Abstract
Geographical and racial factors constitute important distinctions between Kawasaki disease (KD) and multisystem inflammatory syndrome in children (MIS-C), but no study has been conducted in Vietnam. Forty-one children with KD from January 2018 to July 2020 and 42 with KD/MIS-C from August 2020 to December 2022 were included in this study. Of the patients, 52.3% were aged between 12 and 35 months. Only two were aged over 5 years, and both were belong to the KD/MIS-C group. A 59.5% of the patients were male. Apart from fever, all symptoms tended to be more frequent in patients with KD/MIS-C. The prevalence of diffuse skin rash, hand and foot edema or erythema and gastrointestinal signs was significantly higher in patients hospitalized with KD/MIS-C. There was no significant difference in laboratory findings between the two groups. Coronary artery dilation was more frequently observed in patients with KD/MIS-C compared to those with KD (40.5% vs. 14.6%, P = 0.009).
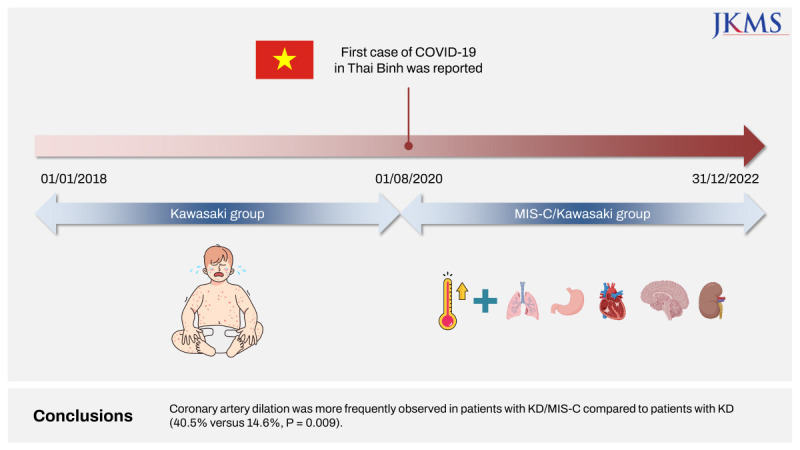
Graphical Abstract
Kawasaki disease (KD) and multisystem inflammatory syndrome in children (MIS-C) are both acute febrile vasculitis conditions that primarily affect children.12 MIS-C, on the other hand, is a newly recognized post-infectious syndrome that has been associated with coronavirus disease 2019 (COVID-19) in children. Both diseases share many clinical features such as fever, rash, and mucocutaneous involvement, and can affect multiple organ systems.12345678910111213141516 Given the similarities and differences between KD and MIS-C, there is a need for a comparative study of their clinical and laboratory characteristics to better understand the underlying pathophysiology of the two diseases and to identify potential diagnostic and therapeutic targets. Several studies have compared the clinical and laboratory features of KD and MIS-C, but the results have been inconsistent and often limited by small sample sizes and methodological heterogeneity. Moreover, previous studies were mostly theoretical overviews.1245678910
On the other hand, geographical and racial factors constitute important distinctions between KD and MIS-C,1 but no study has been conducted in Vietnam. Therefore, we conducted a five-year retrospective study to investigate the differences in clinical and laboratory findings between children under 16 with KD and MIS-C in Thai Binh Pediatric Hospital, Vietnam. The inclusion criteria were KD or MIS-C patients who were hospitalized from January 1, 2018 to December 31, 2022. KD was diagnosed based on the 2017 American Heart Association guidelines.17 MIS-C was diagnosed according to the guideline of Centers for Disease Control and Prevention.18 The following data were collected from the central computer of the hospital: age, sex, clinical features, laboratory findings, and transthoracic echocardiography results.
Due to the unavailability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) serology, we could not assess prior SARS-CoV-2 infection. Therefore, we classified patients based on the time of diagnosis with regards to the dynamic of the COVID-19 outbreak. In Thai Binh, the first case of COVID-19 was reported on August 1, 2020. Patients fulfilling clinical criteria of KD and admitted between January 1, 2018 and July 31, 2020 were classified as KD. Patients hospitalized from August 1, 2020 to December 31, 2022 were classified as KD/MIS-C. This classification has also been used in previous studies.1214192021A total of 83 children who met the inclusion criteria were selected for the study. Among them, 41 (49.4%) were diagnosed with KD during the pre-COVID-19 pandemic period from January 2018 to July 2020, while 42 (50.6%) were diagnosed with KD/MIS-C from August 2020 to December 2022, after the beginning of COVID-19 outbreak in Thai Binh.
