This article has been
cited by other articles in ScienceCentral.
PRESENTATION OF CASE 8
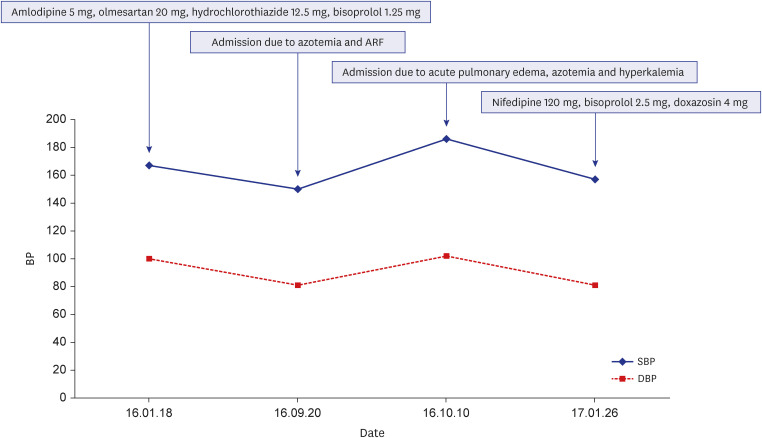
Dr. Su Nam Lee: A 58-year-old male with hypertension (HTN) presented to the cardiology clinic with uncontrolled blood pressure (BP). He had been diagnosed with HTN 3 years prior. Initially, the patient’s BP had been controlled with olmesartan 20 mg, amlodipine 5 mg, hydrochlorothiazide 12.5 mg, and bisoprolol 1.25 mg. However, when admitted to our hospital, he presented with azotemia and hyperkalemia. The patient’s medication was changed to nifedipine 120 mg, bisoprolol 2.5 mg, and doxazosin 4 mg, which improved his azotemia and pulmonary edema. This regimen was continued for approximately 10 months, during which he had no problems. However, he then restarted olmesartan 20 mg to control BP (
Fig. 1). At the time of admission, chest X-ray showed mild cardiomegaly and acute pulmonary edema (
Fig. 2), and laboratory findings revealed a blood urea nitrogen concentration of 75.9 mg/dL (normal value: 8.0–23.0 mg/dL), creatinine concentration of 1.9 mg/dL (normal value: 0.5–1.2 mg/dL), and brain natriuretic peptide concentration of 9,755 pg/mL (normal value: < 115 pg/mL).
Fig. 1
BP graphs of medication use and hospitalization history (before percutaneous transluminal renal angioplasty).
ARF = acute renal failure, BP = blood pressure, SBP = systolic blood pressure, DBP = diastolic blood pressure.
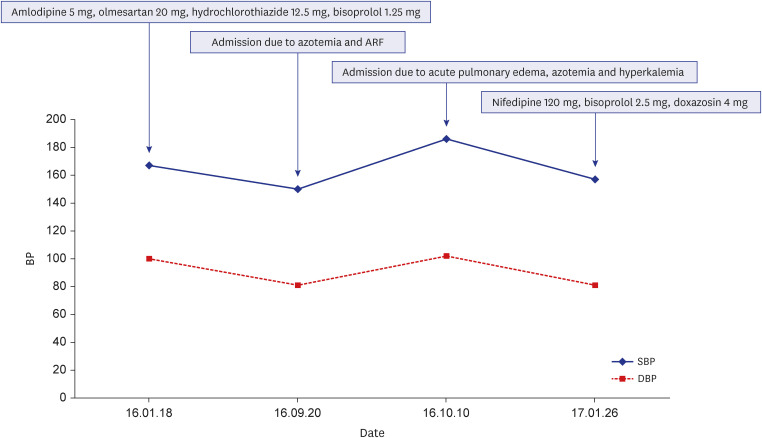
Fig. 2
Chest X-ray showed mild cardiomegaly and acute pulmonary edema, at the time of admission.

DIAGNOSIS
Dr. Gee-Hee Kim: Based on the above results, echocardiography was performed. The findings showed normal ejection fraction, left ventricular hypertrophy, and grade I diastolic dysfunction. A kidney ultrasound was performed due to acute renal failure (not provided), and the findings were indicative of left renal artery stenosis (RAS) and agenesis of the right kidney.
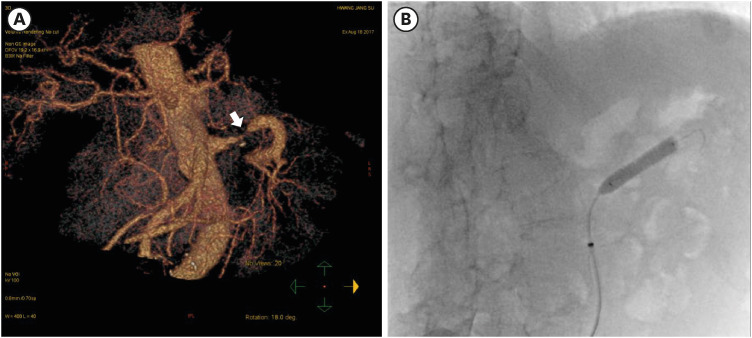
Dr. Su Nam Lee: Computed tomography revealed a solitary kidney and left RAS (
Fig. 3A). Based on the above results, percutaneous transluminal renal angioplasty was performed using a 7 × 29 mm stent (Omnilink Elite; Abbott Laboratories, Chicago, IL, USA) (
Fig. 3B). Following angioplasty, the patient’s pulmonary edema, cardiomegaly, and acute renal failure resolved.
