1. Rennard S, Thomashow B, Crapo J, Yawn B, McIvor A, Cerreta S, et al. Introducing the COPD foundation guide for diagnosis and management of COPD, recommendations of the COPD foundation. COPD. 2013; 10(3):378–389. PMID:
23713598.
2. Stanojevic S, Kaminsky DA, Miller MR, Thompson B, Aliverti A, Barjaktarevic I, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2022; 60(1):2101499. PMID:
34949706.
3. Haynes JM, Kaminsky DA, Stanojevic S, Ruppel GL. Pulmonary function reference equations: a brief history to explain all the confusion. Respir Care. 2020; 65(7):1030–1038. PMID:
32156791.
4. Hulo S, de Broucker V, Giovannelli J, Cherot-Kornobis N, Nève V, Sobaszek A, et al. Global Lung Function Initiative reference equations better describe a middle-aged, healthy French population than the European Community for Steel and Coal values. Eur Respir J. 2016; 48(6):1779–1781. PMID:
27540022.
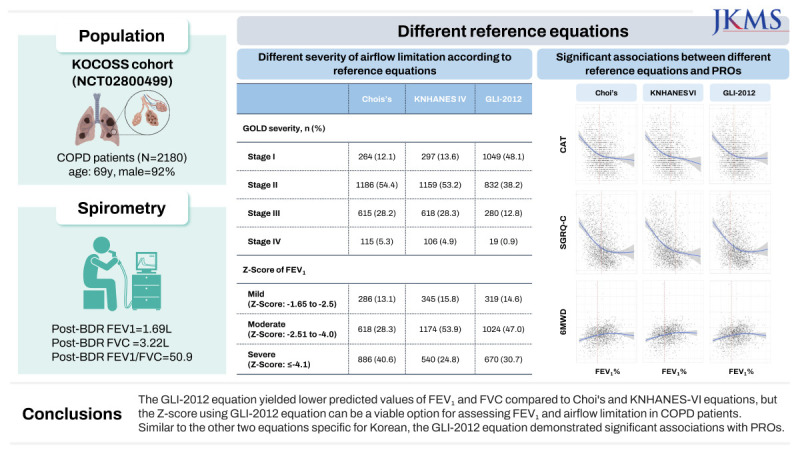
5. Choi HS, Park YB, Yoon HK, Lim SY, Kim TH, Park JH, et al. Validation of previous spirometric reference equations and new equations. J Korean Med Sci. 2019; 34(47):e304. PMID:
31808325.
6. Bhakta NR, Bime C, Kaminsky DA, McCormack MC, Thakur N, Stanojevic S, et al. Race and ethnicity in pulmonary function test interpretation: an official American thoracic society statement. Am J Respir Crit Care Med. 2023; 207(8):978–995. PMID:
36973004.
7. NCD Risk Factor Collaboration (NCD-RisC). A century of trends in adult human height. Elife. 2016; 5:e13410. PMID:
27458798.
8. Yang YS, Han BD, Han K, Jung JH, Son JW. Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31(2):169–177. PMID:
35770450.
9. Cole TJ, Mori H. Fifty years of child height and weight in Japan and South Korea: contrasting secular trend patterns analyzed by SITAR. Am J Hum Biol. 2018; 30(1):e23054. PMID:
28833849.
10. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis (Seoul). 2005; 58(3):230–242.
11. Chang Y, Kim HC, Jo KW, Lee JS, Oh YM, Lee SD, et al. Analysis of high predicted pulmonary function: possibility of overestimation in small elderly examinees. Korean J Intern Med. 2020; 35(1):142–149. PMID:
31610631.
12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370(9596):1453–1457. PMID:
18064739.
13. Lee JY, Chon GR, Rhee CK, Kim DK, Yoon HK, Lee JH, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical center in Korea: The KOrea COpd subgroup study team cohort. J Korean Med Sci. 2016; 31(4):553–560. PMID:
27051239.
14. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Updated 2023. Accessed October 30, 2023.
http://www.goldcopd.org/
.
15. Mannino DM, Reichert MM, Davis KJ. Lung function decline and outcomes in an adult population. Am J Respir Crit Care Med. 2006; 173(9):985–990. PMID:
16439715.
16. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012; 22(3):276–282. PMID:
23092060.
17. Stanojevic S, Wade A, Stocks J. Reference values for lung function: past, present and future. Eur Respir J. 2010; 36(1):12–19. PMID:
20595163.
18. Miller MR, Quanjer PH, Swanney MP, Ruppel G, Enright PL. Interpreting lung function data using 80% predicted and fixed thresholds misclassifies more than 20% of patients. Chest. 2011; 139(1):52–59. PMID:
20522571.
19. Swanney MP, Ruppel G, Enright PL, Pedersen OF, Crapo RO, Miller MR, et al. Using the lower limit of normal for the FEV
1/FVC ratio reduces the misclassification of airway obstruction. Thorax. 2008; 63(12):1046–1051. PMID:
18786983.
