This article has been
cited by other articles in ScienceCentral.
Abstract
The Guidelines of the 2019 European Society of Cardiology (ESC) and the 5th Society of Lipid and Atherosclerosis (KSoLA) for the Management of Dyslipidemia advocate a more intensive lipid-lowering strategy. However, there is a lack of evidence regarding the current status of lipid management in Korean patients in real-world practice. The Korean Society of Myocardial Infarction conducted a survey among its members of the Korean Society of Cardiology on the new lipid guidelines. Although most participants were aware of the changes in the ESC and the KSoLA guidelines, more than half of them did not agree with lowering the low-density lipoprotein cholesterol levels to < 55 mg/dL, because its safety and efficacy have not yet been proven in Koreans. A substantial disparity exists between lipid management guidelines and current clinical practices, highlighting the necessity for clinical research that specifically targets East Asians and Koreans to bridge this gap.
Keywords: Dyslipidemias, Myocardial Infarction, Cholesterol, Low-density Lipoprotein Cholesterol
The upcoming 5th Korean Guidelines for the Management of Dyslipidemia of the Korean Society of Lipid and Atherosclerosis is expected to advocate several changes from previous guidelines. This guideline endorses a treat-to-target strategy, which is an approach shared by the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) guidelines
1 but differs in each risk category. The ESC and new Korean guidelines recommend a low-density lipoprotein cholesterol (LDL-C) reduction of ≥ 50% from baseline and an LDL-C goal of < 55 mg/dL in secondary prevention for patients with coronary artery disease (CAD). It optionally recommends the same target LDL-C reduction and goal in patients with diabetes mellitus for ≥ 10 years with target organ damage or three or more major risk factors. The 4th edition of the Korean Guidelines for the Management of Dyslipidemia recommended lowering LDL-C to < 70 mg/dL for patients at very high risk (CAD, atherosclerotic ischemic stroke, transient ischemic attack, and peripheral artery disease).
2 However, there is still a lack of evidence concerning the current status of lipid management in Korean patients in real-world practice. From this perspective, we summarized a survey of the Korean Society of Myocardial Infarction (KSMI) on lipid management in patients with CAD, including acute myocardial infarction (AMI), and revealed the gap between guidelines and real-world practice.
