METHODS
Study setting
This study was conducted at a single university hospital emergency medical center located in a large city in South Korea, using medical records from January 1, 2019, to December 31, 2021. The ED had approximately 90,000 annual visits before the COVID-19 pandemic and approximately 60,000 annual visits after the pandemic. Patients with AMI can be diagnosed and treated with emergency procedures such as coronary angiography (CAG), percutaneous coronary intervention (PCI), and coronary artery bypass graft.
South Korea’s government-based emergency medical system is run by the National Fire Agency. Prehospital emergency medical services (EMS) providers must have first- or second-class emergency medical technician (EMT) or nurse qualifications. Currently, the Emergency Medical Care Act and the Medical Service Act do not allow EMS providers to perform a 12-lead ECG in the field. Therefore, all patients with chest pain can have a 12-lead ECG performed after arrival at the ED. AHA guidelines recommend a 12-lead ECG within 10 minutes for patients presenting to the ED with chest pain as their chief complaint.
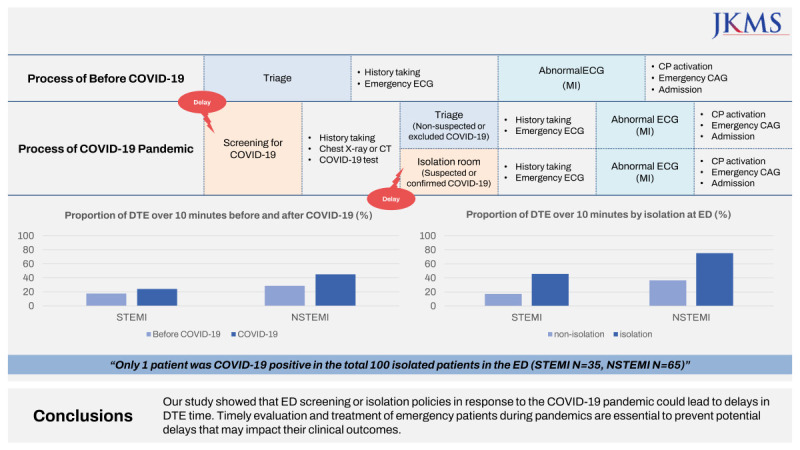
Since the COVID-19 pandemic, all EDs in South Korea have started screening for symptoms of suspected COVID-19. When a patient presents to the ED where the study was conducted, they are first screened for COVID-19. Patients with symptoms of dyspnea, fever of 37.5°C or higher, cough, rhinorrhea, sputum, or who have had close contact with someone who is positive for COVID-19 will undergo chest X-ray or chest computed tomography (CT) scan regardless of their primary symptoms. Finally, the decision to isolate is made by an emergency physician.
If a patient presents to the ED with chest pain, chest discomfort, dyspnea, epigastric pain, or syncope, the triage nurse can order an emergency 12-lead ECG before the patient is formally seen by a physician. An ECG is performed by a doctor (intern) with the assistance of an EMT. Emergency ECG protocols in the ED were the same in the pre-pandemic and pandemic periods. The triage nurse must be certified in the Korean Triage and Acuity Scale (KTAS), which evaluates the patient's main symptoms into five levels of emergency.
10 If STEMI is suspected on the emergency ECG, the on-call cardiologist is immediately called to determine whether emergency CAG and PCI should be performed.
Study design
This was a retrospective cross-sectional study.
Study population
The study population includes patients of all ages who visited the ED between January 1, 2019, and December 31, 2021, underwent CAG, and were finally diagnosed with STEMI or NSTEMI by cardiologists. Patients were categorized into two groups: the STEMI group and the NSTEMI group. Patients admitted to the cardiology department with a final diagnosis of acute coronary disease other than STEMI or NSTEMI were excluded.
Main outcomes
The primary outcome variables for this study were DTE and in-hospital mortality. DTE was defined as the time from the patient’s arrival and admission to the ED to the electronic transmission of the 12-lead ECG results, both of which are accurately recorded in the electronic medical record. When acquiring a 12-lead ECG, the ECG machine automatically enters the acquisition time into the ECG results, which is used as reference. In-hospital mortality was defined as death in the ED or in the general ward or intensive care unit as documented by the medical record.
Main exposures
The primary exposure in this study is the COVID-19 pandemic. After the first case of COVID-19 in South Korea in January 2020, the participating ED began screening for COVID-19 on January 28. The first wave of the pandemic began in February with a large outbreak of COVID-19 cases in Daegu.
11 For simplicity, the comparison periods are January 1, 2019, to December 31, 2019, before the pandemic, and January 1, 2020, to December 31, 2021. The second exposure is ED isolation status. ED isolation was defined as admission to a negative pressure isolation room of the ED. Patients whose chest radiograph or chest CT scan excludes the possibility of COVID-19 pneumonia were determined not to require isolation. Otherwise, patients were defined as not isolated if they were initially admitted to the non-isolated area of the ED or to the cardiopulmonary resuscitation unit.
Confounders
Baseline patient characteristics, such as gender, age, and medical history, were collected from medical records. Means of transportation were classified as either 119 EMS ambulance or other transportation modes, including private cars. In STEMI cases, the main symptoms reported by patients were categorized into five groups: chest pain, chest discomfort, dyspnea, epigastric pain, and other symptoms, whereas in NSTEMI cases, seven groups were used, with the addition of fever and respiratory symptoms based on the initial nursing records documented by KTAS-certified triage nurses. The KTAS levels assigned by the triage nurses were also examined. Dyspnea was considered a symptom if it was recorded in the initial nursing record, and fever was defined as an initial vital sign of 37.5°C or higher based on the criteria established by the Korea Disease Control and Prevention Agency.
Statistical analysis
The χ2 test was used for categorical variables, and the t-test was used for continuous variables. The Wilcoxon rank-sum test was employed for continuous variables that were not normally distributed. A P value of less than 0.05 was considered statistically significant. Multivariate logistic regression was performed to assess the relationship between independent and outcome variables, with covariates including gender, age group, means of ED visit, and KTAS levels. Stata 16.1 (StataCorp LLC, College Station, TX, USA) was used for statistical analysis.
Ethics statement
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (approval No. B-2106-690-107), and informed consent was waived.
