INTRODUCTION
According to the World Health Organization, the estimated global prevalence of congenital anomalies ranges from 1–5%, depending on the region and population studied.
1 Although the overall mortality rate associated with congenital anomalies is declining, approximately 17–42% of infant mortalities are still attributed to congenital anomalies.
1 Congenital anomalies in the digestive system can be fatal in the absence of timely surgical care, therefore, a multidisciplinary approach is required for the timely management of these conditions.
2
In general, children with congenital anomalies in the digestive system are at risk of developmental delays, feeding difficulties, and other complications. Feeding difficulties can result from the inability of an infant to properly swallow or digest food, while delayed or impaired bowel function can result in constipation, diarrhea, and other digestive problems.
34 These problems, in turn, can lead to malnutrition and failure to thrive. Moreover, surgical treatment for congenital gastrointestinal anomalies can affect the developmental outcome of a child.
4
A Korean study of very low birth weight infants found that the two most common types of congenital anomalies were those of the digestive system (31.7%) and the heart (27.7%).
5 In the European network of population-based registries for the epidemiological surveillance of congenital anomalies (EUROCAT), the prevalence of major congenital gastrointestinal anomalies from 2008 to 2012 was 2.1 per 10,000 live births, with the most common subgroups being anorectal atresia and/or stenosis, followed by esophageal atresia with or without tracheoesophageal fistula, diaphragmatic hernia, Hirschsprung’s disease, and duodenal atresia or stenosis.
6
Abdominal wall defects, also known as ventral wall defects or omphalocele, may result in protrusion of abdominal organs outside the body.
7 The estimated prevalence of abdominal wall defects is approximately 1 in 2,500 to 1 in 5,000 live births worldwide and 3.6 per 10,000 live births in EUROCAT (for gastroschisis [2.3 per 10,000 live births] and omphalocele [1.2 per 10,000 live births]).
8 The prevalence of abdominal wall defects may be positively related to maternal smoking and negatively related to maternal age and socioeconomic status.
9 Prompt diagnosis and management are critical to improve outcomes in infants with abdominal wall defects. Their growth outcomes depend on several factors, including the type and severity of the defect, associated anomalies, and overall health. In general, infants with abdominal wall defects have higher rates of growth delay, malnutrition, and developmental delay than infants without abdominal wall defects.
10
Although, congenital anomalies in the digestive system and abdominal wall defects are relatively rare, they can significantly impact the health and quality of life of an individual. Nevertheless, information about the long-term outcomes of infants with congenital anomalies in the digestive system and abdominal wall defects requiring surgery is limited. Thus, the aim of this study was to analyze the prevalence and long-term growth and developmental outcomes of infants with congenital anomalies in the digestive system and with abdominal wall defects who underwent surgery in Korea.
METHODS
We extracted the data of infants born between 2013 and 2019 from the Korean National Health Insurance Service (NHIS) database. In Korea, nearly all residents are covered by national health insurance, including citizens, foreign residents, and foreigners staying in the country for more than 6 months. Healthcare claims data, such as diagnostic codes, costs of diagnostic tests, and administered procedures, are linked to the National Health Screening Program for Infants and Children database. We obtained the following information from these databases: medical diagnosis at discharge, according to International Classification of Diseases (ICD)-10 codes
11; mortality; age at death; surgery; sex; preterm birth status; and neonatal intensive care unit (NICU) admission. Information on birth weight was obtained using ICD-10 codes or a questionnaire administered as a part of the Infant Health Screening Program. NICU admission was defined as an insurance claim code. Mortality was defined as death from any cause. Surgery was defined as any surgery insurance claim code, without considering the purpose of the surgery. Major congenital anomalies were defined as ICD-10 codes in the Q chapter or D215, D821, D1810, P350, P351, and P371, according to the EUROCAT subgroups of congenital anomalies, version 2014 (
Supplementary Table 1). EUROCAT covers around 25% of the European birth population, providing valuable epidemiological data to the world. Multiple anomalies were defined as more than one ICD-10 code for congenital gastrointestinal anomaly or abdominal wall defects for the same infant. Preterm infants and low birth weight infants were defined as ICD-10 codes P07.29, P07.39, and P07.00–19. The following neurodevelopmental outcomes of infants born between 2013 and 2017 were extracted from the database to prevent underestimation due to a short duration of follow-up: delayed development (ICD-10 code: R62.9), cerebral palsy (G80), autism spectrum disorder (F84.9), sensorineural hearing loss (H90.5), blindness (H54.0), and seizure disorders (G40 or R56.8). Birth certificate data obtained from the Korean Statistical Information Service were used to calculate the prevalence of anomalies per 10,000 live births.
12
The National Health Screening Program for Infants and Children in Korea was launched in 2007 to monitor current health issues.