To shed light on the impact of the new Korean lipid guidelines on the management of patients with dyslipidemia encountered in routine clinical practice, KSMI conducted a survey among its members of the Korean Society of Cardiology (KSC). A link to a web-based survey containing 15 questions was mailed to KSC members between July 1 and July 15, 2022. The survey consisted of 15 questions regarding the participants’ general personal information and lipid-lowering therapy (
Supplementary Data 1).
A total of 407 members responded to the survey. Of them, 79.9% were male and 46.9% were doctors in their 40s. Among them, 60.7% were interventional cardiologists and 63.6% work in teaching hospitals and 54.0% worked in Seoul or Capital area of Korea.
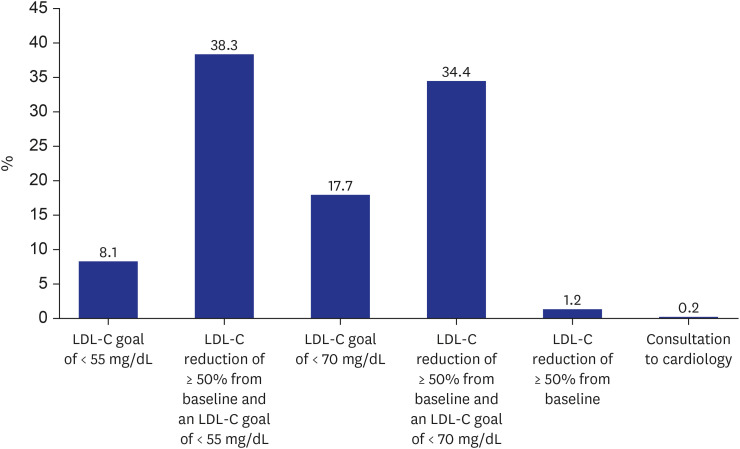
Of all the survey participants, 94.1% were aware of the changes in the Korean lipid guidelines. With respect to the target for LDL-C reduction in patients with AMI, 46.4% of the respondents opted for an LDL-C goal of < 55 mg/dL, while 52.1% selected a goal of < 70 mg/dL (
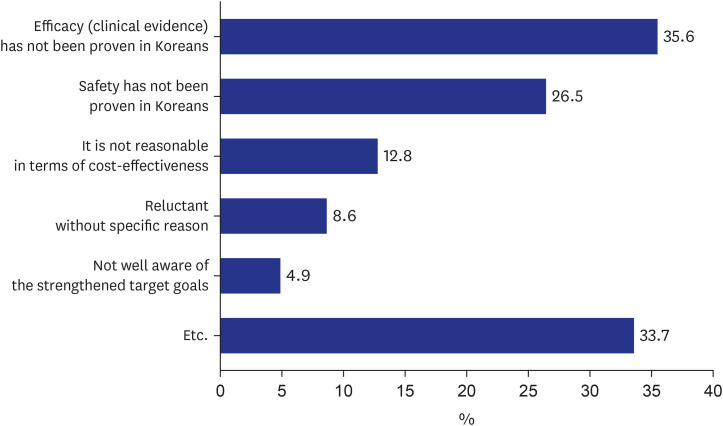
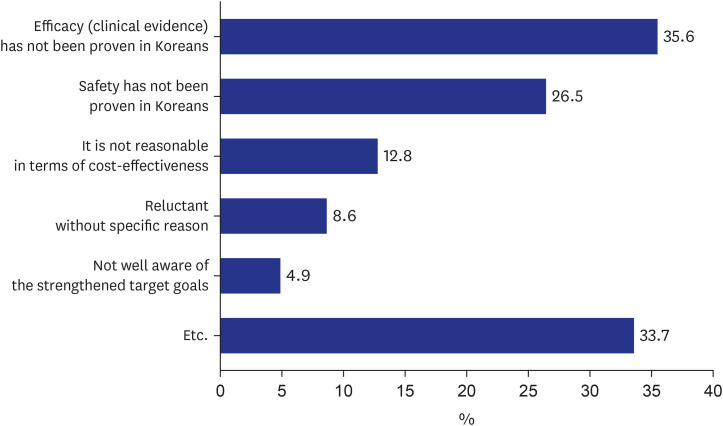
Fig. 1). The primary rationale for excluding the new LDL-C goal was inadequate substantiated data with respect to its efficacy (35.6%) and safety (26.5%) in the Korean population (
Fig. 2). Cost-effectiveness (12.8%) constituted the third rationale. Regarding the goal of reducing LDL-C levels in individuals with atherosclerotic cardiovascular disease (excluding AMI), only 12.6% of the participants selected an LDL-C target of < 55 mg/dL. With respect to lipid-lowering strategy in patients with AMI, 65.1% of the respondents used high-intensity statins regardless of the LDL-C level. The main reason for not following the new LDL-C goal was the lack of evidence regarding its efficacy and safety in the Korean population. When the initial drug treatment failed to achieve the LDL-C goal, 62.7% of the participants answered that they added ezetimibe first, while 34.6% increased statin dose to the maximum. Regarding the reason for the early use of ezetimibe instead of statin intensification, participants chose the following as the main reasons: concerns regarding the side effects of high-dose statins (16.0%) and improved chances of attaining LDL-C goal when ezetimibe was added (16.2%). Approximately half of the participants (47.4%) answered that the time of their first blood test in patients with AMI was 4–6 weeks after discharge. Approximately 63.4% of the survey respondents indicated that they would consider prescribing proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors to patients with AMI only if their LDL-C levels were < 70 mg/dL, and only 11.1% considered prescribing this lipid-lowering agent to patients with LDL-C levels < 55 mg/dL.