RESULTS
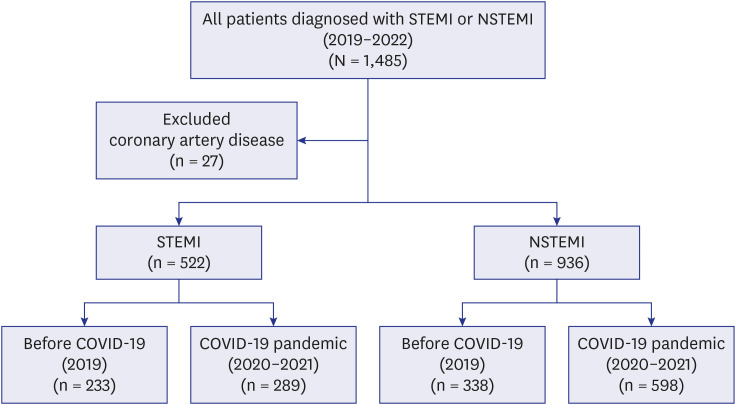
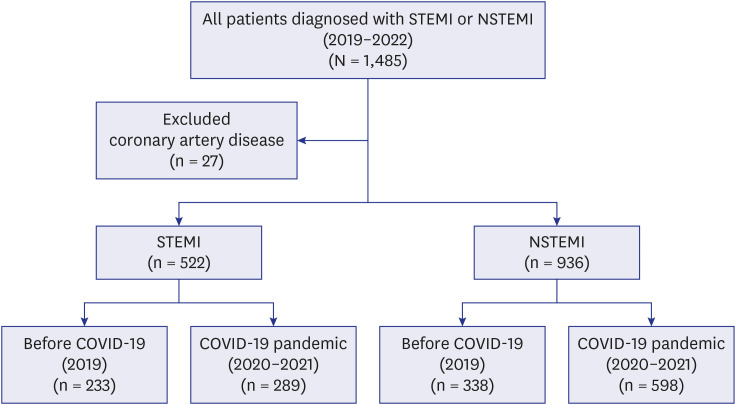
During the study period, 1,485 patients underwent CAG and were diagnosed with STEMI or NSTEMI by cardiologists, with 27 excluded due to a final diagnosis of acute coronary disease rather than MI. Of the remaining patients, 522 were STEMI cases, with 233 occurring before the pandemic and 289 during the pandemic. For NSTEMI, there were 936 cases, with 338 before the pandemic and 598 during the pandemic (
Fig. 1).
Fig. 1
Flow chart of subjected patients.
STEMI = ST segment elevation myocardial infarction, NSTEMI = non-ST segment elevation myocardial infarction, COVID-19 = coronavirus disease 2019.
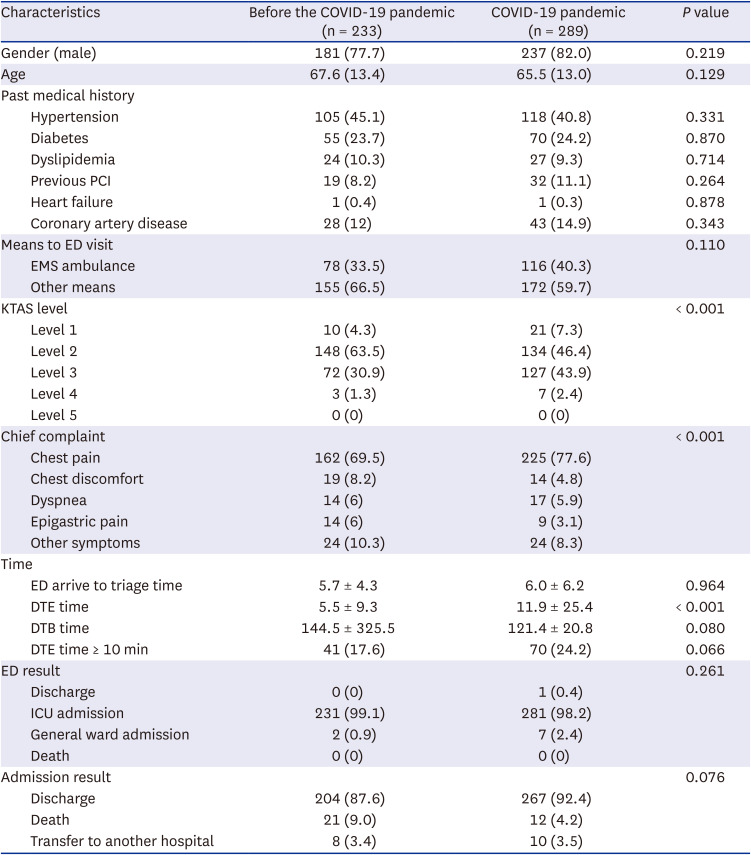
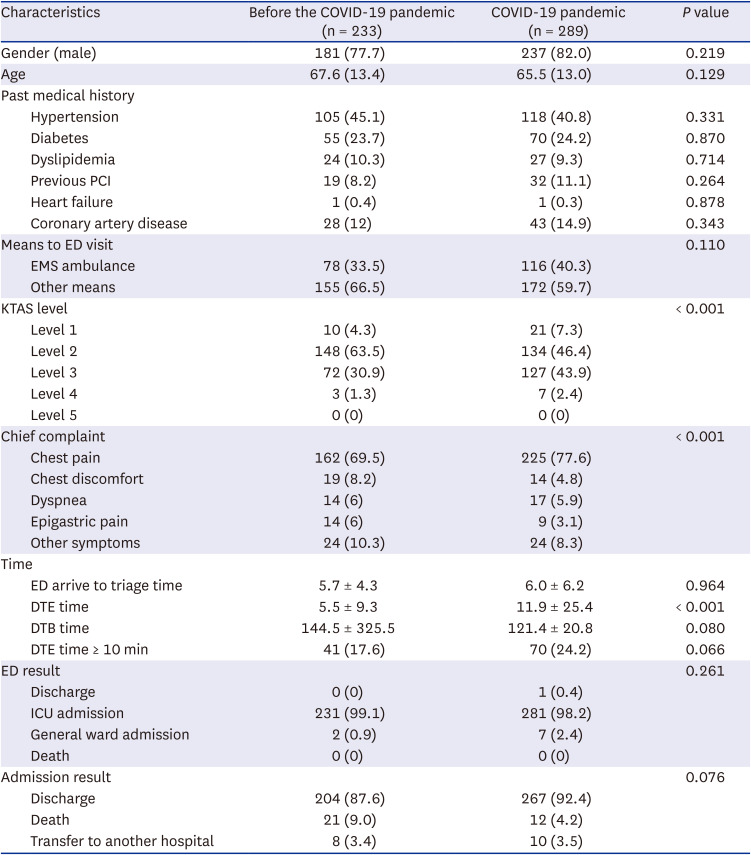
Male patients comprised most STEMI cases, with a mean age of 67.6 years, and about one-third arrived at the ED by EMS ambulance. The most common KTAS level was 2, and chest pain was the most frequently reported chief complaint. During the pandemic period, there was a higher proportion of patients with KTAS level 1 and a lower proportion of levels 2 and 3, as well as a higher proportion of patients with chest pain as their primary symptom. The mean duration of DTE time for STEMI patients during the pandemic period was 11.9 minutes, while the mean duration of DTE time during the pre-pandemic period was 5.5 minutes. Although there was a higher proportion of patients with a DTE time greater than 10 minutes during the pandemic period, the difference was not statistically significant. ED and post-hospitalization outcomes were not significantly different between the two groups (
Table 1).