13 The program provides population surveillance data, including data on medical history, physical examinations, anthropometric measurements, visual acuity screening, Korean Developmental Screening Test (K-DST) results, oral examinations, and questionnaires on anticipatory guidance. The infants had their first clinical visit at 4–6 months of age, second visit at 9–12 months, third visit at 18–24 months, fourth visit at 30–36 months, fifth visit at 42–48 months, sixth visit at 54–60 months, and seventh visit at 66–72 months. All check-ups were based on chronological age rather than corrected age. Postnatal growth was a focus among infants with weight, height, and head circumference below the 10th percentile, representing poor growth.
14 The K-DST is used to verify whether infants have achieved a normal neurodevelopmental status in six domains (gross/fine motor control, cognition, communication, social interaction, and self-control). Results were categorized into four groups based on standard deviation (SD) scores (below −2 SD = “further evaluation,” −2 and −1 SD = “follow-up test,” −1 to 1 SD = “at peer level,” and above 1 SD = “at a high level”). Short-term checkups are recommended for children in the follow-up test group. We defined developmental delays as scores indicating the requirement for further evaluation and follow-up test.
15
Statistical analysis
We used Poisson distribution to calculate 95% confidence intervals of the prevalence of major congenital gastrointestinal anomalies. Baseline infant characteristics are expressed as percentages for categorical variables. The cohort was stratified according to birth year. A χ2 test was used to compare neonatal characteristics and complications among the groups. The Cochran-Armitage trend test was used to test for linear trends. All analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA). Results with P < 0.05 were considered statistically significant.
Ethics statement
In this study, we used data from the NHIS database (NHIS-2021-4-007). The authors have no conflicts of interest associated with the NHIS. In this study, all identifiable variables, including claim-, individual-, and organizational-level identification numbers, were randomly regenerated by the NHIS to protect patient privacy. The study protocol was reviewed and approved by the Institutional Review Board of Samsung Medical Center (approval number: SMC 2020-12-059). The requirement for informed consent was waived, owing to the retrospective study design.
RESULTS
During the study period, 2,703,822 live births were recorded in Korea. Among them, 4,574 infants diagnosed with congenital anomalies of the digestive system and with abdominal wall defects had undergone surgical treatment: 4,192 of these infants were diagnosed with congenital digestive tract anomalies during the first year of life, and 404 were diagnosed with abdominal wall defects. A total of 317 infants showed multiple anomalies. The most common combination of anomalies was esophageal atresia/tracheoesophageal fistula and anorectal atresia/stenosis (n = 68), Hirschsprung’s disease and atresia/stenosis of other parts of the small intestine (n = 47), and duodenal atresia/stenosis and annular pancreas (n = 38). A total of 297 infants had two anomalies, and 20 infants had three anomalies.
Supplementary Table 2 summarizes the prevalence of major congenital anomalies of the digestive system and abdominal wall defects with surgical operation in our study cohort, along with comparison with EUROCAT data. The overall prevalences of congenital digestive tract and abdominal wall anomalies requiring surgery were 15.5 (range, 15.0–16.0) and 1.5 (1.4–1.6) per 10,000 live births, respectively. The three most prevalent anomalies for which infants underwent surgery in Korea were anorectal atresia or stenosis, Hirschsprung’s disease, and atresia or stenosis of other parts of the small intestine, whereas those in EUROCAT were anorectal atresia or stenosis, esophageal atresia with or without tracheoesophageal fistula, and diaphragmatic hernia.
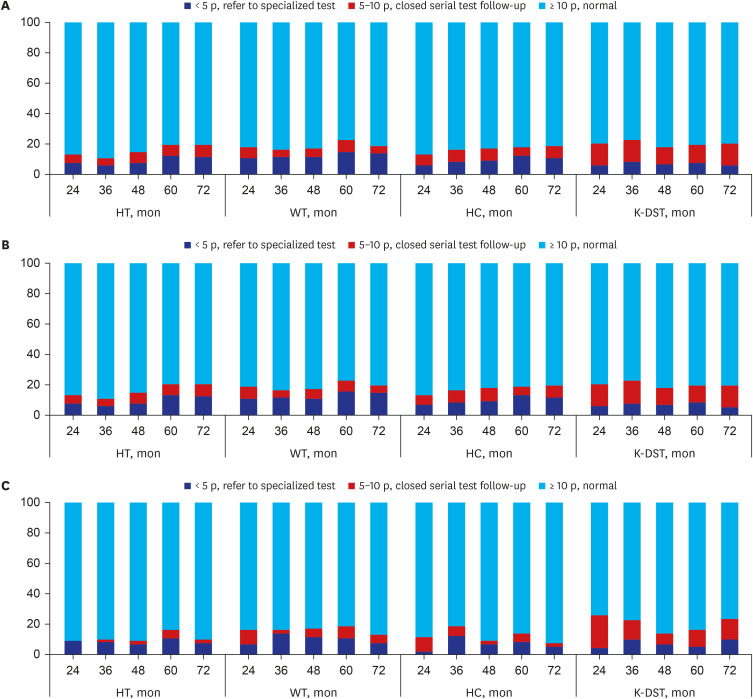
The annual prevalences of congenital anomalies of the digestive system and abdominal wall defects requiring surgy are presented in
Fig. 1. In 2019, the most common anomalies requiring surgery were anorectal anomalies, followed by Hirschsprung’s disease, esophageal atresia with or without tracheoesophageal fistula, and diaphragmatic hernia. Trend tests revealed significant changes in the prevalence of anorectal atresia and stenosis (
P = 0.013), Hirschsprung’s disease (
P = 0.003), biliary atresia (
P = 0.044), diaphragmatic hernia (
P = 0.001), and omphalocele (
P < 0.001) over the study period.
