1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington, VA, USA: American Psychiatric Publishing;2013.
2. McCurdy AP, Boulé NG, Sivak A, Davenport MH. Effects of exercise on mild-to-moderate depressive symptoms in the postpartum period: a meta-analysis. Obstet Gynecol. 2017; 129(6):1087–1097. PMID:
28486363.
3. Yun BS, Shim SH, Cho HY, Heo SJ, Jung I, Jeon HJ, et al. The impacts of insufficient sleep and its change during pregnancy on postpartum depression: a prospective cohort study of Korean women. Int J Gynaecol Obstet. 2021; 155(1):125–131. PMID:
33454978.
4. Park JH, Karmaus W, Zhang H. Prevalence of and risk factors for depressive symptoms in Korean women throughout pregnancy and in postpartum period. Asian Nurs Res. 2015; 9(3):219–225.
5. Kang SY, Khang YH, June KJ, Cho SH, Lee JY, Kim YM, et al. Prevalence and risk factors of maternal depression among women who participated in a home visitation program in South Korea. Soc Psychiatry Psychiatr Epidemiol. 2022; 57(6):1167–1178. PMID:
35044478.
6. Youn H, Lee S, Han SW, Kim LY, Lee TS, Oh MJ, et al. Obstetric risk factors for depression during the postpartum period in South Korea: a nationwide study. J Psychosom Res. 2017; 102:15–20. PMID:
28992892.
7. Choi SK, Ahn SY, Shin JC, Jang DG. A clinical study of depressive symptoms during pregnancy. Korean J Obstet Gynecol. 2009; 52(11):1102. 8.
8. Kim E, Ryu S. The relationship between depression and sociopsychological factors in pregnant women. J Korean Soc Matern Child Health. 2008; 12(2):228. 41.
9. O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013; 9(1):379–407. PMID:
23394227.
10. Cho H, Lee K, Choi E, Cho HN, Park B, Suh M, et al. Association between social support and postpartum depression. Sci Rep. 2022; 12(1):3128. PMID:
35210553.
11. Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013; 70(5):490–498. PMID:
23487258.
12. Cui C, Li M, Yang Y, Liu C, Cao P, Wang L. The effects of paternal perinatal depression on socioemotional and behavioral development of children: a meta-analysis of prospective studies. Psychiatry Res. 2020; 284:112775. PMID:
31927302.
13. Weitzman M, Rosenthal DG, Liu YH. Paternal depressive symptoms and child behavioral or emotional problems in the United States. Pediatrics. 2011; 128(6):1126–1134. PMID:
22065273.
14. Norhayati MN, Hazlina NH, Asrenee AR, Emilin WM. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. 2015; 175:34–52. PMID:
25590764.
15. Dagher RK, Shenassa ED. Prenatal health behaviors and postpartum depression: is there an association? Arch Women Ment Health. 2012; 15(1):31–37.
16. Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014; 384(9956):1775–1788. PMID:
25455248.
17. Stephens S, Ford E, Paudyal P, Smith H. Effectiveness of psychological interventions for postnatal depression in primary care: a meta-analysis. Ann Fam Med. 2016; 14(5):463–472. PMID:
27621164.
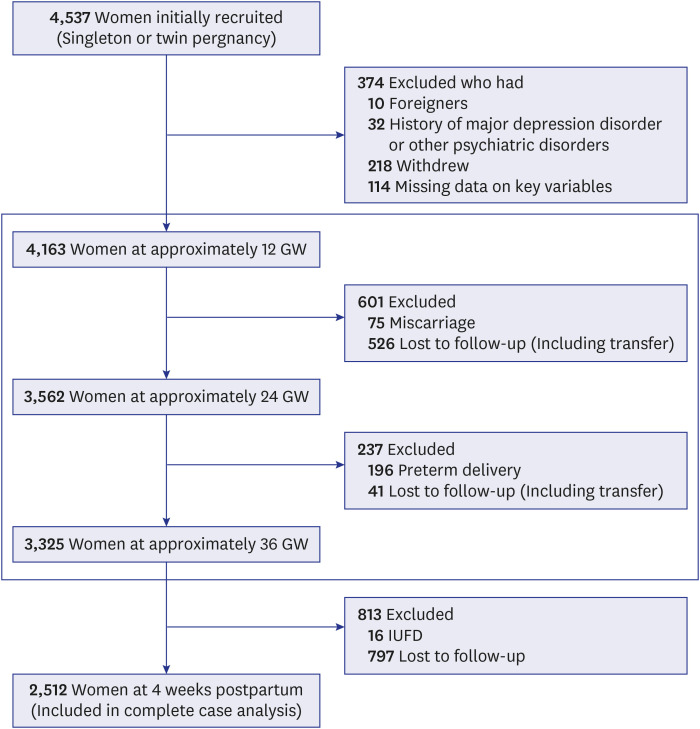
18. Choi H, Kwak DW, Kim MH, Lee SY, Chung JH, Han YJ, et al. The Korean Pregnancy Outcome Study (KPOS): study design and participants. J Epidemiol. 2021; 31(6):392–400. PMID:
32595182.
19. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987; 150(6):782–786. PMID:
3651732.
20. ACOG Committee opinion No. 757: screening for perinatal depression. Obstet Gynecol. 2018; 132(5):e208–e212. PMID:
30629567.
21. Kim YK, Hur JW, Kim KH, Oh KS, Shin YC. Clinical application of Korean version of edinburgh postnatal depression scale. J Korean Neuropsychiatr Assoc. 2008; 47:36–44.
22. Shim EJ, Shin YW, Jeon HJ, Hahm BJ. Distress and its correlates in Korean cancer patients: pilot use of the distress thermometer and the problem list. Psychooncology. 2008; 17(6):548–555. PMID:
17957764.
23. Kim MH, Cho YS, Uhm WS, Kim S, Bae SC. Cross-cultural adaptation and validation of the Korean version of the EQ-5D in patients with rheumatic diseases. Qual Life Res. 2005; 14(5):1401–1406. PMID:
16047514.
24. Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of postpartum depression on mothering. J Obstet Gynecol Neonatal Nurs. 2006; 35(5):652–658.
25. Schaffir J. Consequences of antepartum depression. Clin Obstet Gynecol. 2018; 61(3):533–543. PMID:
29659372.
26. Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry. 2000; 157(6):924–930. PMID:
10831472.
27. Okun ML. Disturbed sleep and postpartum depression. Curr Psychiatry Rep. 2016; 18(7):66. PMID:
27222140.
28. Okun ML, Hanusa BH, Hall M, Wisner KL. Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behav Sleep Med. 2009; 7(2):106–117. PMID:
19330583.
29. Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989; 262(11):1479–1484. PMID:
2769898.
30. Coll CVN, Domingues MR, Stein A, da Silva BGC, Bassani DG, Hartwig FP, et al. Efficacy of regular exercise during pregnancy on the prevention of postpartum depression: the PAMELA randomized clinical trial. JAMA Netw Open. 2019; 2(1):e186861. PMID:
30646198.
31. Nakamura A, van der Waerden J, Melchior M, Bolze C, El-Khoury F, Pryor L. Physical activity during pregnancy and postpartum depression: systematic review and meta-analysis. J Affect Disord. 2019; 246:29–41. PMID:
30576955.
32. Matsuo S, Ushida T, Iitani Y, Imai K, Nakano-Kobayashi T, Moriyama Y, et al. Pre-pregnancy sleep duration and postpartum depression: a multicenter study in Japan. Arch Women Ment Health. 2022; 25(1):181–189.
33. Wolfson AR, Crowley SJ, Anwer U, Bassett JL. Changes in sleep patterns and depressive symptoms in first-time mothers: last trimester to 1-year postpartum. Behav Sleep Med. 2003; 1(1):54–67. PMID:
15600137.
34. Wakamatsu M, Nakamura M, Douchi T, Kasugai M, Kodama S, Sano A, et al. Predicting postpartum depression by evaluating temperament during pregnancy. J Affect Disord. 2021; 292:720–724. PMID:
34161890.
35. Cheng CY, Chou YH, Chang CH, Liou SR. Trends of perinatal stress, anxiety, and depression and their prediction on postpartum depression. Int J Environ Res Public Health. 2021; 18(17):9307. PMID:
34501906.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download