Table 1
Comparison of ST segment elevation myocardial infarction patient baseline characteristics and clinical outcomes in pre-pandemic and pandemic periods
|
Characteristics |
Before the COVID-19 pandemic (n = 233) |
COVID-19 pandemic (n = 289) |
P value |
|
Gender (male) |
181 (77.7) |
237 (82.0) |
0.219 |
|
Age |
67.6 (13.4) |
65.5 (13.0) |
0.129 |
|
Past medical history |
|
|
|
|
Hypertension |
105 (45.1) |
118 (40.8) |
0.331 |
|
Diabetes |
55 (23.7) |
70 (24.2) |
0.870 |
|
Dyslipidemia |
24 (10.3) |
27 (9.3) |
0.714 |
|
Previous PCI |
19 (8.2) |
32 (11.1) |
0.264 |
|
Heart failure |
1 (0.4) |
1 (0.3) |
0.878 |
|
Coronary artery disease |
28 (12) |
43 (14.9) |
0.343 |
|
Means to ED visit |
|
|
0.110 |
|
EMS ambulance |
78 (33.5) |
116 (40.3) |
|
Other means |
155 (66.5) |
172 (59.7) |
|
KTAS level |
|
|
< 0.001 |
|
Level 1 |
10 (4.3) |
21 (7.3) |
|
Level 2 |
148 (63.5) |
134 (46.4) |
|
Level 3 |
72 (30.9) |
127 (43.9) |
|
Level 4 |
3 (1.3) |
7 (2.4) |
|
Level 5 |
0 (0) |
0 (0) |
|
Chief complaint |
|
|
< 0.001 |
|
Chest pain |
162 (69.5) |
225 (77.6) |
|
Chest discomfort |
19 (8.2) |
14 (4.8) |
|
Dyspnea |
14 (6) |
17 (5.9) |
|
Epigastric pain |
14 (6) |
9 (3.1) |
|
Other symptoms |
24 (10.3) |
24 (8.3) |
|
Time |
|
|
|
|
ED arrive to triage time |
5.7 ± 4.3 |
6.0 ± 6.2 |
0.964 |
|
DTE time |
5.5 ± 9.3 |
11.9 ± 25.4 |
< 0.001 |
|
DTB time |
144.5 ± 325.5 |
121.4 ± 20.8 |
0.080 |
|
DTE time ≥ 10 min |
41 (17.6) |
70 (24.2) |
0.066 |
|
ED result |
|
|
0.261 |
|
Discharge |
0 (0) |
1 (0.4) |
|
ICU admission |
231 (99.1) |
281 (98.2) |
|
General ward admission |
2 (0.9) |
7 (2.4) |
|
Death |
0 (0) |
0 (0) |
|
Admission result |
|
|
0.076 |
|
Discharge |
204 (87.6) |
267 (92.4) |
|
Death |
21 (9.0) |
12 (4.2) |
|
Transfer to another hospital |
8 (3.4) |
10 (3.5) |
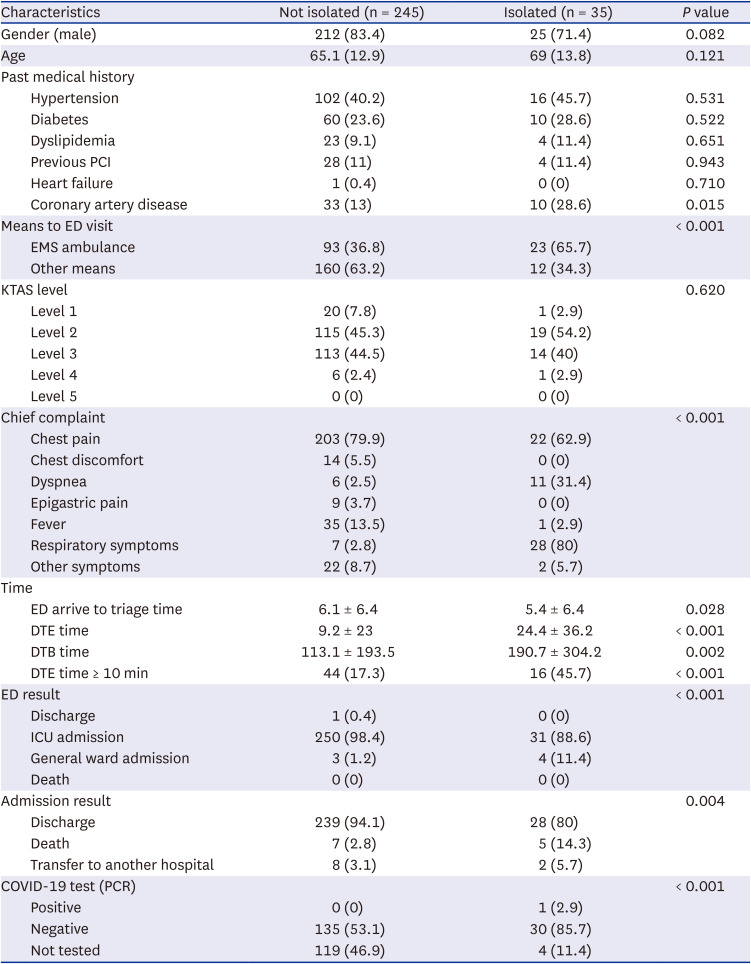
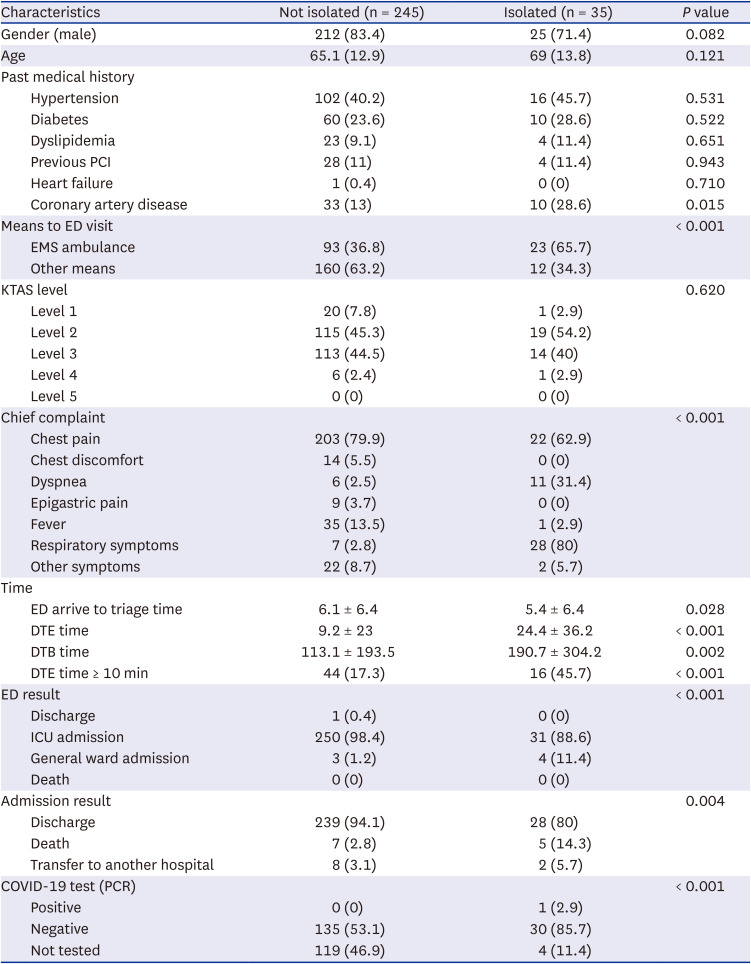
In both isolated and non-isolated STEMI groups, males were the predominant gender, and the average age was in the mid-to-late 60s. The isolated group had a higher likelihood of presenting to the ED by EMS ambulance and reporting dyspnea as their main symptom, while fever was a rare reason for isolation. The isolation group had a longer mean DTE time, and a significantly higher proportion of DTEs greater than 10 minutes compared to the non-isolated group. Additionally, the isolation group had a significantly higher proportion of in-hospital deaths. Throughout the study period, only one STEMI patient was diagnosed with COVID-19 (
Table 2).