Most of the KD and KD/MIS-C patients were aged between 12 and 35 months (46.3% and 52.3%, respectively), followed by children aged under 12 months (34.2% and 38.1%, respectively) and those aged from 36 to 59 months (19.5% and 4.8%, respectively). Interestingly, only two children were aged > 5 years, and both were in the KD/MIS-C group. By sex, 68.3% of KD patients and 59.5% of KD/MIS-C patients were male. There were no significant differences in age and sex distributions between the two groups (P = 0.114 and 0.406, respectively by χ2 test).
The most prevalent clinical sign observed in both groups of patients was fever lasting at least 5 days, which was present in all patients. In patients with KD, the proportions of conjunctivitis, red and cracked lips, cervical lymphadenopathy, respiratory symptoms, and neurological symptoms were 75.6%, 87.8%, 65.9%, 39.0%, and 2.4%, respectively. In patients with KD/MIS-C, these proportions were 85.7%, 88.1%, 71.4%, 50.0%, and 9.8%, respectively. Except for fever, all other symptoms tended to be more frequent in patients with KD/MIS-C. Particularly, diffuse skin rash, hand and foot edema or erythema, and gastrointestinal symptoms were significantly more frequent in patients with KD/MIS-C than in KD patients. The proportions were 92.9% vs. 75.6% (P = 0.031), 71.4% vs. 46.3% (P value = 0.020), and 47.6% vs. 19.5% (P value = 0.007), respectively (χ2 test).
Among the patients, 61.9% had elevated white blood cell counts, 64.3% had normal platelet counts, and 64.3% exhibited elevated C-reactive protein (CRP) levels. Anemia was observed in the majority of patients. No significant differences in laboratory findings were found between patients with KD and KD/MIS-C (Table 1). Coronary artery dilation or aneurysm was more frequently observed in patients with KD/MIS-C compared to patients with KD (40.5% vs. 14.6%, P = 0.009, χ2 test). However, there was no difference in proportions of pericarditis and myocarditis between the two groups, although myocarditis was seen only in two patients with KD (Table 1).
Since the beginning of the COVID-19 pandemic, the cases of MIS-C have increased in Europe and North America.1 It is quite confusing that they have been less commonly described in Asia where COVID-19 first outbroke. The low incidence of MIS-C in Asia may be explained by several theories. One of the theories put forward is racial and genomic differences. Indeed, previous studies have shown that black children are at higher risk for MIS-C than Asian children.2223 Another theory that can be taken into account is the difference in the incidence and fatality rate of COVID-19 in Asia.24 In addition, underdiagnosis in settings with limited medical conditions may be a reason why less MIS-C cases were reported in Asia.
Despite overlapping clinical features, the differences in epidemiology, pathology, inflammation, and immunology between MIS-C and KD demonstrate that these two diseases are distinct entities.1925 Consequently, it is imperative to conduct a comparative analysis of the clinical and laboratory characteristics of KD and MIS-C. By identifying the similarities and disparities between these two diseases, we can develop more focused diagnostic and therapeutic approaches that may lead to improved outcomes of affected children.
KD usually occurs in children under the age of five, whereas the median age of MIS-C patients was 9 years.126 In our study, however, no difference was found in the age distribution between two groups, which might be attributed to the limited sample size. However, it is worth noting that two children aged over 5 were included, and both of them belonged to the KD/MIS-C group.
