INTRODUCTION
Despite efforts to reduce the health inequalities among Korean regions, regional health inequalities still exist. For example, a comparison of the age-standardized mortality rates among the 17 municipal and provincial regions (hereafter “17 regions”) shows no significant changes over time in the disparities between the regions showing the highest and lowest mortality rates.
1 Regarding the regional health inequalities for healthy life expectancy, differences between the regions showing the highest and lowest health-adjusted life expectancy and quality-adjusted life expectancy, which are widely used measures of healthy life expectancy,
2 are 3.2 and 4.6 years, respectively.
34 Another study found that the regional disparity in health-adjusted life expectancy increased from 4.9 years in 2008 to 5.7 years in 2008.
5
Among many causes of regional health inequalities, one is the situation wherein residents in a region cannot receive the essential medical services when health needs arise.
6 This requires not only the existence of medical institutions that can provide essential medical care, but also the need to consider the existence of medical institutions that can satisfy the preferences of local residents. Therefore, whether a local community has the infrastructure required for a good delivery of essential medical services, which is closely related to life and has a decisive influence on health-related quality of life, must be examined. The Korean government is recently attempting to position a healthcare delivery system in each region with the Public Healthcare Network Plan and Regional Healthcare Promotion Plan.
78 As a part of such efforts, they began to designate and operate competent medical institutions (so-called “Accountable Care Hospital”) in 17 regional and 70 subregions across the country.
9 Designated medical institutions provide high-quality medical services in the essential medical fields, including trauma care, cardiocerebrovascular, maternal and neonatal, mental health, infection, cancer, and older adults’ care and rehabilitation areas at the regional and local levels.
However, the most significant in a precise regional healthcare delivery system structure is examining how local patients use healthcare services, which is the relevance index status. The data on patients’ regional healthcare service utilization patterns provide a crucial evidential basis for assembling regional and local leading medical institutions’ concrete roles and building additional ones. In Republic of Korea (hereinafter Korea), studies on relevance index have been reported in some diseases or disease areas,
101112 but they do not consider the trend analysis of relevance index of the diseases in the essential medical service fields. Park et al.
13 attempted to analyze the relevance index trends, but it was limited to one region (Ulsan Metropolitan City).
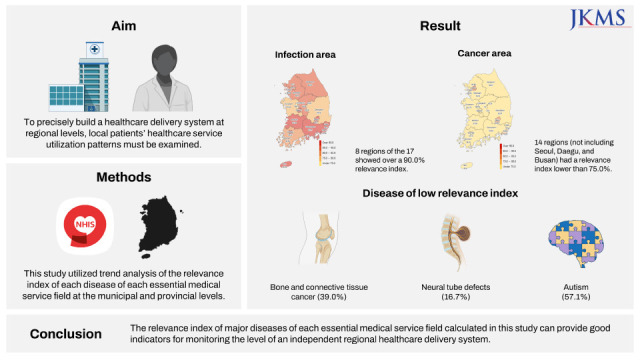
To bridge this research gap, this study aimed to analyze the trends of relevance index by region and disease in each essential medical service field. Furthermore, this study intended to broaden the scope of relevance index analysis by classifying relevance index according to service utilization type (inpatient and outpatient) and unit (number of patients and total out-of-pocket expenses).
