RESULTS
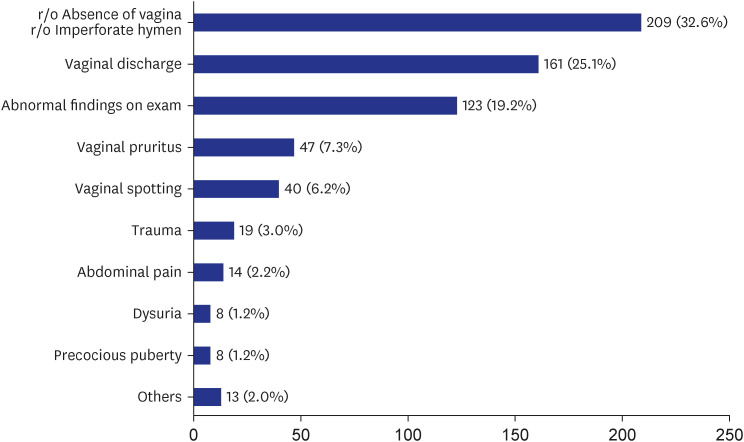
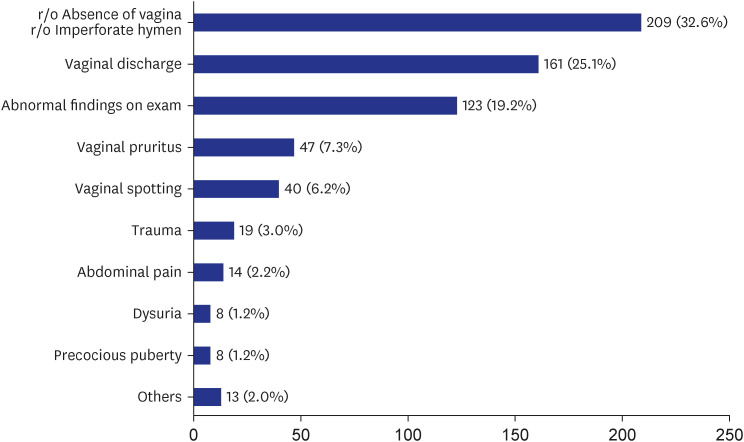
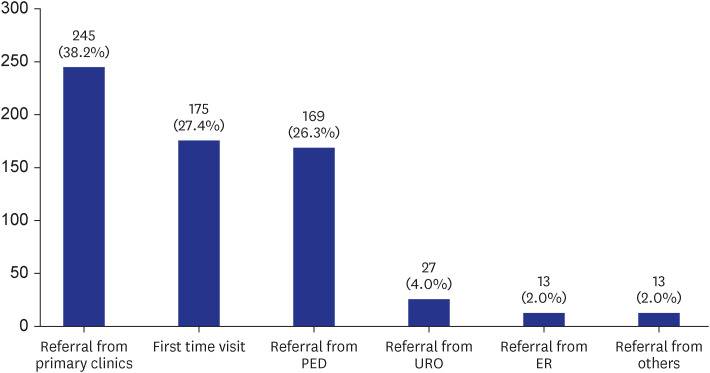
The chief complaints about the gynecologic problems varied among pediatric patients in this study (
Fig. 1). The most frequent chief complaint was abnormal external genitalia, with absence of the vagina or imperforate hymen as the main concerns at presentation (n = 209, 32.6% of the study population). The second most encountered group of problems was infectious and inflammatory conditions of the vulva and vaginal area, with the primary symptom of increased vaginal discharge (n = 161, 25.1%). Other chief complaints in the clinic included abnormal findings on examinations requiring the further evaluation by gynecologic specialists, vaginal pruritus and spotting, trauma, and other incidental findings.
Fig. 1
Chief complaints of pediatric patients who visited the pediatric and adolescent gynecologic clinic.
Among those who visited with concerns about genital abnormalities, the most frequently diagnosed disease entity was agglutination of the labia minora (n = 198). Vulvovaginitis was the second most common disease (n = 169), followed by problems regarding neoplasm, vaginal bleeding, and other miscellaneous reasons.