Table 2
Comparison of ST segment elevation myocardial infarction patient baseline characteristics and clinical outcomes by isolation status
|
Characteristics |
Not isolated (n = 245) |
Isolated (n = 35) |
P value |
|
Gender (male) |
212 (83.4) |
25 (71.4) |
0.082 |
|
Age |
65.1 (12.9) |
69 (13.8) |
0.121 |
|
Past medical history |
|
|
|
|
Hypertension |
102 (40.2) |
16 (45.7) |
0.531 |
|
Diabetes |
60 (23.6) |
10 (28.6) |
0.522 |
|
Dyslipidemia |
23 (9.1) |
4 (11.4) |
0.651 |
|
Previous PCI |
28 (11) |
4 (11.4) |
0.943 |
|
Heart failure |
1 (0.4) |
0 (0) |
0.710 |
|
Coronary artery disease |
33 (13) |
10 (28.6) |
0.015 |
|
Means to ED visit |
|
|
< 0.001 |
|
EMS ambulance |
93 (36.8) |
23 (65.7) |
|
Other means |
160 (63.2) |
12 (34.3) |
|
KTAS level |
|
|
0.620 |
|
Level 1 |
20 (7.8) |
1 (2.9) |
|
Level 2 |
115 (45.3) |
19 (54.2) |
|
Level 3 |
113 (44.5) |
14 (40) |
|
Level 4 |
6 (2.4) |
1 (2.9) |
|
Level 5 |
0 (0) |
0 (0) |
|
Chief complaint |
|
|
< 0.001 |
|
Chest pain |
203 (79.9) |
22 (62.9) |
|
Chest discomfort |
14 (5.5) |
0 (0) |
|
Dyspnea |
6 (2.5) |
11 (31.4) |
|
Epigastric pain |
9 (3.7) |
0 (0) |
|
Fever |
35 (13.5) |
1 (2.9) |
|
Respiratory symptoms |
7 (2.8) |
28 (80) |
|
Other symptoms |
22 (8.7) |
2 (5.7) |
|
Time |
|
|
|
|
ED arrive to triage time |
6.1 ± 6.4 |
5.4 ± 6.4 |
0.028 |
|
DTE time |
9.2 ± 23 |
24.4 ± 36.2 |
< 0.001 |
|
DTB time |
113.1 ± 193.5 |
190.7 ± 304.2 |
0.002 |
|
DTE time ≥ 10 min |
44 (17.3) |
16 (45.7) |
< 0.001 |
|
ED result |
|
|
< 0.001 |
|
Discharge |
1 (0.4) |
0 (0) |
|
ICU admission |
250 (98.4) |
31 (88.6) |
|
General ward admission |
3 (1.2) |
4 (11.4) |
|
Death |
0 (0) |
0 (0) |
|
Admission result |
|
|
0.004 |
|
Discharge |
239 (94.1) |
28 (80) |
|
Death |
7 (2.8) |
5 (14.3) |
|
Transfer to another hospital |
8 (3.1) |
2 (5.7) |
|
COVID-19 test (PCR) |
|
|
< 0.001 |
|
Positive |
0 (0) |
1 (2.9) |
|
Negative |
135 (53.1) |
30 (85.7) |
|
Not tested |
119 (46.9) |
4 (11.4) |
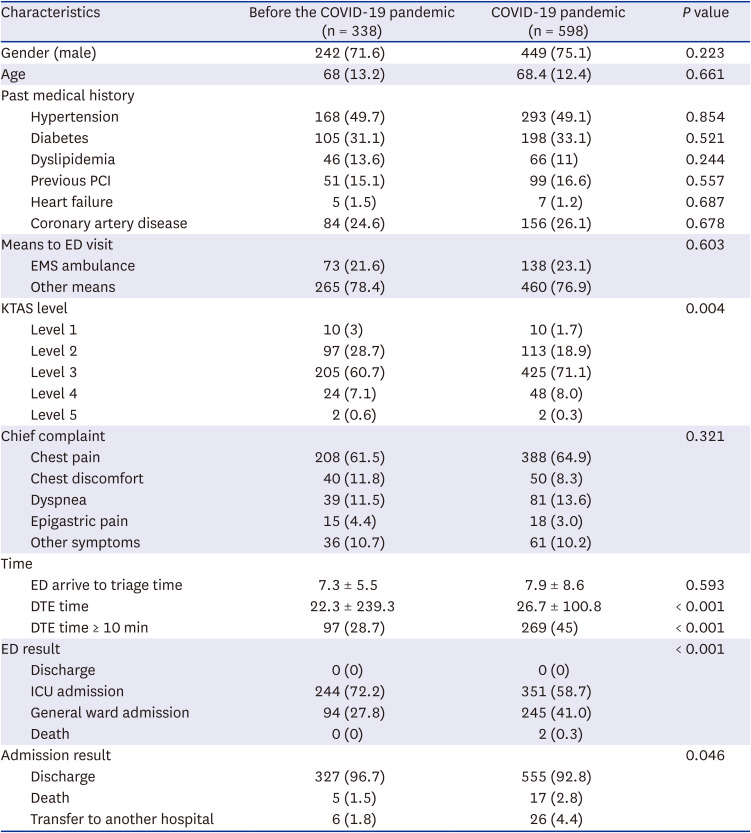
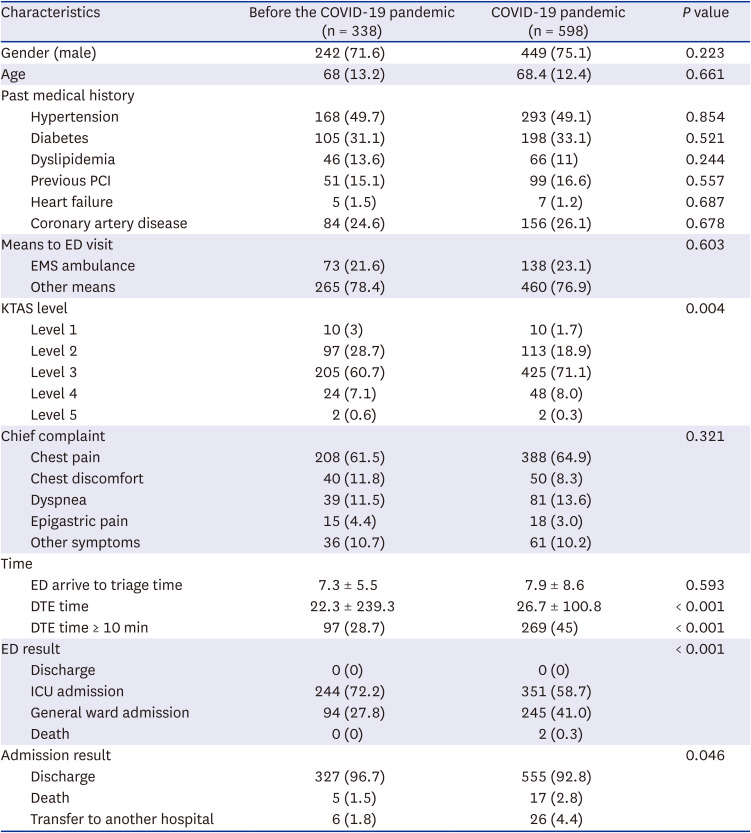
There were no significant differences in basic characteristics such as gender, age, and past medical history between patients with NSTEMI before and after the COVID-19 pandemic. However, after the pandemic, there was a significant increase in the mean DTE time and the proportion of DTEs greater than 10 minutes. Additionally, the proportion of normal discharges after hospitalization decreased compared to the period before the pandemic (
Table 3).