Fig. 1
The trends in the prevalence of congenital gastrointestinal anomalies with the operation (per 10,000 live births).
*P < 0.05.
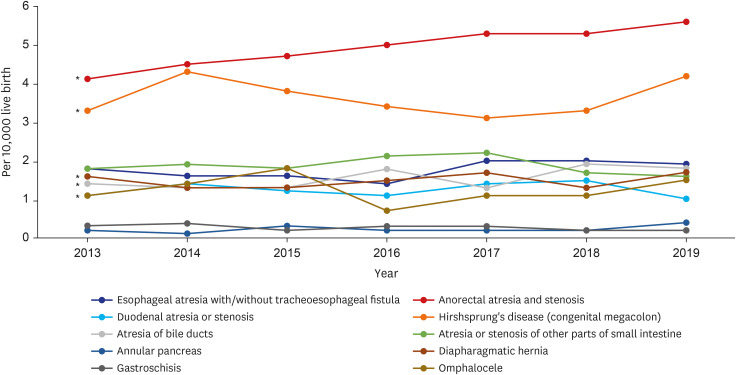
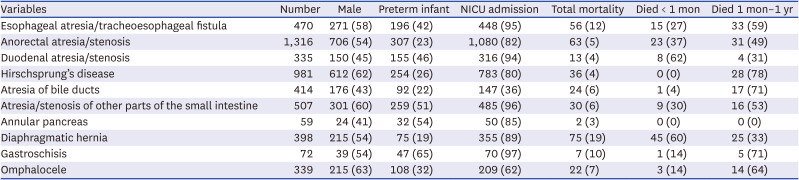
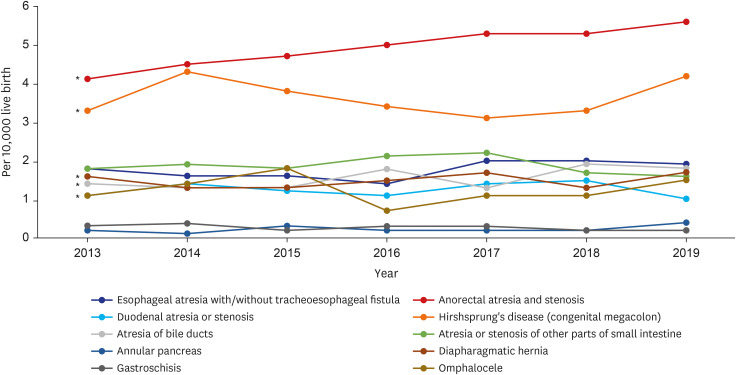
Table 1 summarizes the demographics of infants who underwent surgery for congenital anomalies of the digestive system, and abdominal wall defects. Among infants with Hirschsprung’s disease, omphalocele, atresia or stenosis of other parts of the small intestine, and esophageal atresia/tracheoesophageal fistula, the proportion of males exceeded 50%. Among infants with gastroschisis, 65.3% were born preterm. In total, 328 (6.7%) infants who underwent surgery for congenital anomalies of the digestive system and for abdominal wall defects died: 299 (6.6%) infants with congenital digestive tract anomalies requiring surgery and 29 (7.1%) infants with abdominal wall defects requiring surgery died. The most common defects requiring surgery among deceased infants were diaphragmatic hernia (18.8%), esophageal atresia (11.9%), and gastroschisis (9.7%).