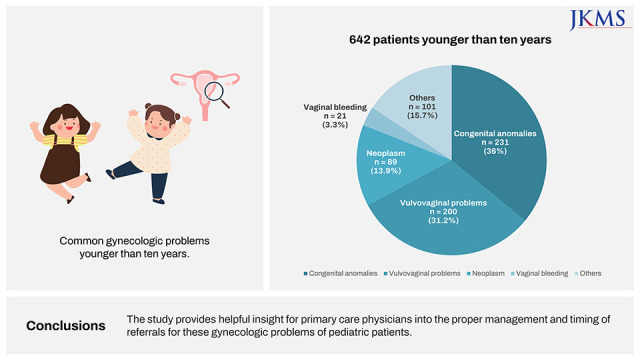
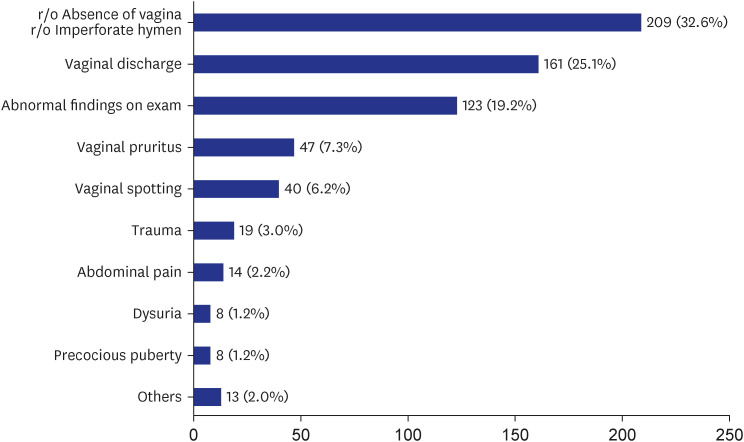
Gynecologic diseases in pediatric patients can be categorized into these groups: 1) congenital anomalies, which mainly involve an abnormal appearance; 2) vulvovaginal problems, including inflammatory or infectious conditions; 3) neoplasm; 4) vaginal bleeding; and 5) other miscellaneous conditions (
Fig. 2).
Fig. 2
Numbers of patients by disease category.
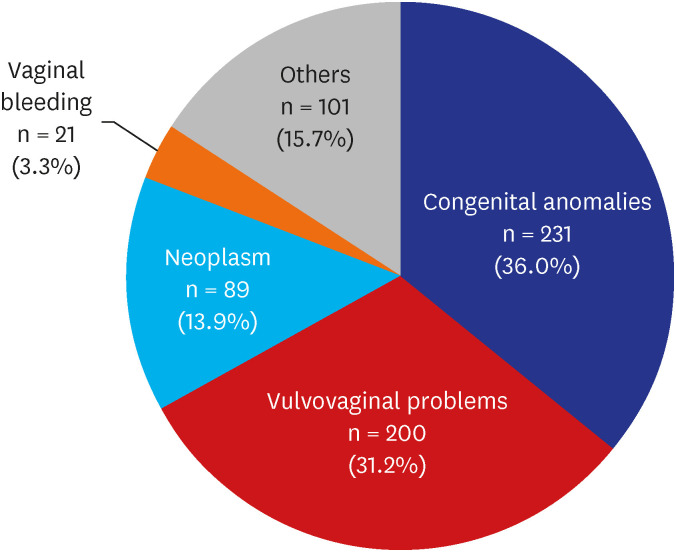
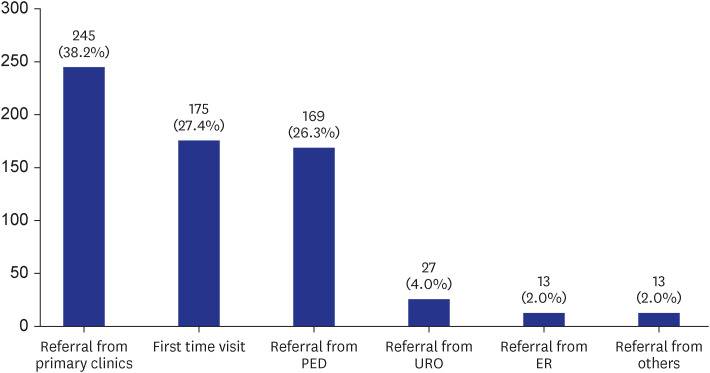
Among the 642 patients who visited the clinic during the study period, 245 cases (38.2%) were referrals from primary care sources; 175 cases (27.4%) were direct outpatient clinic visits; 169 cases (26.3%) were referrals from the pediatric department; and the remainder were referrals from other departments, including emergency medicine, urology, and general surgery (
Fig. 3).
Fig. 3
Categorization of referrals to the pediatric and adolescent gynecologic clinic.
PED = pediatric emergency department, URO = urology, ER = emergency room.