Table 3
Comparison of non-ST segment elevation myocardial infarction patient baseline characteristics and clinical outcomes in pre-pandemic and pandemic periods
|
Characteristics |
Before the COVID-19 pandemic (n = 338) |
COVID-19 pandemic (n = 598) |
P value |
|
Gender (male) |
242 (71.6) |
449 (75.1) |
0.223 |
|
Age |
68 (13.2) |
68.4 (12.4) |
0.661 |
|
Past medical history |
|
|
|
|
Hypertension |
168 (49.7) |
293 (49.1) |
0.854 |
|
Diabetes |
105 (31.1) |
198 (33.1) |
0.521 |
|
Dyslipidemia |
46 (13.6) |
66 (11) |
0.244 |
|
Previous PCI |
51 (15.1) |
99 (16.6) |
0.557 |
|
Heart failure |
5 (1.5) |
7 (1.2) |
0.687 |
|
Coronary artery disease |
84 (24.6) |
156 (26.1) |
0.678 |
|
Means to ED visit |
|
|
0.603 |
|
EMS ambulance |
73 (21.6) |
138 (23.1) |
|
Other means |
265 (78.4) |
460 (76.9) |
|
KTAS level |
|
|
0.004 |
|
Level 1 |
10 (3) |
10 (1.7) |
|
Level 2 |
97 (28.7) |
113 (18.9) |
|
Level 3 |
205 (60.7) |
425 (71.1) |
|
Level 4 |
24 (7.1) |
48 (8.0) |
|
Level 5 |
2 (0.6) |
2 (0.3) |
|
Chief complaint |
|
|
0.321 |
|
Chest pain |
208 (61.5) |
388 (64.9) |
|
Chest discomfort |
40 (11.8) |
50 (8.3) |
|
Dyspnea |
39 (11.5) |
81 (13.6) |
|
Epigastric pain |
15 (4.4) |
18 (3.0) |
|
Other symptoms |
36 (10.7) |
61 (10.2) |
|
Time |
|
|
|
|
ED arrive to triage time |
7.3 ± 5.5 |
7.9 ± 8.6 |
0.593 |
|
DTE time |
22.3 ± 239.3 |
26.7 ± 100.8 |
< 0.001 |
|
DTE time ≥ 10 min |
97 (28.7) |
269 (45) |
< 0.001 |
|
ED result |
|
|
< 0.001 |
|
Discharge |
0 (0) |
0 (0) |
|
ICU admission |
244 (72.2) |
351 (58.7) |
|
General ward admission |
94 (27.8) |
245 (41.0) |
|
Death |
0 (0) |
2 (0.3) |
|
Admission result |
|
|
0.046 |
|
Discharge |
327 (96.7) |
555 (92.8) |
|
Death |
5 (1.5) |
17 (2.8) |
|
Transfer to another hospital |
6 (1.8) |
26 (4.4) |
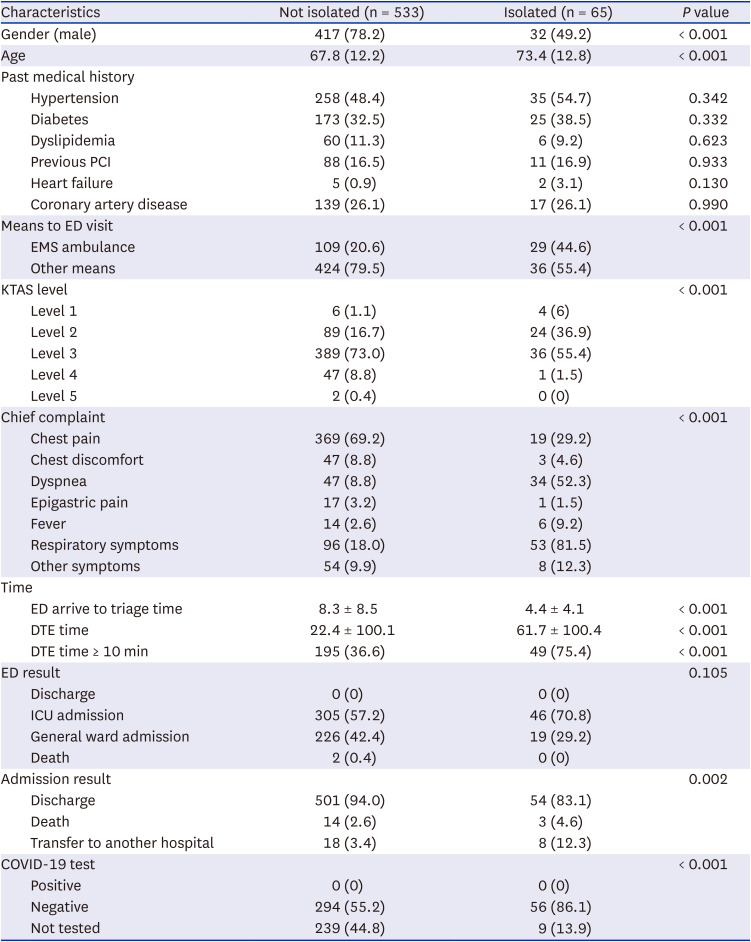
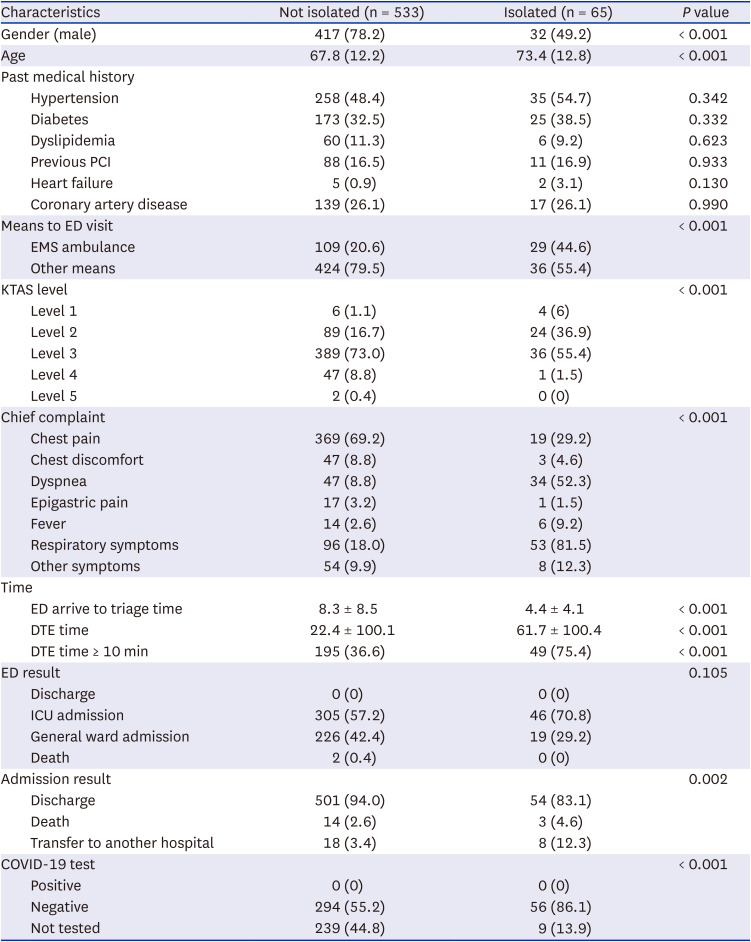
In the NSTEMI group, comparison of the isolated and non-isolated groups showed that the isolated group had a higher proportion of females and older patients. The isolated group had a higher percentage of patients who used EMS ambulance services, higher triage level, more cases of dyspnea, respiratory symptoms, and fever. The isolated group had a longer mean DTE time and a significantly higher proportion of DTEs greater than 10 minutes compared to the non-isolated group. There was a more significant delay in DTE time in the isolated group, and none of the NSTEMI patients were diagnosed with COVID-19 during the study period (