Table 1
Demographics of infants diagnosed with congenital gastrointestinal anomalies with the surgery
|
Variables |
Number |
Male |
Preterm infant |
NICU admission |
Total mortality |
Died < 1 mon |
Died 1 mon–1 yr |
|
Esophageal atresia/tracheoesophageal fistula |
470 |
271 (58) |
196 (42) |
448 (95) |
56 (12) |
15 (27) |
33 (59) |
|
Anorectal atresia/stenosis |
1,316 |
706 (54) |
307 (23) |
1,080 (82) |
63 (5) |
23 (37) |
31 (49) |
|
Duodenal atresia/stenosis |
335 |
150 (45) |
155 (46) |
316 (94) |
13 (4) |
8 (62) |
4 (31) |
|
Hirschsprung’s disease |
981 |
612 (62) |
254 (26) |
783 (80) |
36 (4) |
0 (0) |
28 (78) |
|
Atresia of bile ducts |
414 |
176 (43) |
92 (22) |
147 (36) |
24 (6) |
1 (4) |
17 (71) |
|
Atresia/stenosis of other parts of the small intestine |
507 |
301 (60) |
259 (51) |
485 (96) |
30 (6) |
9 (30) |
16 (53) |
|
Annular pancreas |
59 |
24 (41) |
32 (54) |
50 (85) |
2 (3) |
0 (0) |
0 (0) |
|
Diaphragmatic hernia |
398 |
215 (54) |
75 (19) |
355 (89) |
75 (19) |
45 (60) |
25 (33) |
|
Gastroschisis |
72 |
39 (54) |
47 (65) |
70 (97) |
7 (10) |
1 (14) |
5 (71) |
|
Omphalocele |
339 |
215 (63) |
108 (32) |
209 (62) |
22 (7) |
3 (14) |
14 (64) |
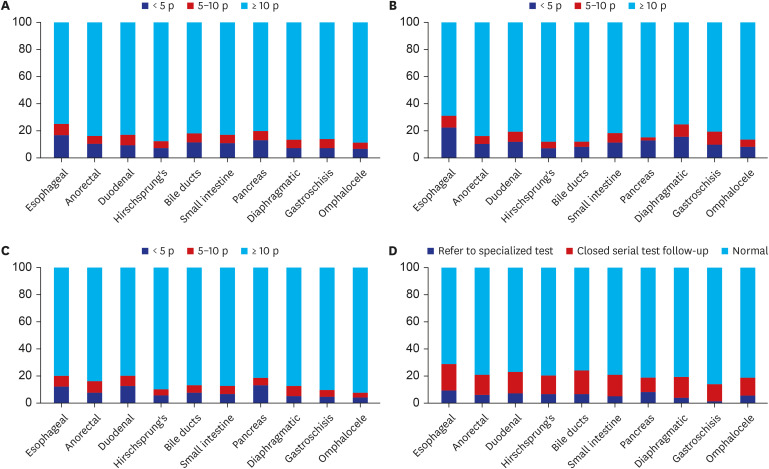
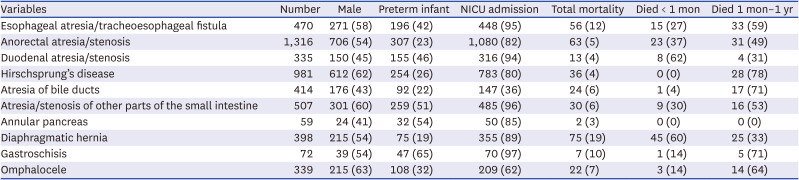
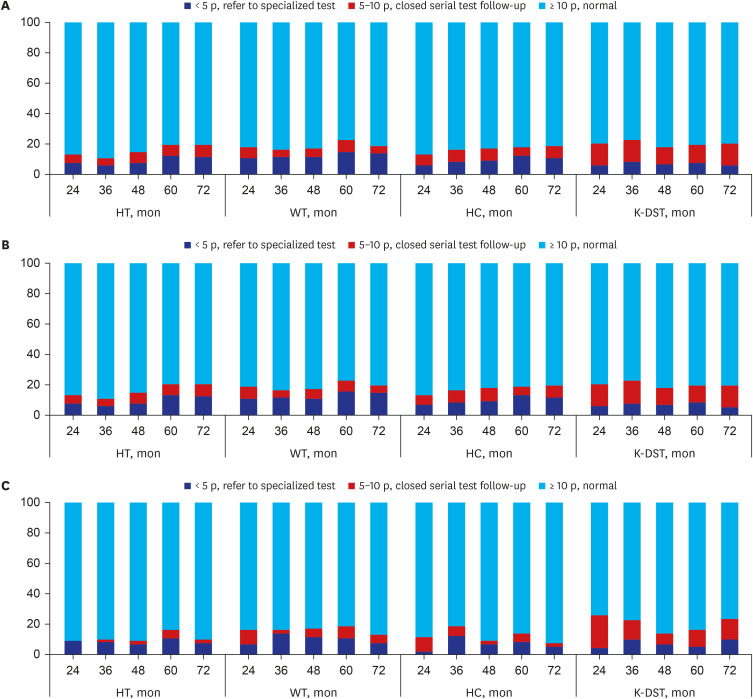
The growth outcomes at 6, 12, 24, 36, 48 60, and 72 months of age successfully extracted from 4,574 enrolled infants with congenital gastrointestinal anomalies who underwent surgery during the study period are illustrated in
Fig. 2. A total of 12,336 examinations of the National Health Screening Program for Infants and Children, including K-DST were conducted and extracted from 4,574 enrolled infants at 6, 12, 24, 36, 60, and 72 months of age. Among them, 2,065 (16.7%), 1,943 (15.8%), and 1,630 (13.2%) examinations revealed a body weight, height, and head circumference below the 10th percentile, respectively. These parameters varied greatly according to the recorded congenital anomaly: body weight, 11.8–30.9%; height, 11.5–25.4%; and head circumference, 8.0–20.5%. Values for these parameters below the 10th percentile were most common among infants with esophageal atresia with or without tracheoesophageal fistula. Patients with Hirschsprung’s disease had the