20. Choi KY, Lee HJ, Lee JK, Park TY, Heo EY, Kim DK, et al. Rapid FEV
1/FVC decline is related with incidence of obstructive lung disease and mortality in general population. J Korean Med Sci. 2023; 38(1):e4. PMID:
36593688.
21. Lee HW, Lee HJ, Lee JK, Park TY, Heo EY, Kim DK. Rapid FEV
1 decline and lung cancer incidence in South Korea. Chest. 2022; 162(2):466–474. PMID:
35318007.
22. Huprikar NA, Holley AB, Skabelund AJ, Hayes JA, Hiles PD, Aden JK, et al. A comparison of global lung initiative 2012 with third national health and nutrition examination survey spirometry reference values. implications in defining obstruction. Ann Am Thorac Soc. 2019; 16(2):225–230. PMID:
30427734.
23. Fasola S, La Grutta S, Cibella F, Cilluffo G, Viegi G. Global Lung Function Initiative 2012 reference values for spirometry in South Italian children. Respir Med. 2017; 131:11–17. PMID:
28947016.
24. Park JS, Suh DI, Choi YJ, Ahn K, Kim KW, Shin YH, et al. Pulmonary function of healthy Korean children from three independent birth cohorts: validation of the Global Lung Function Initiative 2012 equation. Pediatr Pulmonol. 2021; 56(10):3310–3320. PMID:
34375041.
25. Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3−95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012; 40(6):1324–1343. PMID:
22743675.
26. Leong WY, Gupta A, Hasan M, Mahmood S, Siddiqui S, Ahmed S, et al. Reference equations for evaluation of spirometry function tests in South Asia, and among South Asians living in other countries. Eur Respir J. 2022; 60(6):2102962. PMID:
35896203.
27. Yap WS, Chan CC, Chan SP, Wang YT. Ethnic differences in anthropometry among adult Singaporean Chinese, Malays and Indians, and their effects on lung volumes. Respir Med. 2001; 95(4):297–304. PMID:
11316113.
28. Nakanishi Y, Nethery V. Anthropometric comparison between Japanese and Caucasian American male university students. Appl Human Sci. 1999; 18(1):9–11.
29. Lim U, Ernst T, Buchthal SD, Latch M, Albright CL, Wilkens LR, et al. Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes. 2011; 1(5):e6. PMID:
23449381.
30. Kakavas S, Kotsiou OS, Perlikos F, Mermiri M, Mavrovounis G, Gourgoulianis K, et al. Pulmonary function testing in COPD: looking beyond the curtain of FEV
1
. NPJ Prim Care Respir Med. 2021; 31(1):23. PMID:
33963190.
31. Lange P, Halpin DM, O'Donnell DE, MacNee W. Diagnosis, assessment, and phenotyping of COPD: beyond FEV
1
. Int J Chron Obstruct Pulmon Dis. 2016; 11 Spec Iss(Spec Iss):3–12. PMID:
26937185.
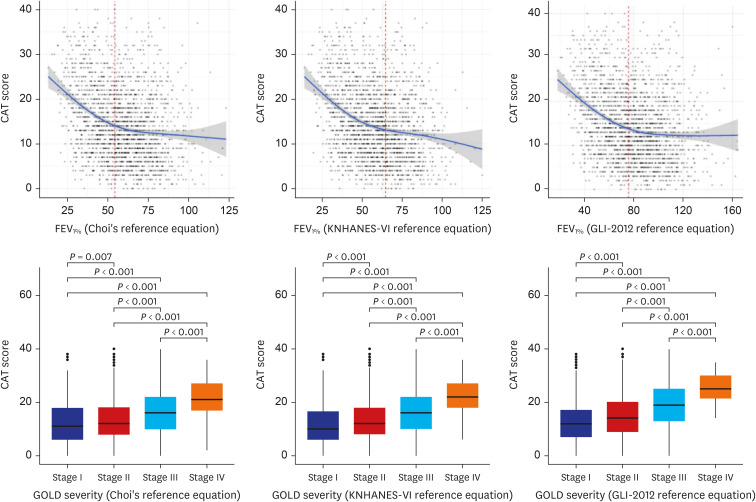
32. Miravitlles M, Koblizek V, Esquinas C, Milenkovic B, Barczyk A, Tkacova R, et al. Determinants of CAT (COPD assessment test) scores in a population of patients with COPD in central and Eastern Europe: the POPE study. Respir Med. 2019; 150:141–148. PMID:
30961941.
33. Ghobadi H, Ahari SS, Kameli A, Lari SM. The relationship between COPD assessment test (CAT) scores and severity of airflow obstruction in stable COPD patients. Tanaffos. 2012; 11(2):22–26. PMID:
25191410.
34. Tu YH, Zhang Y, Fei GH. Utility of the CAT in the therapy assessment of COPD exacerbations in China. BMC Pulm Med. 2014; 14(1):42. PMID:
24618290.