Table 4).
Table 4
Comparison of non-ST segment elevation myocardial infarction patient baseline characteristics and clinical outcomes by isolation status
|
Characteristics |
Not isolated (n = 533) |
Isolated (n = 65) |
P value |
|
Gender (male) |
417 (78.2) |
32 (49.2) |
< 0.001 |
|
Age |
67.8 (12.2) |
73.4 (12.8) |
< 0.001 |
|
Past medical history |
|
|
|
|
Hypertension |
258 (48.4) |
35 (54.7) |
0.342 |
|
Diabetes |
173 (32.5) |
25 (38.5) |
0.332 |
|
Dyslipidemia |
60 (11.3) |
6 (9.2) |
0.623 |
|
Previous PCI |
88 (16.5) |
11 (16.9) |
0.933 |
|
Heart failure |
5 (0.9) |
2 (3.1) |
0.130 |
|
Coronary artery disease |
139 (26.1) |
17 (26.1) |
0.990 |
|
Means to ED visit |
|
|
< 0.001 |
|
EMS ambulance |
109 (20.6) |
29 (44.6) |
|
Other means |
424 (79.5) |
36 (55.4) |
|
KTAS level |
|
|
< 0.001 |
|
Level 1 |
6 (1.1) |
4 (6) |
|
Level 2 |
89 (16.7) |
24 (36.9) |
|
Level 3 |
389 (73.0) |
36 (55.4) |
|
Level 4 |
47 (8.8) |
1 (1.5) |
|
Level 5 |
2 (0.4) |
0 (0) |
|
Chief complaint |
|
|
< 0.001 |
|
Chest pain |
369 (69.2) |
19 (29.2) |
|
Chest discomfort |
47 (8.8) |
3 (4.6) |
|
Dyspnea |
47 (8.8) |
34 (52.3) |
|
Epigastric pain |
17 (3.2) |
1 (1.5) |
|
Fever |
14 (2.6) |
6 (9.2) |
|
Respiratory symptoms |
96 (18.0) |
53 (81.5) |
|
Other symptoms |
54 (9.9) |
8 (12.3) |
|
Time |
|
|
|
|
ED arrive to triage time |
8.3 ± 8.5 |
4.4 ± 4.1 |
< 0.001 |
|
DTE time |
22.4 ± 100.1 |
61.7 ± 100.4 |
< 0.001 |
|
DTE time ≥ 10 min |
195 (36.6) |
49 (75.4) |
< 0.001 |
|
ED result |
|
|
0.105 |
|
Discharge |
0 (0) |
0 (0) |
|
ICU admission |
305 (57.2) |
46 (70.8) |
|
General ward admission |
226 (42.4) |
19 (29.2) |
|
Death |
2 (0.4) |
0 (0) |
|
Admission result |
|
|
0.002 |
|
Discharge |
501 (94.0) |
54 (83.1) |
|
Death |
14 (2.6) |
3 (4.6) |
|
Transfer to another hospital |
18 (3.4) |
8 (12.3) |
|
COVID-19 test |
|
|
< 0.001 |
|
Positive |
0 (0) |
0 (0) |
|
Negative |
294 (55.2) |
56 (86.1) |
|
Not tested |
239 (44.8) |
9 (13.9) |
Patients’ chief complaints were subdivided into classic symptoms (chest pain, chest discomfort, and dyspnea) and atypical symptoms (epigastric pain, fever, respiratory symptoms, and other symptoms) for comparison. In both periods, regardless of the duration of the COVID-19 pandemic, patients with atypical symptoms had a statistically significant delay in DTE time and a higher proportion of patients who died after hospitalization (
Supplementary Table 1).
