1. National Lung Screening Trial Research Team. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365(5):395–409. PMID:
21714641.
2. Tukey MH, Wiener RS. Population-based estimates of transbronchial lung biopsy utilization and complications. Respir Med. 2012; 106(11):1559–1565. PMID:
22938740.
3. Detterbeck FC, Lewis SZ, Diekemper R, Addrizzo-Harris D, Alberts WM. Executive summary: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 ):Suppl. 7S–37S. PMID:
23649434.
4. Kulis M, Esteller M. DNA methylation and cancer. Adv Genet. 2010; 70:27–56. PMID:
20920744.
5. Kandimalla R, van Tilborg AA, Zwarthoff EC. DNA methylation-based biomarkers in bladder cancer. Nat Rev Urol. 2013; 10(6):327–335. PMID:
23628807.
6. Wang Y, Zhang M, Hu X, Qin W, Wu H, Wei M. Colon cancer-specific diagnostic and prognostic biomarkers based on genome-wide abnormal DNA methylation. Aging (Albany NY). 2020; 12(22):22626–22655. PMID:
33202377.
7. Darılmaz Yüce G, Ortaç Ersoy E. Lung cancer and epigenetic modifications. Tuberk Toraks. 2016; 64(2):163–170. PMID:
27481083.
8. Langevin SM, Kratzke RA, Kelsey KT. Epigenetics of lung cancer. Transl Res. 2015; 165(1):74–90. PMID:
24686037.
9. Mehta A, Dobersch S, Romero-Olmedo AJ, Barreto G. Epigenetics in lung cancer diagnosis and therapy. Cancer Metastasis Rev. 2015; 34(2):229–241. PMID:
25939322.
10. Zhang C, Yu W, Wang L, Zhao M, Guo Q, Lv S, et al. DNA methylation analysis of the SHOX2 and RASSF1A panel in bronchoalveolar lavage fluid for lung cancer diagnosis. J Cancer. 2017; 8(17):3585–3591. PMID:
29151944.
11. Dang Z, Shangguan J, Zhang C, Hu P, Ren Y, Lv Z, et al. Loss of protocadherin-17 (PCDH-17) promotes metastasis and invasion through hyperactivation of EGFR/MEK/ERK signaling pathway in hepatocellular carcinoma. Tumour Biol. 2016; 37(2):2527–2535. PMID:
26386721.
12. Chen T, Long B, Ren G, Xiang T, Li L, Wang Z, et al. Protocadherin20 acts as a tumor suppressor gene: epigenetic inactivation in nasopharyngeal carcinoma. J Cell Biochem. 2015; 116(8):1766–1775. PMID:
25736877.
13. Taylor KH, Pena-Hernandez KE, Davis JW, Arthur GL, Duff DJ, Shi H, et al. Large-scale CpG methylation analysis identifies novel candidate genes and reveals methylation hotspots in acute lymphoblastic leukemia. Cancer Res. 2007; 67(6):2617–2625. PMID:
17363581.
14. Lu Y, Lemon W, Liu PY, Yi Y, Morrison C, Yang P, et al. A gene expression signature predicts survival of patients with stage I non-small cell lung cancer. PLoS Med. 2006; 3(12):e467. PMID:
17194181.
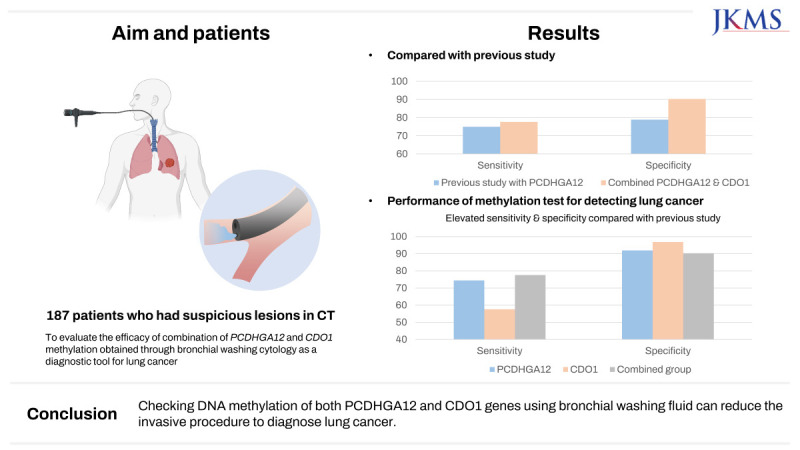
15. Jeong IB, Yoon YS, Park SY, Cha EJ, Na MJ, Kwon SJ, et al.
PCDHGA12 methylation biomarker in bronchial washing specimens as an adjunctive diagnostic tool to bronchoscopy in lung cancer. Oncol Lett. 2018; 16(1):1039–1045. PMID:
29963180.
16. Brait M, Ling S, Nagpal JK, Chang X, Park HL, Lee J, et al. Cysteine dioxygenase 1 is a tumor suppressor gene silenced by promoter methylation in multiple human cancers. PLoS One. 2012; 7(9):e44951. PMID:
23028699.
17. Harada H, Hosoda K, Moriya H, Mieno H, Ema A, Ushiku H, et al. Cancer-specific promoter DNA methylation of cysteine dioxygenase type 1 (CDO1) gene as an important prognostic biomarker of gastric cancer. PLoS One. 2019; 14(4):e0214872. PMID:
30934021.
18. Meller S, Zipfel L, Gevensleben H, Dietrich J, Ellinger J, Majores M, et al. CDO1 promoter methylation is associated with gene silencing and is a prognostic biomarker for biochemical recurrence-free survival in prostate cancer patients. Epigenetics. 2016; 11(12):871–880. PMID:
27689475.