Regarding the differences in clinical and laboratory findings between KD and KD/MIS-C patients, our study found that the prevalence rates of diffuse skin rash, hand and foot oedema or erythema, gastrointestinal symptoms, and coronary dilatations or aneurysm were significantly higher in patients with KD/MIS-C. This is consistent with previous studies.12131427 In an Italian study including 96 patients with KD and 53 patients with KD/MIS-C, the authors showed that respiratory and gastrointestinal involvement was more common in KD/MIS-C children.12
Patients diagnosed with KD/MIS-C exhibit increased levels of CRP, ferritin, D-dimer, troponin, and N-terminal pro-brain natriuretic peptide in comparison to those diagnosed with KD.112 This disparity may suggest more severe inflammation and the possibility of more cardiovascular complications in KD/MIS-C than in KD. On the other hand, contrasting with KD patients, patients with KD/MIS-C had decreased counts of lymphocytes and platelets.12728
While patients with MIS-C may exhibit higher incidence of coronary artery abnormalities compared to KD patients, any observed abnormalities are typically transient and tend to resolve rapidly over time.1319 Conversely, in KD patients, it may take up to two years for small-to-medium aneurysms of the coronary arteries to regress to their normal sizes.293031 The quicker resolution of cardiovascular complications following the acute phase of MIS-C suggests that these complications may arise from hyperinflammation, capillary leakage and vasodilation, rather than infiltration of immune cells causing direct injury to myocardium and coronary arteries. Cattalini et al.12 also discovered that cardiac involvement was more common in the KD/MIS-C group, with over 60% of patients exhibiting myocarditis.
It is important to note that this study has several limitations. First, the sample size is relatively small, which may limit the generalizability of the findings. Secondly, the study was conducted in a specific geographic region and did not fully represent the whole population of Vietnam. Thirdly, we couldn't accurately distinguish MIS-C patients from KD patients like in several previous studies,1213192021 therefore, we classified all children with symptoms of these two diseases as KD/MIS-C patients since the onset of the COVID-19 pandemic. It was very likely to induce systematic bias in sampling and affect the results of comparison between KD and KD/MIS-C. Finally, we did not follow-up the patients after discharge, so we could not assess the patient's long-term outcomes in the two groups.
In conclusion, despite the small sample size, our study is the first report on MIS-C in Vietnam. This work will contribute to the existing knowledge by comparing the clinical and laboratory characteristics of KD and KD/MIS-C. The findings emphasize the need for early recognition, prompt management, and close cardiac monitoring in children with COVID-19-related inflammatory syndromes. Further research is warranted to enhance our understanding of these conditions and improve the outcomes of patients.
The study was performed according to the good clinical practices recommended by the Declaration of Helsinki and its amendments, and approved by the Institutional Review Board of Thai Binh University of Medicine and Pharmacy (Protocol code 616, date of approval: April 26, 2023). We did not collect patient identifiers. All information obtained is kept confidential and used for research purposes only. Only researchers have access to the data. Because this was a retrospective cohort study that reviewed the medical records only, informed consent was waved.
ACKNOWLEDGMENTS
The authors thank Dr. Manh Tuong Nguyen and Dr. Thu Hang Ha for their help in collection of data.
Notes
Author Contributions:
Conceptualization: Phi DL, Dao TL, Hoang VT, Gautret P.
Data curation: Phi DL, Dao TL, To MM, Nguyen TB, Nguyen DC.
Formal analysis: Phi DL, Dao TL, To MM, Nguyen TB, Nguyen DC, Gautret P.
Investigation: Phi DL, Dao TL, To MM, Nguyen TB, Nguyen DC, Gautret P, Hoang VT.
Methodology: Phi DL, Dao TL, Hoang VT, Gautret P.
Software: Dao TL, Hoang VT.
Validation: Phi DL, Dao TL, Hoang VT, Gautret P.
Visualization: Hoang VT.
Writing - original draft: Phi DL, Dao TL, Hoang VT, Gautret P.
Writing - review & editing:.
References
1. Noval Rivas M, Arditi M. Kawasaki disease and multisystem inflammatory syndrome in children. Rheum Dis Clin North Am. 2023; 49(3):647–659. PMID: 37331738.
2. Gkoutzourelas A, Bogdanos DP, Sakkas LI. Kawasaki disease and COVID-19. Mediterr J Rheumatol. 2020; 31(Suppl 2):268–274. PMID: 33196004.
3. Patel JM. Multisystem inflammatory syndrome in children (MIS-C). Curr Allergy Asthma Rep. 2022; 22(5):53–60. PMID: 35314921.
4. Chen MR, Kuo HC, Lee YJ, Chi H, Li SC, Lee HC, et al. Phenotype, susceptibility, autoimmunity, and immunotherapy between Kawasaki disease and coronavirus disease-19 associated multisystem inflammatory syndrome in children. Front Immunol. 2021; 12:632890. PMID: 33732254.