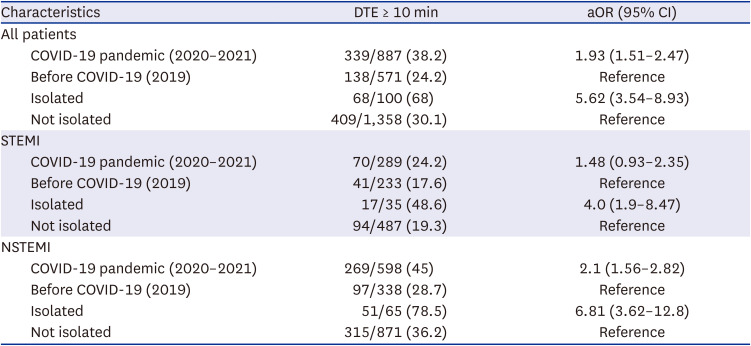
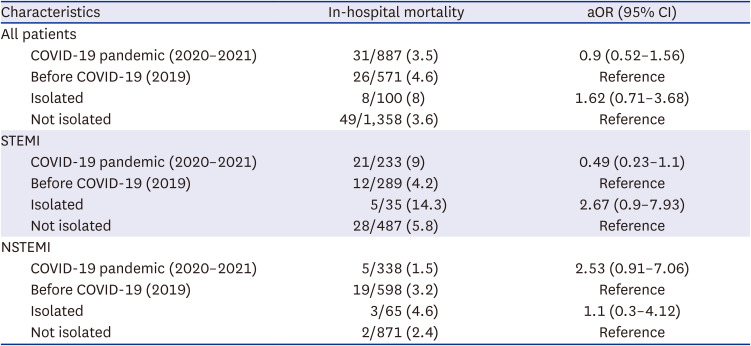
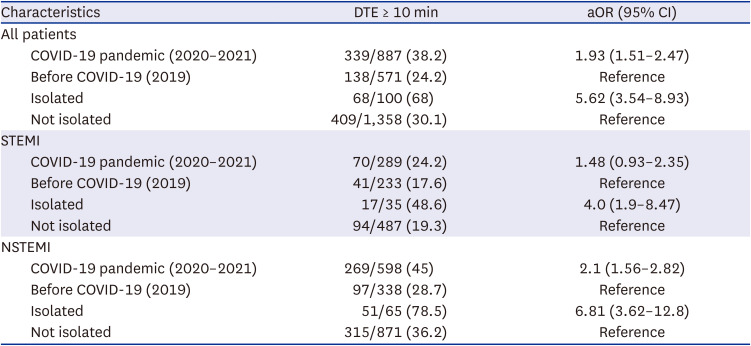
We conducted a multivariate logistic regression analysis to examine the impact of the COVID-19 pandemic and isolation on DTE times greater than 10 minutes. The results revealed that both variables had a statistically significant effect size, with pandemic adjusted odds ratio (aOR) of 1.93 (95% confidence interval [CI], 1.51–2.47) and isolation aOR of 5.62 (95% CI, 3.54–8.93). This association was observed consistently in both STEMI and NSTEMI patients, except for the pandemic variable in the STEMI group (
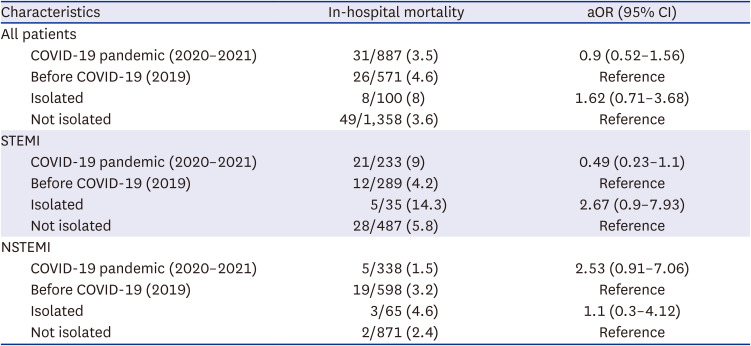
Table 5). However, in the multivariate logistic regression analysis of the impact of pandemic and isolation on in-hospital mortality, no significant effect size was observed for either variable (
Table 6).
Table 5
Multivariate logistic regression analysis of the effect of the COVID-19 pandemic and isolation status on DTE > 10 minutes
|
Characteristics |
DTE ≥ 10 min |
aOR (95% CI) |
|
All patients |
|
|
|
COVID-19 pandemic (2020–2021) |
339/887 (38.2) |
1.93 (1.51–2.47) |
|
Before COVID-19 (2019) |
138/571 (24.2) |
Reference |
|
Isolated |
68/100 (68) |
5.62 (3.54–8.93) |
|
Not isolated |
409/1,358 (30.1) |
Reference |
|
STEMI |
|
|
|
COVID-19 pandemic (2020–2021) |
70/289 (24.2) |
1.48 (0.93–2.35) |
|
Before COVID-19 (2019) |
41/233 (17.6) |
Reference |
|
Isolated |
17/35 (48.6) |
4.0 (1.9–8.47) |
|
Not isolated |
94/487 (19.3) |
Reference |
|
NSTEMI |
|
|
|
COVID-19 pandemic (2020–2021) |
269/598 (45) |
2.1 (1.56–2.82) |
|
Before COVID-19 (2019) |
97/338 (28.7) |
Reference |
|
Isolated |
51/65 (78.5) |
6.81 (3.62–12.8) |
|
Not isolated |
315/871 (36.2) |
Reference |
Table 6
Multivariate logistic regression analysis of the effect of the COVID-19 pandemic and isolation status on in-hospital mortality
|
Characteristics |
In-hospital mortality |
aOR (95% CI) |
|
All patients |
|
|
|
COVID-19 pandemic (2020–2021) |
31/887 (3.5) |
0.9 (0.52–1.56) |
|
Before COVID-19 (2019) |
26/571 (4.6) |
Reference |
|
Isolated |
8/100 (8) |
1.62 (0.71–3.68) |
|
Not isolated |
49/1,358 (3.6) |
Reference |
|
STEMI |
|
|
|
COVID-19 pandemic (2020–2021) |
21/233 (9) |
0.49 (0.23–1.1) |
|
Before COVID-19 (2019) |
12/289 (4.2) |
Reference |
|
Isolated |
5/35 (14.3) |
2.67 (0.9–7.93) |
|
Not isolated |
28/487 (5.8) |
Reference |
|
NSTEMI |
|
|
|
COVID-19 pandemic (2020–2021) |
5/338 (1.5) |
2.53 (0.91–7.06) |
|
Before COVID-19 (2019) |
19/598 (3.2) |
Reference |
|
Isolated |
3/65 (4.6) |
1.1 (0.3–4.12) |
|
Not isolated |
2/871 (2.4) |
Reference |
DISCUSSION
In this study, we investigated the impact of the COVID-19 pandemic on the DTE time of MI patients in a single ED. Our findings suggest that the pandemic significantly delayed the DTE time of MI patients, with ED isolation having an even greater impact on delaying DTE time. Although adjustments were made for confounding variables, the proportion of patients with a DTE time of 10 minutes or more showed a significant increase during the pandemic for both STEMI and NSTEMI. However, we did not observe a clear impact of the pandemic or isolation on in-hospital mortality.
The importance of EDs in the triage and diagnosis of patients with STEMI cannot be overstated.
9 Early ECGs are recommended for all patients with possible cardiac chest pain.
12 The increased time taken by EMS providers to wear personal protective equipment (PPE) for COVID-19 and test for COVID-19,
13 as well as clinical factors such as the need to identify infected patients, contributed to the delay in DTE time.
9 In addition, screening and isolation protocols in EDs have changed throughout the COVID-19 pandemic, potentially causing delays in activating care for MI patients.