lowest prevalence of poor growth in terms of height (12.6%), body weight (11.8%), and head circumference (10.6%). In total, 774 of 12,336 exam results (7.9%) in the K-DST were assigned for “further evaluation,” and 1,479 out of 12,336 (15.1%) were assigned for “follow-up test.” The proportion of infants designated for further evaluation (2.7–11.9%) and follow-up tests (10.9–18.6%) varied significantly according to the type of anomaly. Infants with esophageal atresia with or without tracheoesophageal fistula had the highest prevalence of both categories for poor developmental outcomes, whereas those with gastroschisis had the lowest prevalence requiring further evaluation (
Fig. 2D).
Fig. 2
Growth and developmental screening outcome of infants diagnosed with congenital gastrointestinal anomalies with operation examined at 6, 12, 36, 48, 60, and 72 months between 2013 and 2019. (A) Height. (B) Weight. (C) Head circumference. (D) Korean Developmental Screening Test.
Esophageal = esophageal atresia with/without tracheoesophageal fistula, Anorectal = anorectal atresia, and stenosis, Duodenal = duodenal atresia or stenosis, Hirschsprung’s = Hirschsprung’s disease, Bile ducts = atresia of bile ducts, Small intestine = atresia or stenosis of other parts of the small intestine, Pancreas = annular pancreas, Diaphragmatic = diaphragmatic hernia.
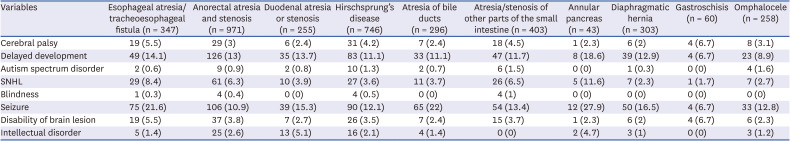
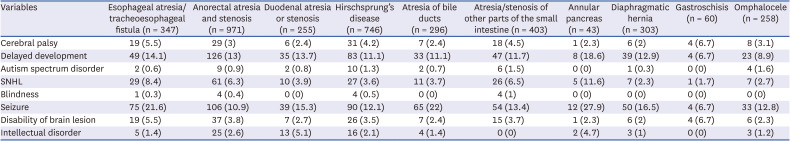
The developmental outcomes of patients born between 2013 and 2017 who had congenital anomalies in the digestive system and had abdominal wall defects requiring surgery are summarized in
Table 2. Cerebral palsy, delayed development, and seizures were observed in 130 out of 4,574 infants (2.8%; range, 2.0–6.7%), 490 infants (10.7%; range, 6.7–18.6%), and 555 infants (12.1%; range, 6.7–27.9%), respectively. The prevalence of cerebral palsy was highest among infants with esophageal atresia with or without tracheoesophageal fistula. Among 303 infants diagnosed with diaphragmatic hernia, 43 (14.2%) were treated with extracorporeal membrane oxygenation (ECMO). Infants receiving ECMO had a higher mortality rate than those who did not (63% vs. 13%,
P < 0.001), although the incidences of delayed development were comparable (16% vs. 12%).