5. Kabeerdoss J, Pilania RK, Karkhele R, Kumar TS, Danda D, Singh S. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol Int. 2021; 41(1):19–32. PMID: 33219837.
6. Lee MS, Liu YC, Tsai CC, Hsu JH, Wu JR. Similarities and differences between COVID-19-related multisystem inflammatory syndrome in children and Kawasaki disease. Front Pediatr. 2021; 9:640118. PMID: 34222140.
7. Sharma C, Ganigara M, Galeotti C, Burns J, Berganza FM, Hayes DA, et al. Multisystem inflammatory syndrome in children and Kawasaki disease: a critical comparison. Nat Rev Rheumatol. 2021; 17(12):731–748. PMID: 34716418.
8. Wessels PA, Bingler MA. A comparison of Kawasaki disease and multisystem inflammatory syndrome in children. Prog Pediatr Cardiol. 2022; 65:101516. PMID: 35313700.
9. Yeo WS, Ng QX. Distinguishing between typical Kawasaki disease and multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2. Med Hypotheses. 2020; 144:110263. PMID: 33254568.
10. Zhang QY, Xu BW, Du JB. Similarities and differences between multiple inflammatory syndrome in children associated with COVID-19 and Kawasaki disease: clinical presentations, diagnosis, and treatment. World J Pediatr. 2021; 17(4):335–340. PMID: 34013488.
11. Bar-Meir M, Guri A, Godfrey ME, Shack AR, Hashkes PJ, Goldzweig O, et al. Characterizing the differences between multisystem inflammatory syndrome in children and Kawasaki disease. Sci Rep. 2021; 11(1):13840. PMID: 34226639.
12. Cattalini M, Della Paolera S, Zunica F, Bracaglia C, Giangreco M, Verdoni L, et al. Defining Kawasaki disease and pediatric inflammatory multisystem syndrome-temporally associated to SARS-CoV-2 infection during SARS-CoV-2 epidemic in Italy: results from a national, multicenter survey. Pediatr Rheumatol Online J. 2021; 19(1):29. PMID: 33726806.
13. Esteve-Sole A, Anton J, Pino-Ramirez RM, Sanchez-Manubens J, Fumadó V, Fortuny C, et al. Similarities and differences between the immunopathogenesis of COVID-19-related pediatric multisystem inflammatory syndrome and Kawasaki disease. J Clin Invest. 2021; 131(6):131.
14. Pick JM, Wang S, Wagner-Lees S, Badran S, Szmuszkovicz JR, Wong P, et al. Abstract 17092: coronary artery aneurysms are more common in post-COVID-19 multisystem inflammatory syndrome in children (MIS-C) than pre-pandemic Kawasaki disease. Circulation. 2020; 142(Suppl_3):A17092–A17092.
15. Rashid U, Nawaz R, Mahmood T, et al. Multisystem inflammatory syndrome (MIS-C) in children on Kawasaki syndrome spectrum: what’s new, local regional experience from Pakistan. Prof Med J. 2022; 29(9):1392–1399.
16. Zhou C, Zhao Y, Wang X, Huang Y, Tang X, Tang L. Laboratory parameters between multisystem inflammatory syndrome in children and Kawasaki disease. Pediatr Pulmonol. 2021; 56(12):3688–3698. PMID: 34583417.
17. McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017; 135(17):e927–e999. PMID: 28356445.
18. Centers for Disease Control and Prevention. Multisystem inflammatory syndrome (MIS). Updated 2020. Accessed June 19, 2023.
https://www.cdc.gov/mis/mis-c/hcp_cstecdc/index.html
.
19. Godfred-Cato S, Abrams JY, Balachandran N, Jaggi P, Jones K, Rostad CA, et al. Distinguishing multisystem inflammatory syndrome in children from COVID-19, Kawasaki disease and toxic shock syndrome. Pediatr Infect Dis J. 2022; 41(4):315–323. PMID: 35093995.
20. Cherqaoui B, Koné-Paut I, Yager H, Bourgeois FL, Piram M. Delineating phenotypes of Kawasaki disease and SARS-CoV-2-related inflammatory multisystem syndrome: a French study and literature review. Rheumatology (Oxford). 2021; 60(10):4530–4537. PMID: 33493353.
