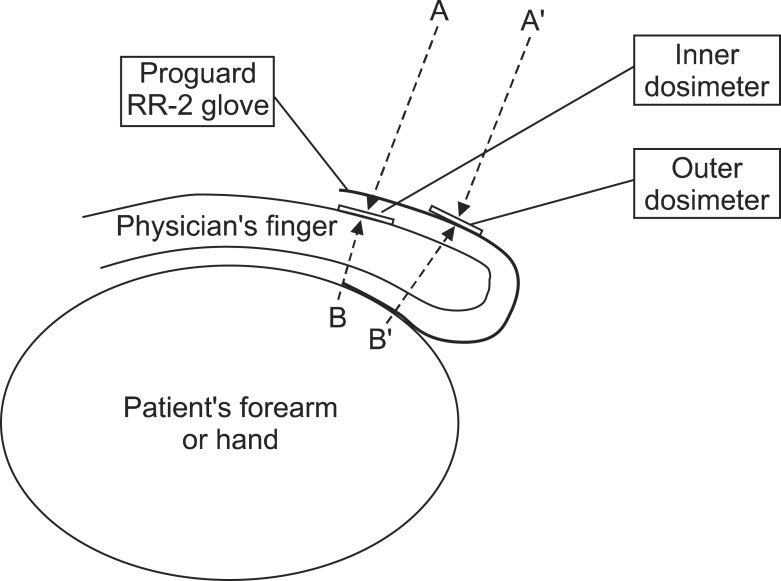
In this study, the Proguard RR-2 gloves provide a radiation attenuation of 25.8-26.5% against scatter radiation. This figure is much lower than the data from an in vitro study, according to the instructions on the package of the Proguard RR-2 gloves (55% attenuation at 60 kVp and 31% attenuation at 120 kVp), and also differs from the radiation attenuation of 60-64% against scatter radiation in a previous study [7]. In this study, according to Calder et al. [7], the surgeon was holding the patients' forearms and hands in his hands and the hands were placed at the side of the image intensifier. It is thought that the radiation attenuation of 60-64% is not the exact radiation-protective efficiency of the gloves. Radiation-protective aprons which are 0.25-0.35 mmPb equivalent thickness provide a radiation attenuation effect up to 90-95% [8]. However, Proguard RR-2 gloves probably could not provide 60% of radiation attenuation, because their Pb equivalent thickness is only 0.022 mm (the gloves are only 6.3-8.8% of the Pb equivalent thickness of the apron). In Calder's study, there could be scatter radiation from several directions. Fig. 3 provides a schematic diagram of Calder's study. In Fig. 3, the authors suggested that the outer dosimeter sensed direct scatter radiation (they thought there was no attenuation) and the inner dosimeter sensed attenuated scatter radiation by one layer of Proguard RR-2 gloves. If there was only one direction of scatter radiation, such as A and A', their suggestion was true. However, we thought there were at least two directions of scatter radiation, such as A and B. Scatter radiation is made by ricocheting radiation from the patient's body, the table, and/or other obstacles to the primary X-ray beam [1,4,5]. Therefore, some scatter radiation might reach from the patient's forearm or hand, such as B and B'. B reached the inner dosimeter through one layer of radiation-reducing glove and the physician's finger. B' reached the outer dosimeter through two layers of radiation-reducing glove and the physician's finger. Therefore, the authors' suggestion was not true. The outer dosimeter sensed not only primary scatter radiation but also attenuated scatter radiation by two layers of gloves. The inner dosimeter also sensed not only attenuated scatter radiation through one layer of glove but also attenuated radiation through one layer of glove and the physician's finger. Therefore, the ED from the outer dosimeter could be lower than the true primary scatter radiation, and the radiation attenuation of 60-64% is higher than our results. In our study, the sensors of the dosimeters were facing the patient's body (Fig. 1) and there was no adjacent obstacle behind the dosimeters. Therefore, it was almost impossible that there was scatter radiation which was coming behind.
Arnstein et al. [9] showed that the dose to the surgeon's hands in the primary beam was 100 times that which was measured at 15 cm from the source. In the typical position of the operator, the dose to the hands, without the ceiling-suspended shields, ranged from 0.2 to 7.3 µSv frame-1 depending on the beam projection [10]. The dose is not so high, but a large number of pain physicians use several frames of C-arm fluoroscopy in each pain intervention, and many procedures are performed each day [1,3,11,12]. According to the dose intensity, the accumulation of radiation exposure may be high dose for several years. The International Commission on Radiological Protection (ICRP) recommended annual permissible dose for hands and feet related to occupational exposure is 500 mSv [13]. However, the National Council on Radiation Protection and Measurement (NCRP) recommended