INTRODUCTION
MATERIALS AND METHODS
Search strategy
Eligibility criteria
• Population (P): extracted teeth in animal models;
• Intervention (I): photobiomodulation treatment of the root surface prior to replantation;
• Comparison (C): control group;
• Outcome (O): root resorption;
• Study design (S): studies in animal models.
Selection of the studies
Data extraction
Qualitative assessment
Certainty of evidence
RESULTS
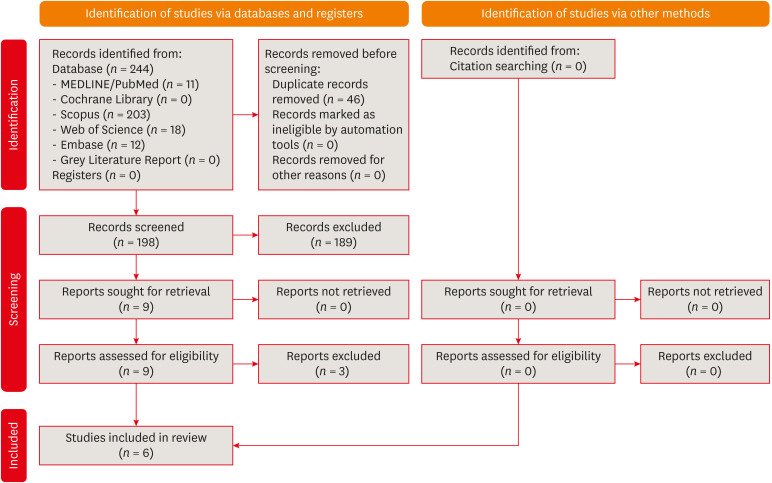
Study selection
Figure 1
Systematic search process according to the PRISMA flow diagram.
Data extraction
Table 1
Characteristics of the included studies

| Authors – country | Year of publication | Animal model (sample size) | Investigated groups (samples per group) | Teeth evaluated | Photobiomodulation protocol | Additional procedures | Extra-alveolar time prior to replantation | Storage medium | Time of outcome assessment | Method of root resorption analysis | Outcomes | Main findings |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Saito et al. [33] – Brazil | 2011 | Male rats (n = 60) | • Group 1: Control 1 (n = 10) | Maxillary right incisors | Palatal root surface/Alevolar socket | • Groups 1 and 4: Asepsis with 1% iodine polyvinylpyrrolidone, and irrigation of the alveolar socket with saline solution | • Group 1: Control 1–4 min | • Groups 1 and 4: kept dry | After 60 days | • Histomorphometric analysis | • No differences were found in inflammatory and replacement resorption among groups. | • Treatment of the root surface and the alveolar wound with low-level laser did not improve the healing process of immediate and delayed tooth replantation in rats. |
| • Group 2: Control 2 (n = 10) | GaAlAs continuous-wave diode laser | • Groups 2, 3, 5, and 6: Removal of the dental papilla and enamel organ with scalpel, pulp extirpation, root canal irrigation with saline solution, root canal filling with calcium hydroxide | • Group 2: Control 2–30 min | • Groups 2, 3, 5, and 6: saline solution | • Areas of ankylosis were greater in group 5. | |||||||
| • Group 3: Control 3 (n = 10) | • Wavelength: 660 nm (palatal root surface), 830 nm (alveolar socket) | • Asepsis with 1% iodine polyvinylpyrrolidone, and irrigation of the alveolar socket with saline solution (after laser application in groups 5 and 6) | • Group 3: Control 3–45 min | |||||||||
| • Group 4: Laser 1 (n = 10) | • Output power: 30 mW (palatal root surface), 40 mW (alveolar socket) | • Group 4: Laser 1–4 min | ||||||||||
| • Group 5: Laser 2 (n = 10) | • Energy density: 57.14 J/cm-2 (each site) | • Group 5: Laser 2–30 min | ||||||||||
| • Group 6: Laser 3 (n = 10) | • Total energy: 4 J (each site) | • Group 6: Laser 3–45 min | ||||||||||
| • Total time of irradiation: 2 min and 13 sec (palatal root surface), 1 min and 40 sec (alveolar socket) | ||||||||||||
| Carvalho et al. [34] – Brazil | 2012 | Male rats (n = 60) | • Group 1: Negative control (n = 10) | Maxillary right incisors | Root surface | • Removal of the dental papilla, pulp extirpation, root canal preparation and irrigation with 1% sodium hypochlorite and EDTA-T | • 60 min | • Kept dry | After 15, 30, and 60 days | • Radiographic analysis | • Histomorphometric and radiographic analyses showed lower incidence of root resorption in the irradiated groups, without differences between irradiated groups. | • Root surface treatments with high-powered diode laser irradiation prior to delayed replantation reduced the occurrence of external root resorption. |
| • Group 2: Positive control (n = 10) | GaAlAs high-power diode laser | • Root canal filling with calcium hydroxide (after laser application in groups 3 and 4) | • Histomorphometric analysis | • Resorption and ankylosis were observed in histological section after 30 and 60 days, except in group 3. | ||||||||