21. Fabi M, Filice E, Biagi C, Andreozzi L, Palleri D, Mattesini BE, et al. Multisystem inflammatory syndrome following SARS-CoV-2 infection in children: one year after the onset of the pandemic in a high-incidence area. Viruses. 2021; 13(10):2022. PMID: 34696451.
22. Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020; 324(3):259–269. PMID: 32511692.
23. Middelburg JG, Crijnen TEM, D’Antiga L, Verdoni L, Chikermane A, Garg P, et al. Association of ethnicity with multisystem inflammatory syndrome in children related to SARS-CoV-2 infection: an international case-referent study. Front Pediatr. 2021; 9:707650. PMID: 34722416.
24. Li W, Tang Y, Shi Y, Chen Y, Liu E. Why multisystem inflammatory syndrome in children has been less commonly described in Asia? Transl Pediatr. 2020; 9(6):873–875. PMID: 33457311.
25. Rowley AH. Multisystem inflammatory syndrome in children and Kawasaki disease: two different illnesses with overlapping clinical features. J Pediatr. 2020; 224:129–132. PMID: 32585239.
26. Belay ED, Abrams J, Oster ME, Giovanni J, Pierce T, Meng L, et al. Trends in geographic and temporal distribution of US children with multisystem inflammatory syndrome during the COVID-19 pandemic. JAMA Pediatr. 2021; 175(8):837–845. PMID: 33821923.
27. Consiglio CR, Cotugno N, Sardh F, Pou C, Amodio D, Rodriguez L, et al. The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. 2020; 183(4):968–981.e7. PMID: 32966765.
28. Olin A, Henckel E, Chen Y, Lakshmikanth T, Pou C, Mikes J, et al. Stereotypic immune system development in newborn children. Cell. 2018; 174(5):1277–1292.e14. PMID: 30142345.
29. Matsubara D, Kauffman HL, Wang Y, Calderon-Anyosa R, Nadaraj S, Elias MD, et al. Echocardiographic findings in pediatric multisystem inflammatory syndrome associated with COVID-19 in the United States. J Am Coll Cardiol. 2020; 76(17):1947–1961. PMID: 32890666.
30. Farooqi KM, Chan A, Weller RJ, Mi J, Jiang P, Abrahams E, et al. Longitudinal outcomes for multisystem inflammatory syndrome in children. Pediatrics. 2021; 148(2):e2021051155. PMID: 34266903.
31. Advani N, Sastroasmoro S, Ontoseno T, Uiterwaal CS. Long-term outcome of coronary artery dilatation in Kawasaki disease. Ann Pediatr Cardiol. 2018; 11(2):125–129. PMID: 29922008.
Table 1
Laboratory findings and cardiovascular injury in patients with KD and KD/MIS-C
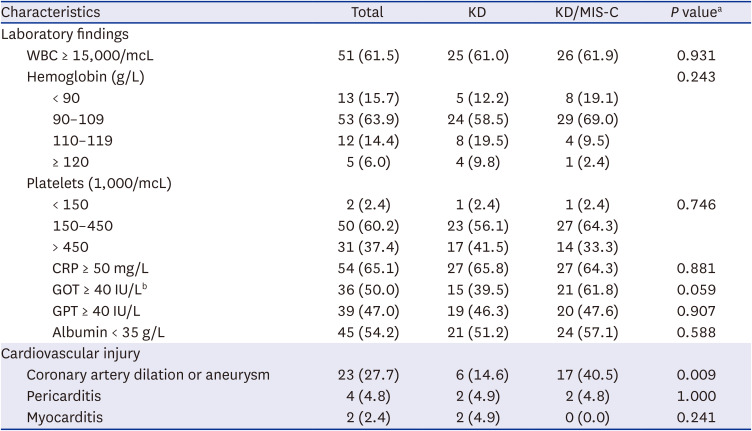
Values are presented as number (%).
KD = Kawasaki disease, MIS-C = multisystem inflammatory syndrome in children, WBC = white blood count, CRP = C-reactive protein, GOT = glutamic oxaloacetic transaminase, GPT = glutamic pyruvic transaminase.
aBy χ2 test or Fisher exact test; bData missing in 3 KD patients and 8 KD/MIS-C patients.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download