The main findings of the KSMI survey are summarized as follows: Most survey participants were in their 40s, male, and primarily university hospital workers who performed cardiovascular interventions. The survey appears to have recruited a group of cardiologists who treat the greatest number of patients with AMI and stable CAD in clinical practice, and the survey results can serve as a basis for representativeness. Although most survey participants were aware of the changes in the clinical guidelines, they had different perceptions of lower LDL-C targets for AMI and stable CAD. Despite the participants’ belief that stricter criteria are needed for LDL-C targets in patients with AMI, more than half did not agree with lowering LDL-C levels to < 55 mg/dL, primarily because its safety and efficacy have not been proven in Koreans. Participants preferred high-intensity statins as the initial treatment strategy for patients with AMI, regardless of LDL-C levels. If the target dose was not reached within 4–6 weeks, they preferred to add ezetimibe rather than increasing the statin dose to the maximum. This result differs from current clinical guidelines that recommend adding ezetimibe after increasing the statin dose to the maximum. The reasons for early selection of ezetimibe were concerns regarding both safety of statins and their efficacy in achieving LDL-C targets. This shows that in actual clinical practice, although high-intensity statins increase adverse reactions, there still is concern that they cannot attain the strengthened LDL-C targets with the maximum dose, despite current clinical guidelines recommending the addition of ezetimibe after maximum dose high-intensity statins. For patients with AMI, the LDL-C level for considering PCSK-9 inhibitor use was thought to be 70 mg/dL, rather than the LDL-C target of 55 mg/dL. This may be interpreted as a conservative treatment preference owing to the reluctance to use injectable drugs; however, it is estimated that the LDL-C target is actually set at 70 mg/dL.
Based on the results of the IMPROVE-IT, FOURRIER, and ODYSSEY OUTCOMES studies, the 2018 American College of Cardiology (ACC)/American Heart Association (AHA)
3 and 2019 ESC/EAS guidelines
1 were published, endorsing the use of intensive lipid-lowering therapy for high-risk cardiovascular patients based on robust evidence. However, it is important to note that applying these findings directly to Korean patients may pose challenges due to the limited inclusion of Asian populations in these studies.
456 Moreover, the impact and potential side effects of intensive lipid-lowering therapy remain uncertain, and there is a possibility of overestimating the risk of cardiovascular disease in Korea.
Society offers valuable clinical practice guidelines based on scientific evidence. The KSMI survey findings confirmed that many doctors do not adhere to these guidelines. This noncompliance can be attributed, in part, to insufficient evidence regarding the safety and efficacy of these guidelines in Koreans. Although the use of PCSK9 inhibitor is inevitable to reach the LDL-C 55 mg/dL target, there is a tendency to give up on reaching the target due to limited insurance benefit indications in Korea. A substantial disparity exists between lipid management guidelines and current clinical practices, highlighting the necessity for clinical research specifically targeting East Asians and Koreans to bridge this gap. Society should adopt a humble approach, provide comprehensive explanations, and effectively communicate scientific evidence and expert opinions to practicing doctors.
This study has some limitations. These findings are relevant only for the duration of the investigation. Representation may be lacking because not all cardiologists in KSC responded to the survey.
In conclusion, the survey revealed a significant gap between lipid management guidelines and real-world clinical practice and suggests that clinical research focusing on East Asians and Koreans is essential to redress the gap.
Fig. 1
What is your LDL-C goal in patients with acute myocardial infarction?
LDL-C = low-density lipoprotein cholesterol.
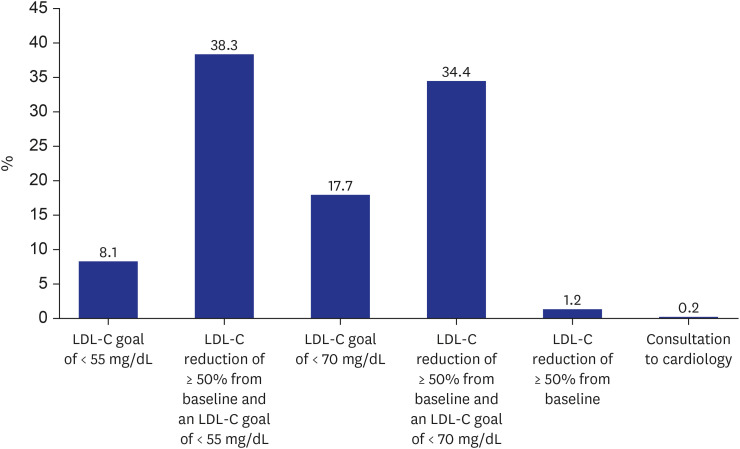
Fig. 2
Why are you not following the new goal of low-density lipoprotein cholesterol < 55 mg/dL?




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download