| • Group 3: Continuous mode laser (n = 10) | • Wavelength: 810 nm | • Prior to laser application, immersion of extracted teeth in 1% sodium hypochlorite for 10 min, removal of remaining periodontal ligament with gauze, and washing with saline solution | • Histological analysis | |||||||||
| • Group 4: Pulse mode laser (n = 10) | • Output power: 1,200 mW | |||||||||||
| • Total time of irradiation: 30 sec (5 sec in each surface) | ||||||||||||
| • Incidence angulation: 45° | ||||||||||||
| Vilela et al. [35] – Brazil | 2012 | Male rats (n = 72) | • Group 1: Control (n = 36) | Maxillary left incisor | Root surface/Alevolar socket | • None | • Not reported | • Kept dry for 15 min and then stored in saline solution | After 15, 30 and 60 days | • Histomorphological analysis | • Increased root resorption in the control group was observed in all periods evaluated when compared to the laser group. | • Laser therapy resulted in less occurrence of root resorption. |
| • Group 2: Laser (n = 36) | InGaAlP continuous-wave diode laser | |||||||||||
| • Wavelength: 685 nm (each site) | ||||||||||||
| • Output power: 50 mW (each site) | ||||||||||||
| • Spot size: 0.02 cm2 | ||||||||||||
| • Optical power density: 2.5 W/cm2 (each site) | ||||||||||||
| • Energy density: 200 J/cm2 (each site) | ||||||||||||
| • Total energy: 4 J (each site) | ||||||||||||
| • Distance from root/irradiated tissue: 1 mm | ||||||||||||
| Carvalho et al. [36] – Brazil | 2016 | Male rats (n = 60) | • Group 1: Control 1 (n = 15) | Maxillary right incisors | Root surface/Alevolar socket/Buccal and palatal mucosa | • Removal of the dental papilla and enamel organ with scalpel, pulp extirpation, root canal irrigation with saline solution, root canal filling with calcium hydroxide | • 40 min | • Group 1: kept dry | After 15, 30 and 60 days | • Histological analysis | • After 15 days, group 4 exhibited moderate external inflammatory resorption. | • Laser application to the root surface and alveolar socket resulted in no external inflammatory root resorption or ankylosis. |
| • Group 2: Control 2 (n = 15) | Laser application in buccal and palatal mucosa only in group 4, every 48 hr for 15 days | • Prior to replantation, irrigation of the alveolar socket with saline solution | • Groups 2, 3, and 4: UHT skimmed milk | • After 30 days, groups 1, 2, and 4 presented intense external inflammatory root resorption, and different levels of ankylosis. | • Association of laser application in buccal and palatal mucosa every 48 hours for 15 days resulted in a higher incidence of external inflammatory root resorption and ankylosis. | |||||||
| • Group 3: Laser (n = 15) | GaAlAs continuous-wave diode laser | • Group 3 remained without external inflammatory root resorption and ankylosis up to 60 days. | ||||||||||
| • Group 4: Laser for 15 days (n = 15) | • Wavelength: 780 nm (each site) | |||||||||||
| • Output power: 70 mW (each site) | ||||||||||||
| • Spot size: 0.04 cm2 | ||||||||||||
| • Energy density: 16.8 J/cm2 (root surface), 4.2 J/cm2 (alveolar socket), 4.2 J/cm2 (buccal and palatal mucosa) | ||||||||||||
| • Total time of irradiation: 320 sec (root surface), 60 sec (alveolar socket), 120 sec (buccal and palatal mucosa) | ||||||||||||
| Matos et al. [37] – Brazil | 2016 | Male rats (n = 60) | • Group 1: Control 1 (n = 10) | Maxillary right incisors | Root surface/Alevolar socket/Buccal and palatal mucosa | • Removal of the dental papilla with a scalpel, pulp extirpation, root canal irrigation with saline solution, root canal filling with calcium hydroxide | 45 min | • Groups 1 and 4: kept dry | After 15 and 30 days | • Histomorphometric analysis | • After 30 days, group 1 presented larger areas of root resorption. | • Laser application, as well as cow and soy milk, reduced the occurrence of root resorption |