DISCUSSION
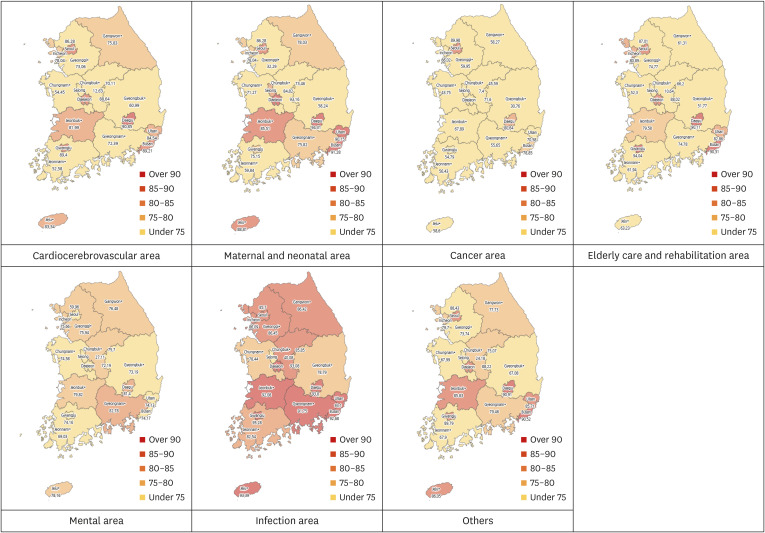
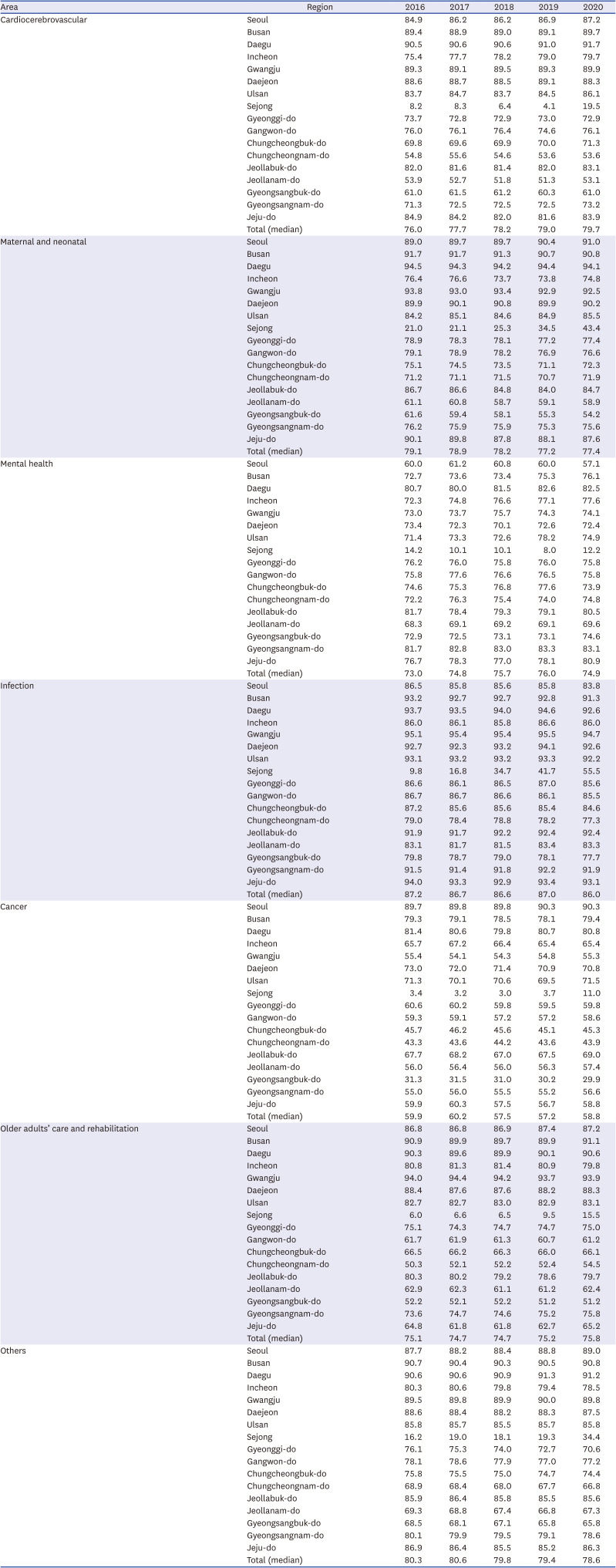
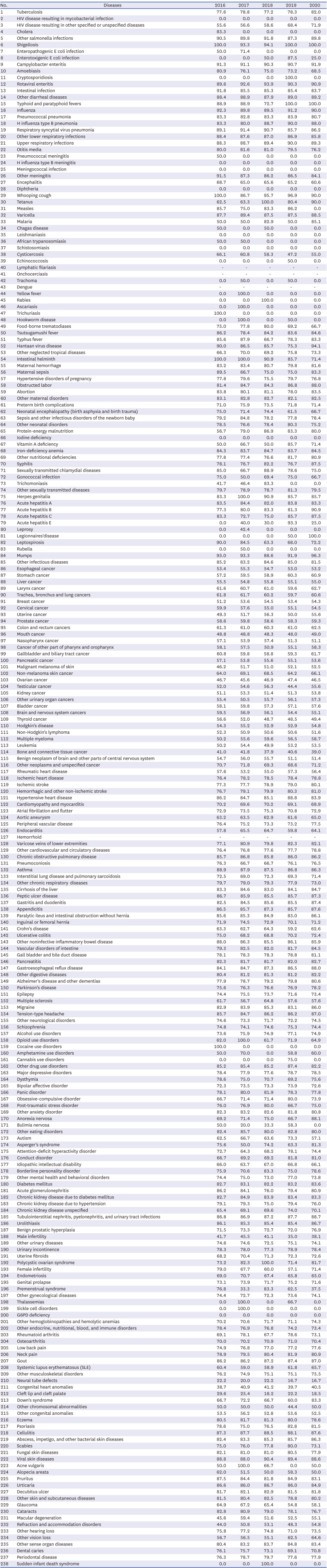
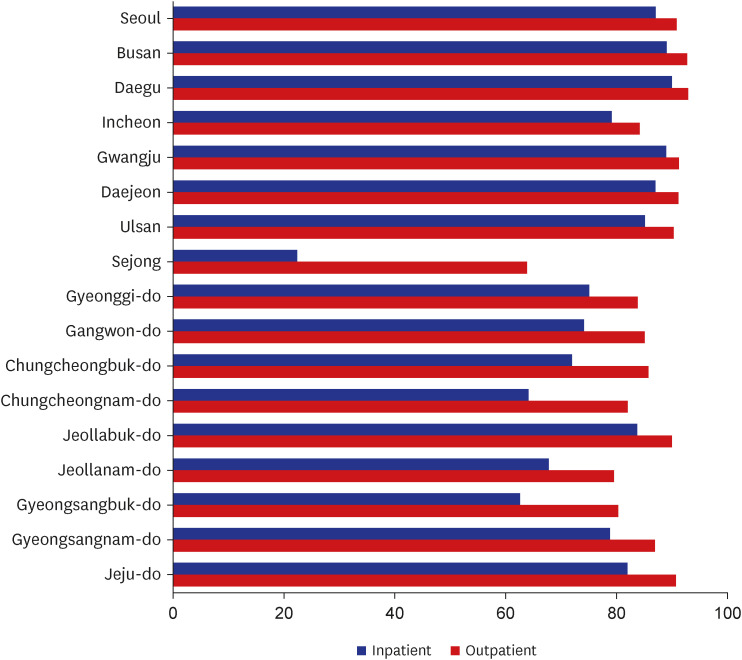
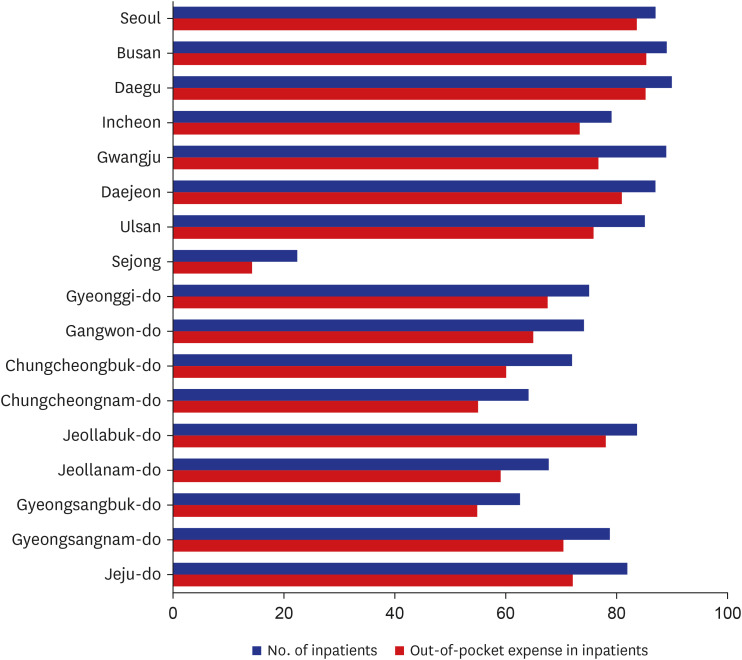
This study analyzed trends of relevance index over time (2016–2020) for each disease in each essential medical service field. The analysis results can be summarized as follows: among the essential medical service fields, the infection and cancer areas showed the highest and lowest relevance index values, respectively. Among the individual diseases, those characterized by a low relevance index were bone and connective tissue cancer (39.0%), ovarian cancer (46.5%), neural tube defects (16.7%), cleft lip and cleft palate (18.5%), and autism (57.1%). Regarding annual trends, the relevance index showed no significant improvement, overall. Moreover, in all 17 regions, inpatient care had a lower relevance index than outpatient care. Additionally, the relevance index based on total out-of-pocket expenses was lower than that based on the number of patients in all 17 regions.