Table 2
Developmental outcome of infants diagnosed with congenital gastrointestinal anomalies with the operation, born between 2013 and 2017
|
Variables |
Esophageal atresia/tracheoesophageal fistula (n = 347) |
Anorectal atresia and stenosis (n = 971) |
Duodenal atresia or stenosis (n = 255) |
Hirschsprung’s disease (n = 746) |
Atresia of bile ducts (n = 296) |
Atresia/stenosis of other parts of the small intestine (n = 403) |
Annular pancreas (n = 43) |
Diaphragmatic hernia (n = 303) |
Gastroschisis (n = 60) |
Omphalocele (n = 258) |
|
Cerebral palsy |
19 (5.5) |
29 (3) |
6 (2.4) |
31 (4.2) |
7 (2.4) |
18 (4.5) |
1 (2.3) |
6 (2) |
4 (6.7) |
8 (3.1) |
|
Delayed development |
49 (14.1) |
126 (13) |
35 (13.7) |
83 (11.1) |
33 (11.1) |
47 (11.7) |
8 (18.6) |
39 (12.9) |
4 (6.7) |
23 (8.9) |
|
Autism spectrum disorder |
2 (0.6) |
9 (0.9) |
2 (0.8) |
10 (1.3) |
2 (0.7) |
6 (1.5) |
0 (0) |
1 (0.3) |
0 (0) |
4 (1.6) |
|
SNHL |
29 (8.4) |
61 (6.3) |
10 (3.9) |
27 (3.6) |
11 (3.7) |
26 (6.5) |
5 (11.6) |
7 (2.3) |
1 (1.7) |
7 (2.7) |
|
Blindness |
1 (0.3) |
4 (0.4) |
0 (0) |
4 (0.5) |
0 (0) |
4 (1) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
|
Seizure |
75 (21.6) |
106 (10.9) |
39 (15.3) |
90 (12.1) |
65 (22) |
54 (13.4) |
12 (27.9) |
50 (16.5) |
4 (6.7) |
33 (12.8) |
|
Disability of brain lesion |
19 (5.5) |
37 (3.8) |
7 (2.7) |
26 (3.5) |
7 (2.4) |
15 (3.7) |
1 (2.3) |
6 (2) |
4 (6.7) |
6 (2.3) |
|
Intellectual disorder |
5 (1.4) |
25 (2.6) |
13 (5.1) |
16 (2.1) |
4 (1.4) |
0 (0) |
2 (4.7) |
3 (1) |
0 (0) |
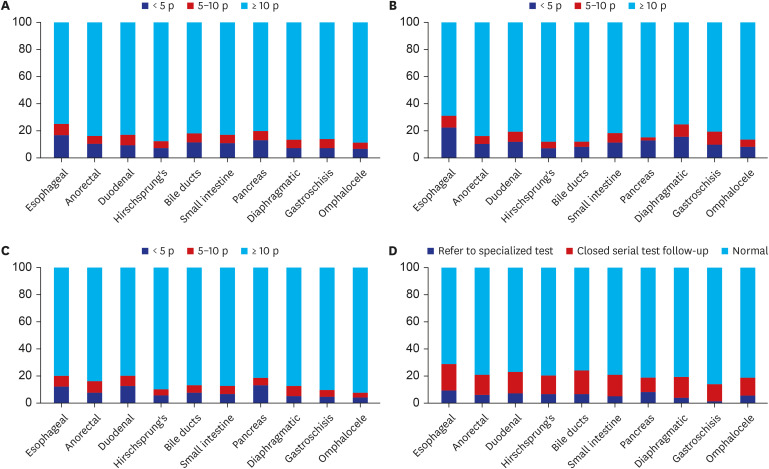
3 (1.2) |
Fig. 3 displays the serial observations of growth and developmental outcomes of infants born in 2013 who underwent surgery for congenital anomalies of the digestive system and abdominal wall defects (n = 685). Among infants with congenital anomalies of the digestive system and abdominal wall defects requiring surgery, 60 (13.5%) and 78 (20.0%) infants had a height below the 10th percentile at 24 and 72 months, respectively, representing a percentage increase of 6.5% over the 3-year period. A total of 56 (13.8%) and 74 (21.0%) infants had congenital anomalies of the digestive system, while 4 (9.5%) and 4 (10.5%) infants had abdominal wall defects at 24 and 72 months, respectively.
Fig. 3
Growth and developmental outcome of infants between 24 and 72 months, who were born in 2013 and diagnosed congenital gastrointestinal anomalies with an operation (A), congenital digestive anomalies with an operation (B), congenital abdominal wall defects with an operation (C).
HT = height, WT = weight, HC = head circumference, K-DST = Korean Developmental Screening Test.
Overall, at 24 and 72 months, respectively, 85 (19.1%) and 77 (19.7%) infants had body weight below the 10th percentile, respectively. Among them, 78 (19.3%) and 72 (20.4%) infants had congenital anomalies of the digestive system, while 7 (16.7%) and 5 (12.8%) infants had abdominal wall defects, showing a decrease of 3.9% over time.
At 24 and 72 months, respectively, 61 (13.7%) and 74 (19.0%) infants had head circumference below the 10th percentile, representing an increase of 5.3%. Among them, 56 (13.8%) and 71 (20.1%) infants had congenital gastrointestinal anomalies, respectively, indicating an increase of 6.3%, while 5 (11.9%) and 3 (8.1%) infants had digestive tract anomalies, showing a decrease of 3.8%.
