1. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22(7):707–710. PMID:
8844239.
2. Moreno R, Rhodes A, Piquilloud L, Hernandez G, Takala J, Gershengorn HB, et al. The Sequential Organ Failure Assessment (SOFA) Score: has the time come for an update? Crit Care. 2023; 27(1):15. PMID:
36639780.
3. Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019; 23(1):374. PMID:
31775846.
4. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26(11):1793–1800. PMID:
9824069.
5. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286(14):1754–1758. PMID:
11594901.
6. Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009; 37(5):1649–1654. PMID:
19325482.
7. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of Clinical Criteria for Sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315(8):762–774. PMID:
26903335.
8. Karakike E, Kyriazopoulou E, Tsangaris I, Routsi C, Vincent JL, Giamarellos-Bourboulis EJ. The early change of SOFA score as a prognostic marker of 28-day sepsis mortality: analysis through a derivation and a validation cohort. Crit Care. 2019; 23(1):387. PMID:
31783881.
9. Pölkki A, Pekkarinen PT, Takala J, Selander T, Reinikainen M. Association of Sequential Organ Failure Assessment (SOFA) components with mortality. Acta Anaesthesiol Scand. 2022; 66(6):731–741. PMID:
35353902.
10. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315(8):801–810. PMID:
26903338.
11. Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315(8):775–787. PMID:
26903336.
12. Bachmann KF, Arabi YM, Regli A, Starkopf J, Reintam Blaser A. Cardiovascular SOFA score may not reflect current practice. Intensive Care Med. 2022; 48(1):119–120. PMID:
34596703.
13. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021; 47(11):1181–1247. PMID:
34599691.
14. Kovach CP, Fletcher GS, Rudd KE, Grant RM, Carlbom DJ. Comparative prognostic accuracy of sepsis scores for hospital mortality in adults with suspected infection in non-ICU and ICU at an academic public hospital. PLoS One. 2019; 14(9):e0222563. PMID:
31525224.
15. Gupta T, Puskarich MA, DeVos E, Javed A, Smotherman C, Sterling SA, et al. Sequential Organ Failure Assessment component score prediction of in-hospital mortality from sepsis. J Intensive Care Med. 2020; 35(8):810–817. PMID:
30165769.
16. Jee W, Jo S, Lee JB, Jin Y, Jeong T, Yoon JC, et al. Mortality difference between early-identified sepsis and late-identified sepsis. Clin Exp Emerg Med. 2020; 7(3):150–160. PMID:
33028057.
17. Kim DS, Park JE, Hwang SY, Jeong D, Lee GT, Kim T, et al. Prediction of vasopressor requirement among hypotensive patients with suspected infection: usefulness of diastolic shock index and lactate. Clin Exp Emerg Med. 2022; 9(3):176–186. PMID:
36164800.
18. Houwink AP, Rijkenberg S, Bosman RJ, van der Voort PH. The association between lactate, mean arterial pressure, central venous oxygen saturation and peripheral temperature and mortality in severe sepsis: a retrospective cohort analysis. Crit Care. 2016; 20(1):56. PMID:
26968689.
19. Vincent JL, Quintairos E Silva A, Couto L Jr, Taccone FS. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care. 2016; 20(1):257. PMID:
27520452.
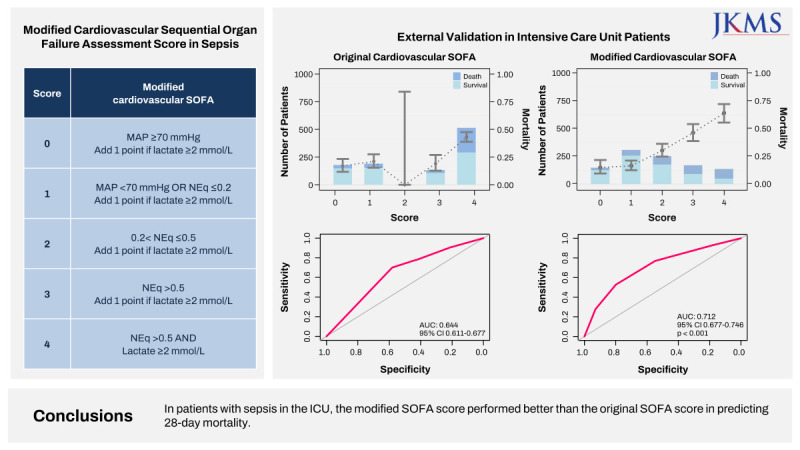
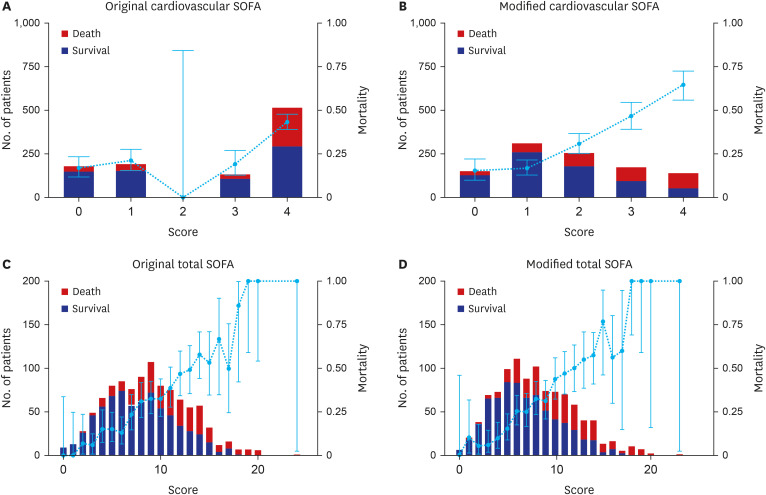
20. Lee HJ, Ko BS, Ryoo SM, Han E, Suh GJ, Choi SH, et al. Modified cardiovascular SOFA score in sepsis: development and internal and external validation. BMC Med. 2022; 20(1):263. PMID:
35989336.
21. Namgung M, Ahn C, Park Y, Kwak IY, Lee J, Won M. Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis. Clin Exp Emerg Med. 2023; 10(2):157–171. PMID:
36882054.
22. de Grooth HJ, Elbers PW, Vincent JL. Vitamin C for sepsis and acute respiratory failure. JAMA. 2020; 323(8):792.
23. Ho KM, Lee KY, Williams T, Finn J, Knuiman M, Webb SA. Comparison of Acute Physiology and Chronic Health Evaluation (APACHE) II score with organ failure scores to predict hospital mortality. Anaesthesia. 2007; 62(5):466–473. PMID:
17448058.
24. Minne L, Abu-Hanna A, de Jonge E. Evaluation of SOFA-based models for predicting mortality in the ICU: a systematic review. Crit Care. 2008; 12(6):R161. PMID:
19091120.
25. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017; 317(3):290–300. PMID:
28114553.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download