Residents of any region have the right to receive high-quality essential medical services, and the government must ensure such a system. This study’s results can enable the identification of the insufficient essential medical service fields of each region and used as source data for placing a delivery system for such fields. To date, analysis of medical service regions, such as relevance index analysis, has tended to approach from the perspective of hospital divisions,
10111220 which does not provide a detailed picture of the situation in the current ever-evolving medical specialty and subspecialty system anymore. Therefore, a shift to disease-based medical service region analysis, like the one adopted in this study, is necessary to provide more detailed improvement strategies. In particular, in this study, the disease classification system of the KNBD study,
1617 which presented the ranking of disease burden as an indicator of DALYs, was used. By considering the RI ranking in this study together with the DALYs ranking by disease in the previous study,
21 it will be possible to confirm the priority of establishing a medical service supply system for each disease in the region.
From the relevance index by the essential medical service field, the infection and cancer areas showed the highest and lowest relevance index values, respectively. This highlights the urgency of constructing strategies to improve the cancer area relevance index. Despite doubts raised about the adequacy of including cancer in the essential medical service fields, because cancer is not an emergency disease, cancer certainly falls under the category of the essential medical area when defined as a medical service that significantly affects life and health-related quality of life.
14 Specifically, cancer care is not simply a matter of surgery or procedure but primarily requires continuous treatment such as chemotherapy, which is reported to be crucial for the cancer survival rate.
22 Therefore, it is necessary to establish a system capable of providing high-quality cancer care within the community. Immediately improving the relevance index related to cancer surgery may be complex; hence, constructing and operating an integrated community care system for postoperative cancer patients can be considered an alternative. The capacity to provide high-quality cancer care for each municipal and provincial region must also be reinforced, and support measures at the national level must be established for the long term.
While the cancer area had the lowest relevance index in most regions, there were exceptions to this trend, indicating the need for a strategy to support weak areas in the affected regions. For example, Seoul and Busan had the lowest relevance index in the mental health area and Jeollanam-do in the cardiocerebrovascular area. This makes it possible to infer that vulnerable essential medical service fields may exist even in metropolitan cities, such as Seoul or Busan. Additionally, even among the region where the cancer area had the lowest relevance index, there were interregional variances in the cancer type. For example, leukemia showed the lowest relevance index in Gwangju, testicular cancer in Daejeon, and bone and connective tissue cancer in Ulsan. Given these inevitable variations in the regional relevance index status among the diseases of each essential medical service field by region, coping measures customized to regional characteristics of the relevance index must be established. A disease-specific approach to improving relevance index will help identify the necessary medical staffs and equipment, and ultimately contribute to improving mortality rates in the region.
23
It is worth noting that there is no significant change in relevance index when looking at the annual change trend of relevance index. In Korea, various center designation projects, such as Regional Cancer Center,
24 have been carried out to improve the level of essential medical care system in the region, but it seems difficult to grasp the effect when considering the trends of the relevance index from this study. The insufficient level of improvement in relevance index supports the need for effective strategies to further strengthen the level of the essential medical care system in the region. Rather, the relevance index even decreased in the maternal and neonatal areas (from 79.1% in 2016 to 77.4% in 2020). It is necessary to fundamentally reexamine the delivery system improvement projects carried out in the maternal and neonatal areas, such as the Supporting Program for Obstetric Care Underserved Areas.
25 On the other hand, the relevance index slightly increased in the cardiocerebrovascular area (from 76.0% in 2016 to 79.7% in 2020), and it is necessary to examine whether the expansion of the Regional CardioCerebroVascular Center’s designation contributed to this phenomenon.