| • Group 2: Control 2 (n = 10) | Laser application in buccal and palatal mucosa, every 48 hr for 5 sessions | • Prior to replantation, irrigation of the alveolar socket with saline solution | • Groups 2 and 5: UHT cow milk | • After 30 days, groups 2 and 3 presented no difference in root resorption. | ||||||||
| • Group 3: Control 3 (n = 10) | GaAlAs continuous-wave diode laser (root surface and alveolar socket) | • Groups 3 and 6: soy milk | • After 30 days, laser application significantly reduced root resorption in group 4. | |||||||||
| • Group 4: Laser 1 (n = 10) | InGaAlP continuous-wave diode laser (buccal and palatal mucosa) | • After 30 days, laser application reduced root resorption in groups 5 and 6, without differences when compared to groups 2 and 3. | ||||||||||
| • Group 5: Laser 2 (n = 10) | • Wavelength: 808nm (root surface and alveolar socket), 660 nm (buccal and palatal mucosa) | |||||||||||
| • Group 6: Laser 3 (n = 10) | • Output power: 100 mW (each site) | |||||||||||
| • Optical power density: 3.6 W/cm2 (each site) | ||||||||||||
| • Energy density: 61 J/cm−2 (each site) | ||||||||||||
| • Total energy: 10.2 J (root surface and alveolar socket), 17 J (buccal and palatal mucosa) | ||||||||||||
| • Total time of irradiation: 102 sec (root surface), 17 sec (alveolar socket), 170 sec (buccal and palatal mucosa) | ||||||||||||
| Carvalho et al. [38] – Brazil | 2017 | Male rats (n = 50) | • Group 1: Negative control (n = 10) | Maxillary right incisors | Root surface | Removal of dental papilla with scalpel in all groups | • Group 2: immediate replantation | • Kept dry | After 60 days | • Radiographic analysis | • Radiographic analysis showed fewer resorptive areas in group 5 than in the negative control. | • Laser application, with or without application of fibroblast growth gel, reduced the occurrence of external root resorption and ankylosis. |
| • Group 2: Positive control (n = 10) | Continuous-wave high-power diode laser | • Groups 3 and 5: Application of 50 μg of 0.2% basic fibroblast growth gel in 3% hydroxypropylmethylcellulose gel in the palatal root surface and in the alveolar socket | • Groups 1, 3, 4, and 5: 60 min | • Histological analysis | • Radiographically, groups 3, 4, 5, and the positive control did not differ regarding areas of external root resorption. | |||||||
| • Group 3: Fibroblast growth gel (n = 10) | • Wavelength: 808 ± 10 nm | • Groups 3, 4, and 5: Pulp extirpation, root canal preparation and irrigation with 1% sodium hypochlorite and EDTA-T, and root canal filling with calcium hydroxide | • Histological analysis showed lower mean values of ankylosis, replacement, and inflammatory resorption for group 4 than in the negative control, without differing from positive control. | |||||||||
| • Group 4: Laser (n = 10) | • Output power: 1,200 mW | • Prior to laser application, immersion of extracted teeth in 1% sodium hypochlorite for 10 min, removal of remaining periodontal ligament with gauze, and washing with saline solution | ||||||||||
| • Group 5: Laser + Fibroblast growth gel (n = 10) | • Optical power density: 7.14 W/cm2 | • Prior to replantation, irrigation of the alveolar socket with saline solution | ||||||||||
| • Energy density: 214.3 J/cm2 | ||||||||||||
| • Total energy: 45 J | ||||||||||||
| • Incidence angulation: 45° | ||||||||||||
| • Total time of irradiation: 30 sec (5 sec on each surface) |
Qualitative assessment
Figure 2
Quality assessment of the included studies according to the risk of bias tool for preclinical animal studies – (SYRCLE’s RoB tool).

Certainty of evidence
Table 2
Certainty of the evidence from the included studies according to the GRADE approach for preclinical animal studies

| Number of studies | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Overall certainty of evidence |
|---|---|---|---|---|---|---|
| 6 studies | Very serious* | Not serious | Not serious | Not serious | None | ⨁⨁◯◯ |
| LOW |




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download