Congenital anomalies: problems with the genital tract
In total, 231 patients (36.0%,
Fig. 2) were referred to the clinic with suspected genital abnormalities. The finding was frequently noted during routine well-baby exams or health check-ups, and 100 (43.3%) patients were referred via a primary pediatric clinic. Of the patients who were diagnosed with congenital anomalies, 198 cases (85.7%) were diagnosed with agglutination of the labia minora. Apparent absence of the vagina and/or imperforate hymen was the most frequent chief complaint among all visits. Other referrals involved symptoms such as urinary discomfort, genital asymmetry, and vaginal pruritus. Patients who presented to the clinic with agglutination of the labia minora complained mostly of an abnormal genital appearance, sometimes accompanied by symptoms such as dysuria. All patients who visited our center with this diagnosis were treated conservatively with topical estrogen to ease their symptoms and were successfully cured. However, surgical separation may be considered for patients who do not respond to conservative treatment.
Vulvovaginal problems
Vulvovaginal inflammatory problems were the second most common disease entity reported in visits to the clinic (n = 200, 31.2%,
Fig. 2). The symptoms in these patients were increased vaginal discharge (n = 142), vaginal pruritus (n = 29), and blood-tinged discharge (n = 13), among others. Patients with poor anal hygiene complained about pruritic symptoms caused by constant irritation. Two patients who experienced recurrent vulvovaginitis and vaginal spotting were diagnosed with a foreign body within the vaginal cavity, which caused continuous irritation of vaginal wall. Foreign bodies were removed under general anesthesia. Other rare conditions included post-traumatic inflammation, vulvar abscess, and parasitic infection. One hundred and seven patients (73.5%) were treated with empiric antibiotics. For patients with suspected vulvovaginitis, gram stain culture of the genital tract was conducted. Of 140 cases that underwent gram stain culture, 118 cases (84.3%) resulted in gram-positive and -negative organisms including normal flora,
Staphylococcus,
Haemophilus, and
Escherichia coli.
Neoplasm
Most adnexal neoplasms were found in imaging studies based on patient symptoms of abdominal pain or distension. Eighty-nine patients (13.9%) presented with problems related to neoplasm requiring further evaluation of incidental findings. An ovarian mass was found in 67 patients, and the diagnosis was confirmed histologically in 27 cases. Mature cystic teratoma (n = 17, 63%) was the most common ovarian mass. Diagnostic modalities for neoplasms at other sites included hysteroscopy, diagnostic vaginoscopy, and excisional biopsy. The pathological diagnoses varied from benign to malignant and included mature cystic teratoma, immature teratoma, juvenile granulosa cell tumor, neuroblastoma, serous cystadenoma, mucinous cystadenoma, mixed germ cell tumor and yolk sac tumor. Other benign conditions without symptoms, including periurethral cyst, vaginal polyp, and vulvar mass, were monitored without further treatment. All patients were followed closely, and most cases of suspected benign cysts, such as physiologic and functional cysts, regressed spontaneously.
Vaginal bleeding
Problems with vaginal bleeding and accompanying symptoms were identified in 21 cases (3.3%) and constituted the least common reason for referral to our center. Patients suspected of precocious puberty (n = 17) were evaluated in consultation with pediatric endocrinologists to determine the need for further medical interventions. Patients without structural or hormonal abnormalities were followed without medical intervention, and there was no additional bleeding.
Others
Twenty-nine patients (4.5%) with Marfan syndrome were referred to our clinic by the pediatric department; most had been diagnosed with familial Marfan syndrome. Fifteen cases with traumatic injuries to the genital area comprised 2.3% of all patients who visited the clinic; most of those injuries were accidental contusions or genital lacerations. Those with superficial abrasions were discharged with topical medication, but lacerations with active bleeding required surgical intervention. Most of these patients were discharged and recovered without complications.
DISCUSSION
This study describes the clinical characteristics of pediatric patients and presents a brief review of common gynecologic problems and the diversity of medical conditions that can be expected in a pediatric and adolescent gynecology clinic. Most patients presented with concerns about genital anomalies or vaginal discharge. Chief complaints of neoplasms and issues involving vaginal bleeding were subsequent reasons for referral to the clinic. Most patients were managed conservatively; only a few underwent surgical intervention. Referral from a primary physician, direct visits to the pediatric gynecologic clinic, and referral from the pediatric department were the most common sources of patient presentation.
Genital anomalies were the most frequent clinical manifestations associated with referrals; most of these cases were diagnosed as agglutination of the labia minora. Such conditions are mostly noticed incidentally by an infant’s caregiver during routine care or observed at a health check-up.