2627
Notably, the relevance index based on total out-of-pocket expenses are lower than the number of patients. This phenomenon was noticeable in all essential medical service fields in metropolitan areas, such as Busan, Daegu, and Ulsan, as well as in generally vulnerable medical regions, such as Gangwon-do and Chungcheongnam-do. This suggests that patients spend more out-of-pocket expenses when receiving essential medical services in other regions. However, the patients may receive essential medical services in other regions due to the high severity of the disease, and this severity may worsen during transit to another region. This aspect must be considered by future research by examining the treatment results of patients who have received essential medical services in regions other than their regions. If no significant difference is found in patient outcomes between the treatments in the residential and other regions, encouraging patients to receive treatment in their residential regions can help increase the health insurance cost-effectiveness. In other words, this indicates that expanding medical institutions with the capacity to provide high quality essential medical care in the region can have advantages not only in terms of equity but also in terms of financial efficiency.
This study examined only out-of-pocket expenses of health insurance, but receiving treatment in a different region involves additional costs for transport and the accompanying caregiver (if any) and additional time, doubling the total costs.
28 If local residents travel to other regions to receive essential medical services because there is no reliable healthcare delivery system in the residential region, such additional costs are incurred by them alone. Therefore, the total medical expenses spent in other regions can help estimate the costs that can be saved by building a local healthcare delivery system that ensures essential medical services.
This study has some limitations, and proposals are presented to address these limitations. First, emergency cases could not be identified in this study. For the cardiocerebrovascular area, for example, it is of utmost importance whether emergency care was provided within the crucial hour. In this study, however, relevance index analysis considered emergency and non-emergency cases combined. It does not mean that an essential health care system should be established only in emergency situations, but the inability to provide adequate medical care in the region even in emergency situations would be a bigger problem. In future research, relevance index analysis must examine whether or not the cases reviewed are emergency cases in each essential medical service field.
Second, the relevance index analysis of the trauma care area, an important essential medical service field, could not be performed. In various other injuries, such as severe trauma, it is crucial to have an emergency care delivery system capable of providing treatment within the crucial hour, as in cardiocerebrovascular disease, and build a local management system. Since the data from the National Health Insurance Service do not clearly indicate the mechanism of injury, it was difficult to analyze the relevance index in the trauma area fitting the disease classification system criteria of the KNBD study. In future research, it is necessary to reinforce the relevance index analysis of the trauma care area by using data that can confirm injury cases, such as the discharge injury in-depth survey data.
Third, the essential medical services quality provided could not be accurately assessed; the relevance index analysis only concerned whether inpatient or outpatient care was provided. In addition, it was difficult to ascertain whether the medical services provided met the expectations of patients and caregivers. In future research, this must be assessed for treatment outcomes and patient or caregiver satisfaction and experience. For example, it would be a noteworthy undertaking to examine whether there is a significant difference in the five-year survival and patient experience between cancer patients treated in their own and other regions.
Fourth, relevance index analysis must also include uncovered medical expenses. In this study, relevance index analysis was performed only on out-of-pocket expenses, and whether the inclusion of uncovered expenses will negatively affect the relevance index must be examined. If it worsens the relevance index relative to the total medical expenses compared with this study’s estimated value, the need for a medical institution providing high-quality essential medical services in the concerned region becomes more compelling.
Finally, adopting this study’s research methodology, the scope of research can be extended to analyzing the relevance index at the district and county level or in subregional units, contributing to creating subregional public health service plans or regional healthcare delivery plans. For cardiocerebrovascular and maternal and neonatal areas, specifically, having a healthcare delivery system is more advantageous at the subregional level (districts and counties) over the regional level (municipalities and provinces). Analysis of the subregional relevance index at the subregional level can help detect medically disadvantaged areas within a region.
As a strategy to reduce regional health inequalities, establishing an independent regional healthcare delivery system to provide essential medical services is drawing increasing attention. This undertaking requires extended time and continuous monitoring of the system level. The relevance index of each disease in each essential medical service field analyzed in this study can provide a good indicator to monitor the level of regionally independent essential medical services. The study’s methodology and results can form the basis for building a system capable of relevance index monitoring in a comprehensive way at the national level.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download