occupational dose limit of the whole body is 10 mSv per year for a lifetime [13]. Most importantly, nobody knows the exact threshold of radiation exposure which is related to cancer or genetic defects in humans [14,15]. Therefore, pain physicians who perform C-arm fluoroscopy-guided pain interventions need to try to reduce their radiation exposure. Miller et al. indicated that the head, neck, and hands were at greatest risk to radiation [16]. Although there exists the possibility of high radiation exposure of the hands [3], the rate of glove use among pain physicians was low in a Korean study [1]. Lead and lead-equivalent gloves have been suggested to attenuate direct-beam and scatter radiation effectively [7,17].
Many studies have emphasized the importance of more systemic monitoring of the doses to the most vulnerable body parts of radiation for the practitioner involved in such procedures [18,19,20,21]. Even though the estimated annual doses are found to be well below the limits, additional measures such as careful beam collimation and the use of automatic contrast media injector could reduce the doses significantly [10]. Arnstein et al. [9] recommended coning down of the image, avoidance of the primary beam, and the use of a remote-positioning device. For effective radiation protection, practitioners should use radiation protection devices such as aprons, thyroid shields, radiation protective glasses, and radiation-reducing gloves routinely [6,22], and also employ primary protection strategies. The protection strategies are to minimize fluoroscopy time, to minimize the number of fluoroscopic images, to use low dose or pulsed mode, to use collimation, to use good-imaging chain geometry, to position oneself a long distance from radiation sources, to use protective shielding, to wear one's own dosimeter, and to know one's own dose [3,6,11,22,23].
There are some limitations in this study. First, the dosimeters could have detectable errors. The accuracy of the two dosimeters was known as within ± 10%. The accuracy could be biased in this study. However, the EDs of the two dosimeters without gloves showed no significant differences. Therefore, any bias might be small. Second, we compared the EDs of two groups measured at the side of the table and at a location 20 cm away from the side of the table. The results showed that the distance was not correlated with the radiation attenuation effect of the gloves. However, we compared the ratio of EDs in only two positions. If data could be collected in more than two positions, the results could be more trusted. In two groups, the RADs were different. The different RADs might influence the results. However, the RAD-adjusted comparison by ANCOVA was analyzed in this study. The results were not significantly different from the results of the Student's t-test.
In conclusion, Proguard RR-2 gloves possess 25.8-26.5% of radiation attenuation effect. The radiation attenuation by the Proguard RR-2 gloves is not significantly different by the intensity of scatter radiation or the different RADs of C-arm fluoroscopy. A 20 cm longer distance from the side of the table can be a more effective method of radiation protection than the use of radiation-reducing gloves; thus, the method of pulling back the physician's hands can be a very effective and economic method of radiation safety. The combination use of radiation-reducing gloves and positioning the hands at 20 cm away from the table can decrease radiation exposure much more effectively.
References
1. Park PE, Park JM, Kang JE, Cho JH, Cho SJ, Kim JH, et al. Radiation safety and education in the applicants of the final test for the expert of pain medicine. Korean J Pain. 2012; 25:16–21. PMID: 22259711.