19. Nishizawa N, Harada H, Kumamoto Y, Kaizu T, Katoh H, Tajima H, et al. Diagnostic potential of hypermethylation of the cysteine dioxygenase 1 gene (CDO1) promoter DNA in pancreatic cancer. Cancer Sci. 2019; 110(9):2846–2855. PMID:
31325200.
20. Ushiku H, Yamashita K, Ema A, Minatani N, Kikuchi M, Kojo K, et al. DNA diagnosis of peritoneal fluid cytology test by CDO1 promoter DNA hypermethylation in gastric cancer. Gastric Cancer. 2017; 20(5):784–792. PMID:
28243814.
21. Wang P, Zhao H, Shi R, Liu X, Liu J, Ren F, et al. The role of plasma CDO1 methylation in the early diagnosis of lung cancer. Zhongguo Fei Ai Za Zhi. 2020; 23(5):314–320. PMID:
32317090.
22. Chung W, Bondaruk J, Jelinek J, Lotan Y, Liang S, Czerniak B, et al. Detection of bladder cancer using novel DNA methylation biomarkers in urine sediments. Cancer Epidemiol Biomarkers Prev. 2011; 20(7):1483–1491. PMID:
21586619.
23. Kneip C, Schmidt B, Seegebarth A, Weickmann S, Fleischhacker M, Liebenberg V, et al. SHOX2 DNA methylation is a biomarker for the diagnosis of lung cancer in plasma. J Thorac Oncol. 2011; 6(10):1632–1638. PMID:
21694641.
24. Zhai X, Li SJ. Methylation of RASSF1A and CDH13 genes in individualized chemotherapy for patients with non-small cell lung cancer. Asian Pac J Cancer Prev. 2014; 15(12):4925–4928. PMID:
24998565.
26. Funahashi A, Browne TK, Houser WC, Hranicka LJ. Diagnostic value of bronchial aspirate and postbronchoscopic sputum in fiberoptic bronchoscopy. Chest. 1979; 76(5):514–517. PMID:
498821.
27. Li W, Liu JB, Hou LK, Yu F, Zhang J, Wu W, et al. Liquid biopsy in lung cancer: significance in diagnostics, prediction, and treatment monitoring. Mol Cancer. 2022; 21(1):25. PMID:
35057806.
28. Rolfo C, Mack P, Scagliotti GV, Aggarwal C, Arcila ME, Barlesi F, et al. Liquid biopsy for advanced NSCLC: a consensus statement from the International Association for the Study of Lung Cancer. J Thorac Oncol. 2021; 16(10):1647–1662. PMID:
34246791.
29. Girard P, Caliandro R, Seguin-Givelet A, Lenoir S, Gossot D, Validire P, et al. Sensitivity of cytology specimens from bronchial aspirate or washing during bronchoscopy in the diagnosis of lung malignancies: an update. Clin Lung Cancer. 2017; 18(5):512–518. PMID:
28007409.
30. Villalba M, Exposito F, Pajares MJ, Sainz C, Redrado M, Remirez A, et al. TMPRSS4: a novel tumor prognostic indicator for the stratification of stage IA tumors and a liquid biopsy biomarker for NSCLC patients. J Clin Med. 2019; 8(12):2134. PMID:
31817025.
31. Topaloglu O, Hoque MO, Tokumaru Y, Lee J, Ratovitski E, Sidransky D, et al. Detection of promoter hypermethylation of multiple genes in the tumor and bronchoalveolar lavage of patients with lung cancer. Clin Cancer Res. 2004; 10(7):2284–2288. PMID:
15073103.
32. Schnabel RM, van der Velden K, Osinski A, Rohde G, Roekaerts PM, Bergmans DC. Clinical course and complications following diagnostic bronchoalveolar lavage in critically ill mechanically ventilated patients. BMC Pulm Med. 2015; 15(1):107. PMID:
26420333.
33. Zhang H, Wang S, Zhong F, Liao M. Risk factors for air embolism following computed tomography-guided percutaneous transthoracic needle biopsy: a systematic review and meta-analysis. Diagn Interv Radiol. 2023; 29(3):478–491. PMID:
36994842.
34. Polat G, Özdemir Ö, Serçe Unat D, Karadeniz G, Ayrancı A, Unat OS, et al. Pneumothoraxes after CT-guided percutaneous transthoracic needle aspiration biopsy of the lung: a single-center experience with 3426 patients. Tuberk Toraks. 2023; 71(1):67–74. PMID:
36912411.
35. Na KJ, Park IK, Park S, Kang CH, Kim YT. Efficacy and cost-effectiveness of surgical biopsy for histologic diagnosis of indeterminate nodules suspected for early stage lung cancer: comparison with percutaneous needle biopsy. J Korean Med Sci. 2020; 35(28):e261. PMID:
32686374.
36. Ji XY, Li H, Chen HH, Lin J. Diagnostic performance of RASSF1A and SHOX2 methylation combined with EGFR mutations for differentiation between small pulmonary nodules. J Cancer Res Clin Oncol. 2023; 149(11):8557–8571. PMID:
37097393.
37. Hulbert A, Jusue-Torres I, Stark A, Chen C, Rodgers K, Lee B, et al. Early detection of lung cancer using DNA promoter hypermethylation in plasma and sputum. Clin Cancer Res. 2017; 23(8):1998–2005. PMID:
27729459.
38. Marmor HN, Zorn JT, Deppen SA, Massion PP, Grogan EL. Biomarkers in lung cancer screening: a narrative review. Curr Chall Thorac Surg. 2023; 5:5. PMID:
37016707.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download