1. Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017; 177(3):G1–70. PMID:
28705803.
2. Stochholm K, Juul S, Juel K, Naeraa RW, Gravholt CH. Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab. 2006; 91(10):3897–3902. PMID:
16849410.
3. Viuff MH, Stochholm K, Uldbjerg N, Nielsen BB, Gravholt CH. Danish Fetal Medicine Study Group. Only a minority of sex chromosome abnormalities are detected by a national prenatal screening program for Down syndrome. Hum Reprod. 2015; 30(10):2419–2426. PMID:
26251461.
4. Alpman A, Cogulu O, Akgul M, Arikan EA, Durmaz B, Karaca E, et al. Prenatally diagnosed Turner syndrome and cystic hygroma: incidence and reasons for referrals. Fetal Diagn Ther. 2009; 25(1):58–61. PMID:
19202339.
5. Bondy CA. Turner Syndrome Study Group. Care of girls and women with Turner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab. 2007; 92(1):10–25. PMID:
17047017.
6. Kim SE, Park SH, Han K, Cho WK, Suh BK, Park YG. Population Prevalence, Cancer Risk, and Mortality Risk of Turner Syndrome in South Korean Women Based on National Health Insurance Service Data. Yonsei Med J. 2022; 63(11):991–998. PMID:
36303307.
7. Bondy CA. Turner syndrome 2008. Horm Res. 2009; 71(Suppl 1):52–56.
8. Hjerrild BE, Mortensen KH, Gravholt CH. Turner syndrome and clinical treatment. Br Med Bull. 2008; 86(1):77–93. PMID:
18400842.
9. Balasch J. Sex steroids and bone: current perspectives. Hum Reprod Update. 2003; 9(3):207–222. PMID:
12859043.
10. Riggs BL, Khosla S, Melton LJ 3rd. Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002; 23(3):279–302. PMID:
12050121.
11. Lim SK, Lee NH, Lee JH, Choi MS, Chung YS, Ahn KJ, et al. Peak bone mass and affecting factors in Korean women. Yonsei Med J. 1993; 34(1):57–62. PMID:
8379183.
12. Lee SR, Cho MK, Cho YJ, Chun S, Hong SH, Hwang KR, et al. The 2020 menopausal hormone therapy guidelines. J Menopausal Med. 2020; 26(2):69–98. PMID:
32893509.
13. Friedman-Koss D, Crespo CJ, Bellantoni MF, Andersen RE. The relationship of race/ethnicity and social class to hormone replacement therapy: results from the Third National Health and Nutrition Examination Survey 1988-1994. Menopause. 2002; 9(4):264–272. PMID:
12082362.
14. Read MD, Edey KA, Hapeshi J, Foy C. Compliance with estrogen hormone replacement therapy after oophorectomy: a prospective study. Menopause Int. 2010; 16(2):60–64. PMID:
20729495.
15. Cameron-Pimblett A, Davies MC, Burt E, Talaulikar VS, La Rosa C, King TF, et al. Effects of estrogen therapies on outcomes in Turner syndrome: assessment of induction of puberty and adult estrogen use. J Clin Endocrinol Metab. 2019; 104(7):2820–2826. PMID:
30726925.
16. Nguyen HH, Wong P, Strauss BJ, Ebeling PR, Milat F, Vincent A. A cross-sectional and longitudinal analysis of trabecular bone score in adults with Turner syndrome. J Clin Endocrinol Metab. 2018; 103(10):3792–3800. PMID:
30020460.
17. Nakamura T, Tsuburai T, Tokinaga A, Nakajima I, Kitayama R, Imai Y, et al. Efficacy of estrogen replacement therapy (ERT) on uterine growth and acquisition of bone mass in patients with Turner syndrome. Endocr J. 2015; 62(11):965–970. PMID:
26289838.
18. Hansen MA, Overgaard K, Riis BJ, Christiansen C. Role of peak bone mass and bone loss in postmenopausal osteoporosis: 12 year study. BMJ. 1991; 303(6808):961–964. PMID:
1954420.