14 Studies have shown that infection control measures during the pandemic in EDs can delay the time to hospitalization for STEMI patients,
8 which can ultimately lead to adverse clinical outcomes.
15
We identified two main reasons for the delay in DTE time in our study. First, in the early stages of the pandemic, the screening process prioritized the identification of COVID-19, resulting in delays in DTE time as the decision to isolate or not was made before ECG testing. The second reason is related to personal protection, with a significant increase in DTE time observed for both STEMI and NSTEMI patients admitted to ED isolation rooms due to the time it takes for patients to enter the isolation area and for healthcare workers to don PPE.
The COVID-19 pandemic has caused delays in emergency patient care.
161718 Delays in DTE and DTB time have occurred since the pandemic, with healthcare providers prioritizing epidemiologic investigations and lung CT scans to rule out COVID-19. Delayed treatment may occur when symptoms are not evident, leading to delays in DTB time.
19 Furthermore, delays from first medical contact to PCI in STEMI patients have been observed in previous studies after the pandemic, leading to increased mortality and complication rates.
20 In our study, we observed delays in both DTE and DTB times in isolated STEMI patients during the pandemic. These findings support previous studies on the impact of the COVID-19 pandemic on delayed DTB time.
During the COVID-19 pandemic, stroke patients experienced delays in their onset-to-needle time due to COVID-19 prevention procedures, such as obtaining travel and contact history, taking temperatures, performing chest X-rays or CT, testing for coronavirus antibodies, and donning PPE by healthcare workers.
21 The COVID-19 pandemic also caused delays in imaging processes critical to the diagnosis and outcome of acute cerebrovascular disease patients, and COVID-19 testing has caused delays in ED length of stay.
22
While triage methods focusing solely on chest pain symptoms may fail to recognize STEMI, an ECG call system has been shown to reduce missed STEMIs.
23 In this study, despite the presence of an ECG call system after triage, DTE time was delayed due to the COVID-19 screening process. Atypical symptoms such as dyspnea, syncope, gastrointestinal discomfort, or weakness can also delay DTE time,
23 and patients without chest pain have been shown to have significantly longer arrival times at emergency medical centers and delayed ECG compared to patients with chest pain.
24 In our study, we found that in patients presenting to the ED with atypical symptoms, DTE time was delayed regardless of the COVID-19 pandemic. During the COVID-19 pandemic, patients with non-specific symptoms such as dyspnea may be screened and admitted to an isolation room, which can delay DTE.
Studies have shown that there are differences in ECG testing times depending on the mode of transportation. Delays in DTE have been reported in patients with chest pain who drive themselves to an ED rather than take an ambulance.
25 In this study, DTE time was delayed in patients who presented to the ED by EMS ambulances after the COVID-19 pandemic. Although the cause is difficult to extrapolate, it is suggested that EMS providers have more information to screen for COVID-19, which increases the likelihood that they will be tested or isolated.
The question is whether there was an actual delay in performing an ECG or detecting a STEMI. There may be instances where a 12-lead ECG is performed in the prehospital setting on a patient with chest pain, or where a patient arrives from another hospital with a diagnosis of STEMI. The South Korean National Fire Agency is conducting a pilot project that will allow trained and adequately staffed EMS providers to perform 12-lead ECGs starting in winter 2019. However, as of early 2020, in response to the COVID-19 pandemic, EMS providers in the region where the study was conducted are known to have performed very few actual 12-lead ECGs. Therefore, it is likely that very few patients presented to the hospital where this study was conducted with a prehospital 12-lead ECG. When we further analyzed the data, we found that the DTE for patients who used an EMS ambulance was 31.6 minutes, while the DTE for other patients was 14.2 minutes, indicating that calling 119 was associated with a delay in DTE. Even if STEMI was diagnosed with a 12-lead ECG prior to the ED visit, the hospitals in the study still require these patients to undergo an emergency 12-lead ECG with the same protocol. Therefore, we believe it is unlikely that the presence of a prior diagnosis affected DTE time.
In this study, the COVID-19 pandemic delayed DTE time in STEMI or NSTEMI patients and delayed DTB time in STEMI patients. In STEMI patients, isolation increased mean DTE and DTB times by approximately 15 and 75 minutes, respectively, compared with nonisolation. However, multivariate logistic regression did not show a significant aOR. The difference in in-hospital mortality was more than 2-fold, with isolation at 14.3% and non-isolation at 5.8%. We suggest that perhaps the small number of patients did not allow for statistical significance. When analyzed separately among patients with isolated STEMI, the difference in in-hospital mortality was 0.5% for patients with DTB < 90 minutes and 4% for patients with DTB ≥ 90 minutes.
We believe that the lack of significant differences in hospital outcomes is due to the efforts of the hospitals where the study was conducted to maintain an overall high level of care in the context of COVID-19. To overcome delays in DTE and DTB times, the ED where this study was conducted made efforts to reduce delays through internal system changes in response to the COVID-19 pandemic. Efforts such as prioritizing ECGs when indicated in isolated patients minimized delays in DTE time, and the level of care provided after diagnosis was not significantly affected by the COVID-19 pandemic, which may explain why there was no clear difference in hospitalization outcomes.
This study has limitations, including being limited to patients presenting to a single ED in a large urban area, and differences in screening processes and ECG testing policies in other EDs may lead to different results. Patients with other cardiac problems that could be diagnosed by ECG other than MI were excluded, which may have affected the study’s findings. Approximately 25% of patients in the COVID-19 diagnosis variable were not tested, but it can be assumed that these patients were not diagnosed with COVID-19 because they did not have any relevant clinical evidence. Even among patients who were ultimately deemed not to be in isolation, there may have been cases where it took some time for a decision to be made, and it is possible that some not-isolated patients were delayed.
It is possible that the time of 12-lead ECG acquisition in the ED was different from the time of physician review. While the time of 12-lead ECG acquisition was accurately recorded, the time of physician review was not measurable. Therefore, we cannot exclude the possibility that the actual DTE time was delayed more than the measured DTE time. However, since the protocol in the ED calls for direct reporting to the physician immediately after 12-ECG acquisition, we believe that this problem is rare.
The study did not evaluate delays in the prehospital setting. Prehospital delays have been reported since the COVID-19 pandemic.
26 As the results of our study show, isolated patients are often transported by EMS ambulance. Therefore, it is possible that delays in the prehospital phase may have further affected final care.
Finally, the retrospective cross-sectional analysis used in this study has limitations in determining causality, and it would be difficult to conduct this study in the form of a randomized controlled trial due to its nature.
The findings of this study suggest that COVID-19 screening and isolation protocols in EDs have led to delays in DTE time for MI patients, which could ultimately lead to adverse clinical outcomes. Therefore, it is crucial to ensure that emergency patients receive timely evaluation and treatment, and care should be taken to minimize any potential delays caused by pandemic-related policies. Healthcare providers and policymakers should consider these implications when planning and implementing pandemic response strategies to ensure that emergency patients receive the care they need without delay.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download