2. Kim C, Vasaiwala S, Haque F, Pratap K, Vidovich MI. Radiation safety among cardiology fellows. Am J Cardiol. 2010; 106:125–128. PMID: 20609659.

3. Jung CH, Ryu JS, Baek SW, Oh JH, Woo NS, Kim HK, et al. Radiation exposure of the hand and chest during C-arm fluoroscopy-guided procedures. Korean J Pain. 2013; 26:51–56. PMID: 23342208.

4. Fink GE. Radiation safety in fluoroscopy for neuraxial injections. AANA J. 2009; 77:265–269. PMID: 19731844.
5. Schueler BA. Operator shielding: how and why. Tech Vasc Interv Radiol. 2010; 13:167–171. PMID: 20723831.

6. Ryu JS, Baek SW, Jung CH, Cho SJ, Jung EG, Kim HK, et al. The survey about the degree of damage of radiation-protective shields in operation room. Korean J Pain. 2013; 26:142–147. PMID: 23614075.

7. Calder PR, Tennent TD, Allen PW. Assessment of the efficacy of Proguard RR-2 radio-protective gloves during forearm manipulation. Injury. 2003; 34:159–161. PMID: 12565026.

8. Mori H, Koshida K, Ishigamori O, Matsubara K. Evaluation of the effectiveness of X-ray protective aprons in experimental and practical fields. Radiol Phys Technol. 2014; 7:158–166. PMID: 24338033.

9. Arnstein PM, Richards AM, Putney R. The risk from radiation exposure during operative X-ray screening in hand surgery. J Hand Surg Br. 1994; 19:393–396. PMID: 8077836.

10. Koukorava C, Carinou E, Simantirakis G, Vrachliotis TG, Archontakis E, Tierris C, et al. Doses to operators during interventional radiology procedures: focus on eye lens and extremity dosimetry. Radiat Prot Dosimetry. 2011; 144:482–486. PMID: 21044993.

11. Baek SW, Ryu JS, Jung CH, Lee JH, Kwon WK, Woo NS, et al. A randomized controlled trial about the levels of radiation exposure depends on the use of collimation C-arm fluoroscopic-guided medial branch block. Korean J Pain. 2013; 26:148–153. PMID: 23614076.

12. Hernández García JM, Vidal Marcos A, Gasco García C. A survey on the use of fluoroscopy in the treatment of pain: do we perform it correctly? Rev Esp Anestesiol Reanim. 2012; 59:430–435. PMID: 22824536.
13. Rehani MM, Ciraj-Bjelac O, Vañó E, Miller DL, Walsh S, Giordano BD, et al. ICRP Publication 117. Radiological protection in fluoroscopically guided procedures performed outside the imaging department. Ann ICRP. 2010; 40:1–102. PMID: 22732420.

14. Albert JM. Radiation risk from CT: implications for cancer screening. AJR Am J Roentgenol. 2013; 201:W81–W87. PMID: 23789701.

15. Shah DJ, Sachs RK, Wilson DJ. Radiation-induced cancer: a modern view. Br J Radiol. 2012; 85:e1166–e1173. PMID: 23175483.

16. Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983; 65:1–4. PMID: 6848524.

17. Back DL, Hilton AI, Briggs TW, Scott J, Burns M, Warren P. Radiation protection for your hands. Injury. 2005; 36:1416–1420. PMID: 16051240.

18. Sanchez R, Vano E, Fernandez JM, Gallego JJ. Staff radiation doses in a real-time display inside the angiography room. Cardiovasc Intervent Radiol. 2010; 33:1210–1214. PMID: 20694467.

19. Luchs JS, Rosioreanu A, Gregorius D, Venkataramanan N, Koehler V, Ortiz AO. Radiation safety during spine interventions. J Vasc Interv Radiol. 2005; 16:107–111. PMID: 15640417.

20. Detorie N, Mahesh M, Schueler BA. Reducing occupational exposure from fluoroscopy. J Am Coll Radiol. 2007; 4:335–337. PMID: 17467618.

21. Vano E, Kleiman NJ, Duran A, Romano-Miller M, Rehani MM. Radiation-associated lens opacities in catheterization personnel: results of a survey and direct assessments. J Vasc Interv Radiol. 2013; 24:197–204. PMID: 23369556.

22. Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R, et al. Cardiovscular and Interventional Radiology Society of Europe. Society of Interventional Radiology. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc Intervent Radiol. 2010; 33:230–239. PMID: 20020300.

23. Cho JH, Kim JY, Kang JE, Park PE, Kim JH, Lim JA, et al. A study to compare the radiation absorbed dose of the C-arm fluoroscopic modes. Korean J Pain. 2011; 24:199–204. PMID: 22220241.