35. Huang WC, Wu MF, Chen HC, Hsu JY. TOLD Group. Features of COPD patients by comparing CAT with mMRC: a retrospective, cross-sectional study. NPJ Prim Care Respir Med. 2015; 25(1):15063. PMID:
26538368.
36. Lee HW, Lee JK, Lee MG, Shin KC, Ra SW, Kim TH, et al. Risk factors of rapid FEV
1 decline in a real-world chronic obstructive pulmonary disease cohort. Respiration. 2022; 101(12):1078–1087. PMID:
36349793.
37. Kostikas K, Greulich T, Mackay AJ, Lossi NS, Aalamian-Mattheis M, Nunez X, et al. Treatment response in COPD: does FEV
1 say it all? A
post hoc analysis of the CRYSTAL study. ERJ Open Res. 2019; 5(1):00243–2018. PMID:
30815470.
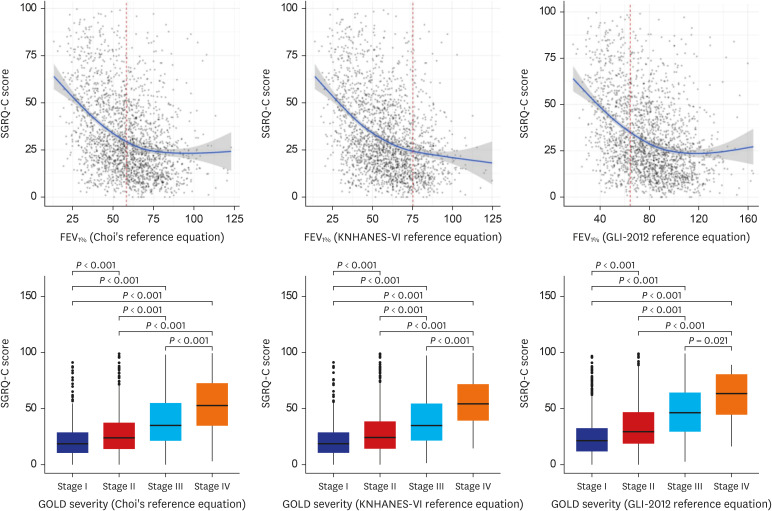
38. Weatherall M, Marsh S, Shirtcliffe P, Williams M, Travers J, Beasley R. Quality of life measured by the St George’s Respiratory Questionnaire and spirometry. Eur Respir J. 2009; 33(5):1025–1030. PMID:
19164350.
39. Lutter JI, Jörres RA, Kahnert K, Schwarzkopf L, Studnicka M, Karrasch S, et al. Health-related quality of life associates with change in FEV
1 in COPD: results from the COSYCONET cohort. BMC Pulm Med. 2020; 20(1):148. PMID:
32471493.
40. de la Loge C, Tugaut B, Fofana F, Lambert J, Hennig M, Tschiesner U, et al. Relationship between FEV
1 and patient-reported outcomes changes: results of a meta-analysis of randomized trials in stable COPD. Chronic Obstr Pulm Dis (Miami). 2016; 3(2):519–538. PMID:
28848877.
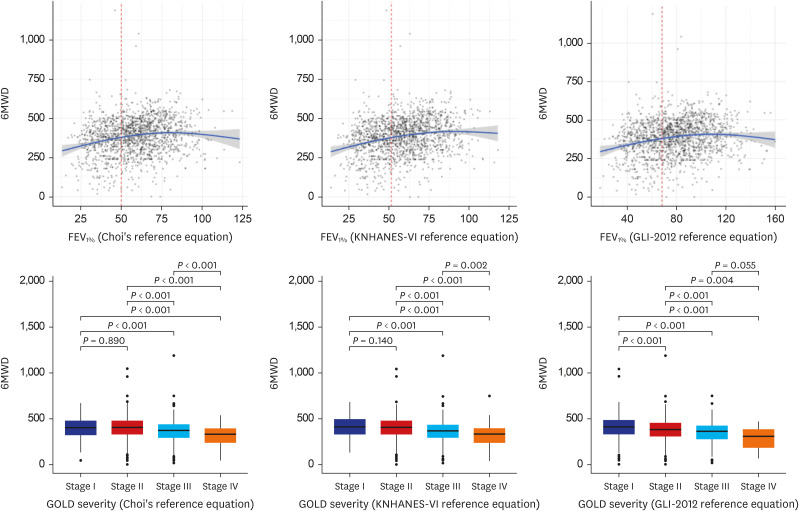
41. Agrawal MB, Awad NT. Correlation between six minute walk test and spirometry in chronic pulmonary disease. J Clin Diagn Res. 2015; 9(8):OC01–OC04.
42. Chauhan NK, Sanwaria P, Singh S, Dutt N, Saini L, Kumar S, et al. Correlation between FEV1 percentage predicted and 6 minute walk distance in patients of chronic obstructive pulmonary disease. 2017; 61(1):38–42.
43. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004; 350(10):1005–1012. PMID:
14999112.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download