19. Riis BJ, Hansen MA, Jensen AM, Overgaard K, Christiansen C. Low bone mass and fast rate of bone loss at menopause: equal risk factors for future fracture: a 15-year follow-up study. Bone. 1996; 19(1):9–12. PMID:
8830981.
20. Faienza MF, Ventura A, Colucci S, Cavallo L, Grano M, Brunetti G. Bone fragility in Turner syndrome: mechanisms and prevention strategies. Front Endocrinol (Lausanne). 2016; 7:34. PMID:
27199891.
21. Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, et al. Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom. 2014; 17(2):225–242. PMID:
24690232.
22. Itonaga T, Koga E, Nishigaki S, Kawai M, Sakakibara H, Hasegawa Y. A retrospective multicenter study of bone mineral density in adolescents and adults with Turner syndrome in Japan. Endocr J. 2020; 67(10):1023–1028. PMID:
32554947.
23. Nadeem M, Roche EF. Bone mineral density in Turner’s syndrome and the influence of pubertal development. Acta Paediatr. 2014; 103(1):e38–e42. PMID:
24354573.
24. Gawlik AM, Hankus M, Szeliga K, Antosz A, Gawlik T, Soltysik K, et al. Late-onset puberty induction by transdermal estrogen in Turner syndrome girls-a longitudinal study. Front Endocrinol (Lausanne). 2018; 9:23. PMID:
29472893.
25. Holroyd CR, Davies JH, Taylor P, Jameson K, Rivett C, Cooper C, et al. Reduced cortical bone density with normal trabecular bone density in girls with Turner syndrome. Osteoporos Int. 2010; 21(12):2093–2099. PMID:
20135092.
26. Suganuma N, Furuhashi M, Hirooka T, Moriwaki T, Hasegawa Y, Mori O, et al. Bone mineral density in adult patients with Turner’s syndrome: analyses of the effectiveness of GH and ovarian steroid hormone replacement therapies. Endocr J. 2003; 50(3):263–269. PMID:
12940454.
27. Cleemann L, Hjerrild BE, Lauridsen AL, Heickendorff L, Christiansen JS, Mosekilde L, et al. Long-term hormone replacement therapy preserves bone mineral density in Turner syndrome. Eur J Endocrinol. 2009; 161(2):251–257. PMID:
19447901.
28. Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD. Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 2: trabecular bone score. J Clin Densitom. 2015; 18(3):309–330. PMID:
26277849.
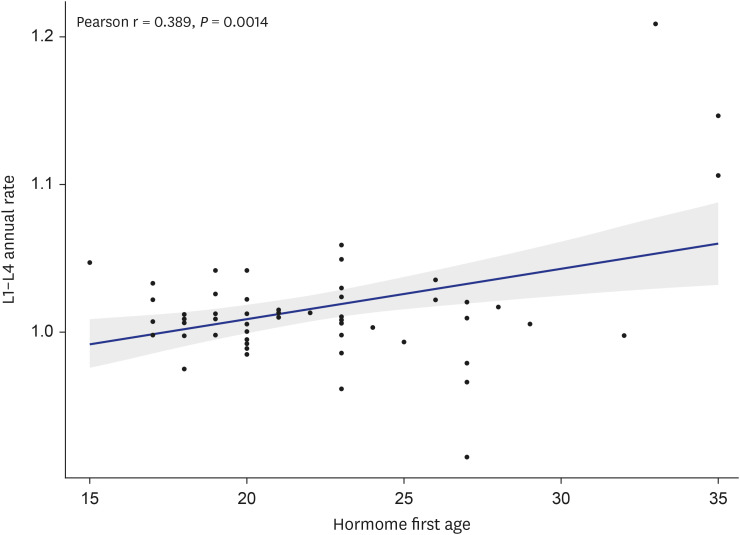
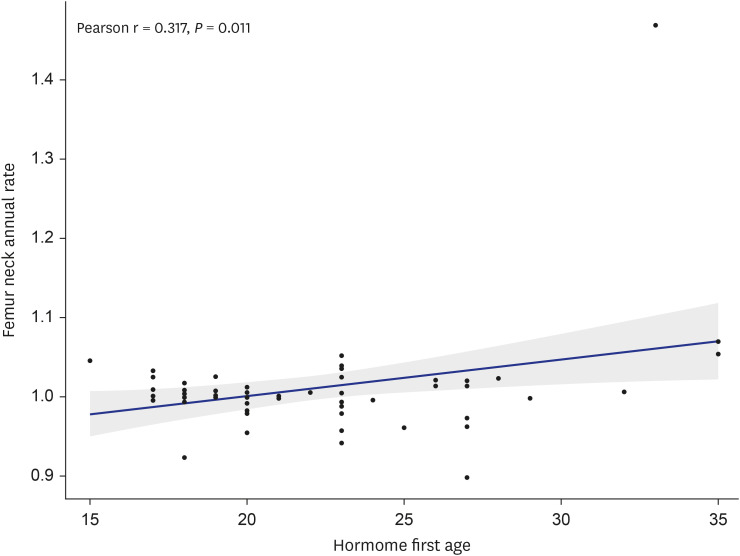
29. Nishigaki S, Itonaga T, Hasegawa Y, Kawai M. Starting age of oestrogen-progestin therapy is negatively associated with bone mineral density in young adults with Turner syndrome independent of age and body mass index. Clin Endocrinol (Oxf). 2021; 95(1):84–91. PMID:
33872421.
30. Saito S, Koga E, Okada Y, Tsuburai T, Yoshikata H, Miyagi E, et al. Effects of age at estrogen replacement therapy initiation on trabecular bone score in Japanese adults with Turner syndrome. Osteoporos Int. 2021; 32(4):671–680. PMID:
32968889.
31. Ott SM. Cortical or trabecular bone: what’s the difference? Am J Nephrol. 2018; 47(6):373–375. PMID:
29788030.
32. Lauretani F, Bandinelli S, Griswold ME, Maggio M, Semba R, Guralnik JM, et al. Longitudinal changes in BMD and bone geometry in a population-based study. J Bone Miner Res. 2008; 23(3):400–408. PMID:
17997708.
33. Khastgir G, Studd JW, Fox SW, Jones J, Alaghband-Zadeh J, Chow JW. A longitudinal study of the effect of subcutaneous estrogen replacement on bone in young women with Turner’s syndrome. J Bone Miner Res. 2003; 18(5):925–932. PMID:
12733734.
34. Sybert VP, McCauley E. Turner’s syndrome. N Engl J Med. 2004; 351(12):1227–1238. PMID:
15371580.
35. Cui X, Cui Y, Shi L, Luan J, Zhou X, Han J. A basic understanding of Turner syndrome: incidence, complications, diagnosis, and treatment. Intractable Rare Dis Res. 2018; 7(4):223–228. PMID:
30560013.
36. Högler W, Briody J, Moore B, Garnett S, Lu PW, Cowell CT. Importance of estrogen on bone health in Turner syndrome: a cross-sectional and longitudinal study using dual-energy X-ray absorptiometry. J Clin Endocrinol Metab. 2004; 89(1):193–199. PMID:
14715849.
37. McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, et al. A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res. 2016; 31(5):940–948. PMID:
26498132.
38. Naeraa RW, Brixen K, Hansen RM, Hasling C, Mosekilde L, Andresen JH, et al. Skeletal size and bone mineral content in Turner’s syndrome: relation to karyotype, estrogen treatment, physical fitness, and bone turnover. Calcif Tissue Int. 1991; 49(2):77–83. PMID:
1913298.
39. Sas TC, de Muinck Keizer-Schrama SM, Stijnen T, van Teunenbroek A, van Leeuwen WJ, Asarfi A, et al. Bone mineral density assessed by phalangeal radiographic absorptiometry before and during long-term growth hormone treatment in girls with Turner’s syndrome participating in a randomized dose-response study. Pediatr Res. 2001; 50(3):417–422. PMID:
11518831.
40. Bertelloni S, Cinquanta L, Baroncelli GI, Simi P, Rossi S, Saggese G. Volumetric bone mineral density in young women with Turner’s syndrome treated with estrogens or estrogens plus growth hormone. Horm Res. 2000; 53(2):72–76. PMID:
10971092.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download