4 Outpatient consultations are generally based on referrals from primary pediatricians based on the abnormal appearance of the genitalia or apparent absence of a vagina. Agglutination of the labia minora can appear in partial or complete form and is generally treated with estrogen cream twice a day for two weeks, followed by a once-daily application for the subsequent two weeks.
5 The need for surgical adhesiolysis in pediatric patients is rare as the tissue is easily separated by estrogen application. After treatment, caregivers are asked to maintain good perineal hygiene to prevent recurrent inflammatory conditions of the vulva.
The second most frequently encountered medical condition was vulvovaginitis, one of the most common gynecological complaints in pediatric and adolescent patients.
6 The vagina is close to the anus, and children often have difficulty maintaining anal hygiene, allowing fecal flora to be introduced into the vagina.
7 The health of the genital region is closely related to personal hygiene, a lack of which can result in vulvovaginitis. If the condition does not improve in response to treatment, clinicians should suspect vaginal foreign bodies. These can cause continuous irritation of the vaginal canal, resulting in vaginitis. If a vaginal exam is required, the clinician should pay particular attention to hymenal injuries. The usual need for sedation mandates consultation with the parents prior to the vaginal examination. Inspection during the examination should be completed with lateral and downward traction to expose problematic areas.
8 Foreign body removal should be performed with a careful approach to prevent genital or hymenal injuries. In our clinic, when a vaginal exam was required, general anesthesia was performed followed by vaginoscopy, and there were no cases of hymenal injuries.
In our cases, the pathogens causing vulvovaginal infections were identified by vaginal culture carried out with the catheter-in-catheter technique to carefully retrieve a sample without damaging the hymen or vulva. Treatment with antibiotics improved the symptoms. Patients with no specific pathogen identified were treated with conservative methods, such as sitz bathing and education to ensure proper self-hygiene.
Neoplasms in childhood are indicated mainly by non-specific clinical symptoms such as abdominal pain or distension. Generally, the incidence of ovarian neoplasm in childhood is 2.2/100,000.
9 Most cases are referred to tertiary care centers for diagnosis and discussion of appropriate treatment options. In our study, ovarian cysts, including physiologic and functional cysts, were often found incidentally during examination.
Problems involving vaginal bleeding were the least common reason for outpatient visits to the clinic in children younger than ten years. Most patients who visited the clinic with vaginal bleeding had transient symptoms or were referred from the pediatric department due to suspected precocious puberty. Considering that the mean age of menarche in Korean girls is 13.0 years,
3 problems with vaginal bleeding among children enrolled in this study were not commonly related to menstruation. In cases of suspected precocious puberty, clinicians should be aware of the available diagnostic tools, including hormone assays, ultrasound evaluation, and appropriate physical exams to assess breast development and the presence of pubic hair.
Among various pediatric traumas, the incidence of genital trauma is 0.6%.
1011 However, since more patients visit the emergency department than outpatient clinics at tertiary hospitals, it is thought that there will be differences from our clinic’s data. When a genital trauma patient visits their primary care clinic, it is necessary to determine whether it is a contusion or laceration, and to decide whether additional treatment and referral are required.
Consultation for patients with Marfan syndrome is a unique feature of our clinic. The incidence of Marfan syndrome in Korea is 1.11–2.25/100,000 below 10 years of age.
12 Our center provides treatment for height control in pediatric females with Marfan syndrome. Therefore, 4.5% of those who visited pediatric gynecology in our center had Marfan syndrome, which is an unusually large percentage. Most patients with a diagnosis of Marfan syndrome have extraordinarily tall stature and are referred from the pediatric department for growth regulation. Because patients with Marfan syndrome experience an extraordinary growth spurt when entering puberty, the pediatric department refers patients to our clinic before that acceleration of growth. Patients are closely monitored according to a growth curve and considered for treatment with appropriately timed high-dose estrogen.
13 Based on our study published in 2021, starting hormone therapy before 10.6 years is most effective in limiting the growth spurt.
14
The findings of this study illustrate the most frequent gynecologic clinical symptoms observed during pediatric period and are consistent with related studies published in the United Kingdom
15 and by the European Board and College of Obstetricians and Gynecologists.
1617 Most patients were referred from primary care and the most common symptoms were vulvovaginitis and labial adhesions. However, in contrary to previous studies, our study included only patients aged younger than ten and excluded pubertal patients, allowing us to focus on gynecological problems in the first decade of life.
This article is anticipated to provide valuable information for primary physicians who need to diagnose and manage common pediatric gynecologic problems. Determining the appropriate timing of treatment or referral is a key aspect of resolving pediatric gynecologic problems.