Overall, at 24 and 72 months, developmental delay was observed in 93 (20.9%) and 81 (20.8%) infants, respectively. Among those with digestive tract anomalies, 83 (20.5%) and 72 (20.4%) infants experienced developmental delay at 24 and 72 months, respectively. Similarly, among those with abdominal wall defects, 11 (26.2%) and 9 (23.7%) infants displayed developmental delay at 24 and 72 months, respectively.
DISCUSSION
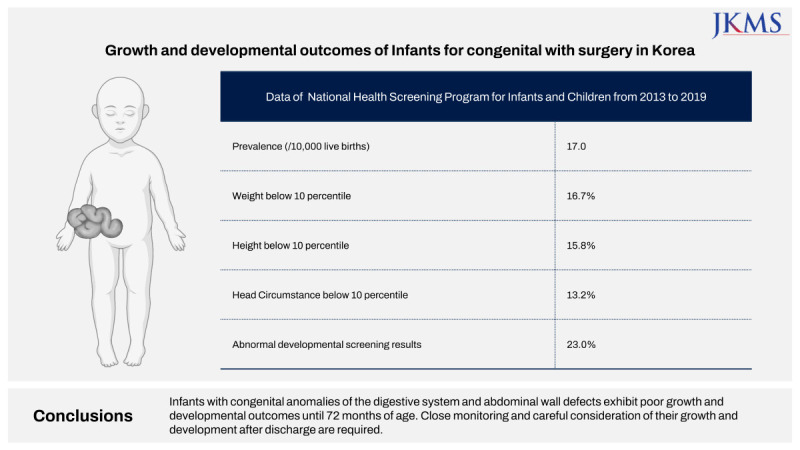
The present study demonstrated that the annual incidence of newborn infants who had digestive system anomalies and abdominal wall defects requiring surgery in Korea was approximately 15.5 and 1.5 per 10,000 live births, respectively, which are comparable to incidences for EUROCAT. Additionally, we discovered that 6.7% died, 16.7% had poor weight growth, and 23% had developmental delay, which was investigated from follow-up examinations until 72 months of age.
This population-based nationwide study provides comprehensive information on the growth and developmental outcomes of infants with congenital anomalies of the digestive system and with abdominal wall defects who underwent surgery in Korea. Understanding the growth and developmental outcomes of infants with congenital gastrointestinal anomalies helps healthcare providers identify risk factors, evaluate treatment approaches, and develop evidence-based guidelines for management. Furthermore, early detection and access to the necessary support services for infants with congenital anomalies can lead to improved outcomes and enhanced quality of life for affected infants and their families.
The EUROCAT is a European network of population-based registries for the epidemiological surveillance of congenital anomalies, for the identification of teratogenic exposure, and for the assessment of the impact of primary prevention and prenatal screening policies and practices. By collecting data from registries in 21 European countries, EUROCAT covers around 25% of the European birth population, providing valuable epidemiological data to the world.
8 Therefore, comparing EUROCAT data with data from Korea can enhance our understanding of congenital anomalies on a global scale and help identify areas for further research and intervention. The prevalences (per 10,000 live births) of congenital anomalies of the digestive system and abdominal wall defects (15.5 and 1.5) in Korea appear to be consistent with the EUROCAT database (16.10 and 3.35, respectively). The most prevalent anomalies were anorectal atresia and/or stenosis in both EUROCAT (2.8) and this study (4.9), followed by esophageal atresia with/without tracheoesophageal fistula (2.5) in EUROCAT and Hirschsprung’s disease (3.6) in this study.
8 In a study of the US, 57% of infants with a congenital gastrointestinal malformation were boys (odds ratio, 1.8), and 27% were preterm infants.
16 In this study, the prevalence of Hirschsprung’s disease, omphalocele, atresia or stenosis of other parts of the small intestine, and esophageal atresia/tracheoesophageal fistula were higher among boys than among girls. The majority of infants with gastroschisis (65.3%), annular pancreas (54.0%), and atresia/stenosis of other parts of the small intestine (51.1%) were preterm infants.
The chance of dying from a congenital gastrointestinal anomaly if born in a low-income country is 2 in 5, compared to 1 in 5 in a middle-income country and 1 in 20 in a high-income country.
17 According to a 2016 Australian report on congenital anomalies, 5.0% of infants with congenital gastrointestinal anomalies died after birth.
18 In this study, 6.6% with anomalies of the digestive system and 7.1% with abdominal wall anomalies died after birth, compatible with high-income countries. Gastroschisis-related mortality rates differ the most between country income strata (90% in low-income countries, 32% in middle-income countries, and 1.4% in high-income countries).
19 In this study, the gastroschisis-related mortality rate was 10%, which is relatively higher than that for high-income countries.
Infants with congenital gastrointestinal anomalies may fail to thrive. A single-site study of neonates with congenital gastrointestinal defects revealed weight and height growth delays until 22 months of age, but not thereafter.