Fig. 1
Study diagram and position of dosimeters in each group (arrow: scatter radiation). A: position of dosimeters at side of table. B: position of dosimeters at 20 cm away from side of table.
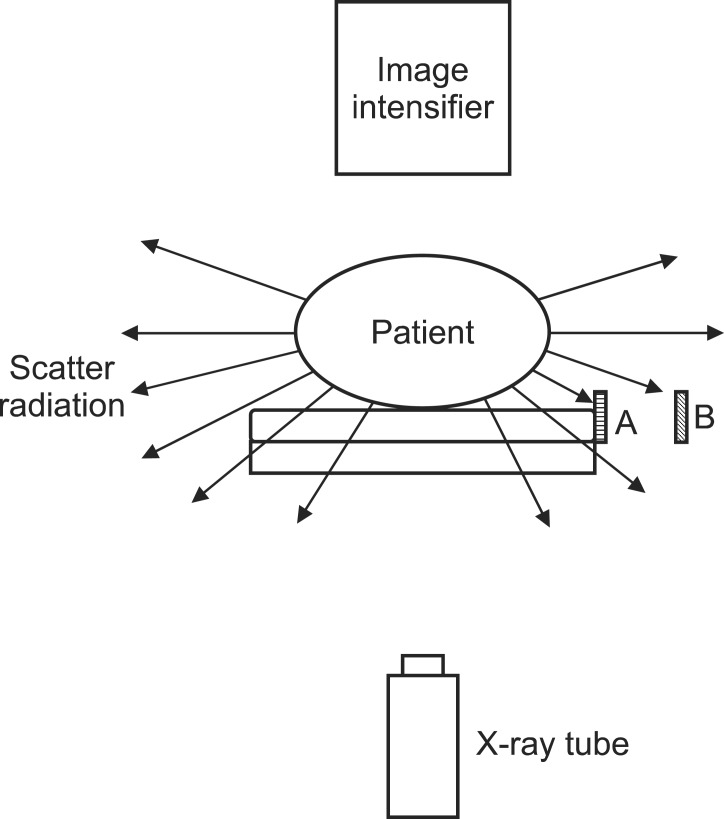
Fig. 2
The position of the two dosimeters at the side of the table. One dosimeter was wrapped with a radiation-reducing glove. Only one layer of the piece totally covered the radiation sensor of the dosimeter. Sensors were facing the patient and table.
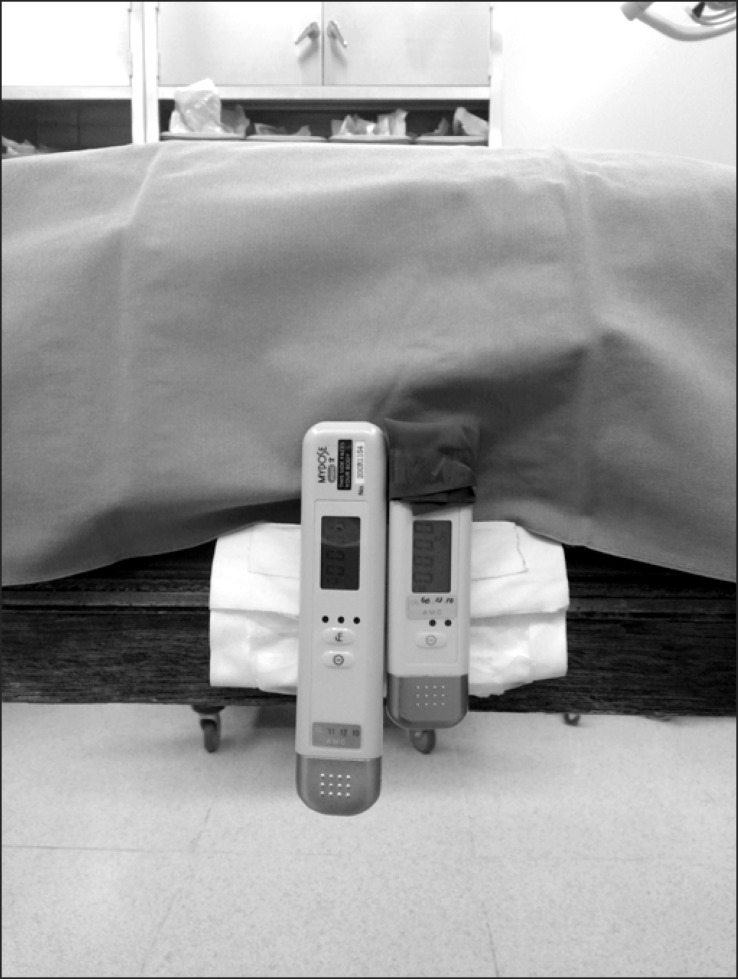
Fig. 3
Schematic diagram of Calder et al.'s [7] study (dotted arrow: scatter radiation). A: attenuated scatter radiation through one layer of radiation-reducing gloves. B: attenuated scatter radiation through one layer of radiation-reducing glove and physician's finger. A': direct scatter radiation. B': attenuated scatter radiation through two layers of radiation-reducing glove and physician's finger.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download