20 The growth of head circumference was delayed only until 15 months. However, in our study, growth below the 10th percentile increased by 6.5% for height, 4.1% for weight, and 8.6% for head circumference from 24 to 72 months. Therefore, specialized medical and nutritional management should be needed until 72 months. According to a previous report, 67% of infants with congenital diaphragmatic hernia exhibit growth failure, and 58% of infants with esophageal atresia exhibit weight loss after surgery.
21 In this study, a birth weight below the 10th percentile was most prevalent among infants with esophageal atresia with/without tracheoesophageal fistula (25.4%), followed by those with diaphragmatic hernia (13.7%). Taken together, our study outcomes suggest that healthcare providers should closely monitor the growth and nutritional status of infants with congenital gastrointestinal anomalies because early intervention can help prevent or mitigate the effects of failure to thrive.
Patients with congenital gastrointestinal malformations exhibit impaired neurodevelopmental outcomes until adolescence. Cognitive impairment among such patients is reportedly mild, whereas motor and language impairment are more pronounced.
22 In this study, the prevalence of delayed development was higher than that of cerebral palsy among such infants. Children with congenital diaphragmatic hernia had a higher risk of neurodevelopmental delays than healthy controls, and 31% of infants with gastroschisis had a high risk of developmental delay, with 34% experiencing delays by 2 years of age. Infants with short bowel syndrome had a significantly poorer overall neurodevelopmental outcome than infants with other gastrointestinal abnormalities.
23
Collectively, patients with gastrointestinal anomalies and abdominal wall defects who were investigated in this study exhibited higher mortality rates and long-term growth and developmental delays, compared to the general population. According to Yoon et al.’s report,
24 for late preterm infants born at 32 to 36 weeks gestation and for full-term infants born at 37 to 41 weeks gestation, the survival rate until 1 year of age is approximately 99.9%. Moreover, in long-term follow-up at 24 and 72 months, cases showing growth delays with head circumference and weight below the 10th percentile, as well as developmental delays based on the K-DST, accounted for around 10% of the cohort. In contrast, the patients in our study demonstrate relatively higher rates of mortality and growth and developmental delay: 31% of infants with atresia/stenosis of the small intestine, 20% of infants with congenital diaphragmatic hernia, and 14% of infants with gastroschisis had poor developmental screening results.
The main strength of the present study is its substantial statistical power for analysis of trends because it was conducted using nationally representative data spanning 7 years from the NHIS in Korea, which covers almost the entire population of Korea. Furthermore, the National Health Screening Program for Infants and Children in Korea is a government-run program that provides regular health screening for about 70–80% of infants and children up to the age of 6 years, regardless of their family income or social status. This nationwide, comprehensive analysis of congenital gastrointestinal anomalies in Korea may serve as a reference guide for clinicians and other health professionals for counseling and public health planning. Furthermore, we reported not only short-term outcomes, such as mortality, but also long-term growth and developmental outcomes. This study provides evidence indicating that infants with congenital gastrointestinal anomalies should be monitored for growth and developmental delays until they are 6 years of age.
However, this study also has several limitations. This was a retrospective review of entries from an anonymized NHIS database. The national claims database does not include individual patient medical information. Hence, we obtained the medical diagnosis at discharge according to the ICD-10 code input by the hospital. Incorrect diagnoses or rule-out diagnoses could be included for the purpose of insurance claims. Additionally, some diagnoses could be missed because they are not required for insurance claims. Next, regarding surgeries for congenital anomalies, we could only confirm that the patient had undergone surgery, not the details of the operation. There may be differences in the frequency and order of the most common pediatric surgeries between other studies using specific surgical codes and the present study.
25 Also, possible over-diagnosis or under-diagnosis may still exist in this study. Individual feeding and nutritional information were also not reviewed. As the K-DST is a developmental screening tool that depends on a questionnaire completed by parents, its use may have introduced recall bias. We did not use the Bayley Scale of Early Childhood Development as a diagnostic tool. As we investigated only congenital anomalies of the digestive system and abdominal wall defects, we could not determine whether infants had genetic disorders or other syndromes affecting their development. The association of outborn delivery with mortality and morbidity was not evaluated. Newborn data were not linked to maternal data, and maternal information was not included. Finally, the growth and development of preterm infants and term infants were not separately investigated, and specific corrections for the growth or development of premature infants compared with a control group were not considered. These aspects should be considered when future research studies are designed.
In conclusion, infants with congenital anomalies of the digestive system and abdominal wall defects exhibit poor growth and developmental outcomes until 72 months of age. To improve long-term prognosis, it is important to focus on appropriate medical and nutritional management, regular monitoring, and early intervention. Furthermore, it is necessary to establish a more systematic follow-up system.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download