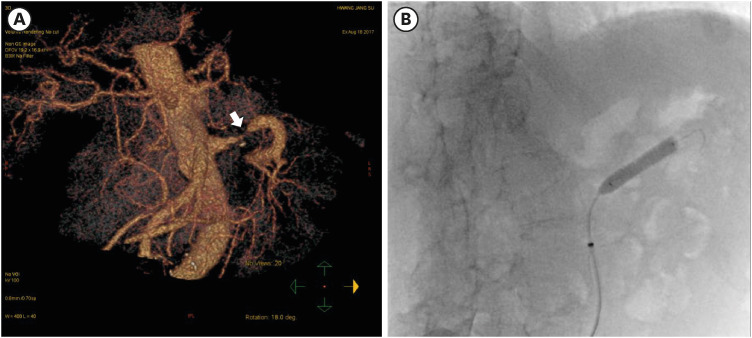
Fig. 3
Images of the left renal artery stenosis. (A) Solitary kidney and left renal artery stenosis on computed tomography. (B) A percutaneous transluminal renal angioplasty was performed using a 7 × 29 mm stent (Omnilink Elite; Abbott Laboratories, Chicago, IL, USA).
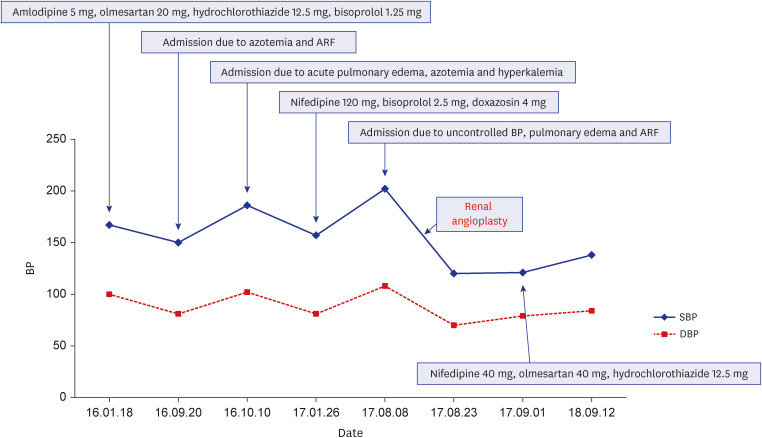
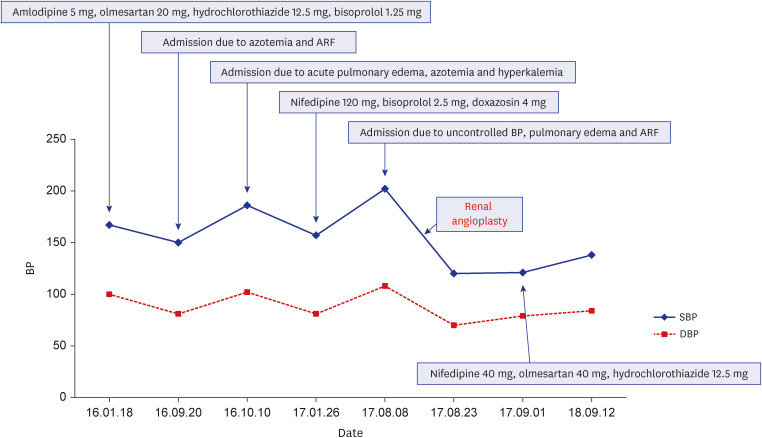
Dr. Gee-Hee Kim: At the 18-month follow-up after angioplasty, the patient’s BP was well controlled with nifedipine 40 mg, lmesartan 40 mg, and hydrochlorothiazide 12.5 mg without any symptoms (
Fig. 4).
Fig. 4
BP graphs of medication use and hospitalization history (include after percutaneous transluminal renal angioplasty).
ARF = acute renal failure, BP = blood pressure, SBP = systolic blood pressure, DBP = diastolic blood pressure.
DIFFERENTIAL DIAGNOSIS OF ACUTE PULMONARY EDEMA
Dr. Gee-Hee Kim: Heart failure with preserved ejection fraction (HfpEF) can be considered the cause of acute pulmonary edema based on B-type natriuretic peptide elevation and diastolic dysfunction on echocardiography. However, after changing drugs and stenting the renal artery, pulmonary edema and acute kidney injury (AKI) were improved even when using conventional drugs such as angiotensin receptor blockers (ARBs). Another possible cause of worsening pulmonary edema and AKI other than HfpEF should be considered.
Dr. Joon-Sung Choi: In addition, acute pulmonary edema might have been due to fluid overload caused by AKI of unknown cause. However, edema also improved after changing drugs. Furthermore, renal function improved after renal artery stenting, indicating that acute pulmonary edema did not occur due to the AKI.
FINAL DIAGNOSIS
Dr. Gee-Hee Kim: In conclusion, the patient had one kidney and continued to experience complication with ARBs after RAS of the intact kidney. Based on the above results, the patient was diagnosed with Pickering syndrome.
DISEASE MANAGEMENT
Dr. Gee-Hee Kim: Current guidelines recommend screening for RAS in patients with unexplained acute pulmonary edema and uncontrolled HTN.
12 Renal revascularization is the treatment of choice for patients with Pickering syndrome. The American College of Cardiology/American Heart Association (ACC/AHA) guidelines endorse percutaneous revascularization as a class I recommendation for patients with hemodynamically significant RAS and recurrent pulmonary edema.
3
DISCUSSION
Dr. Gee-Hee Kim: In 1988, the association of bilateral or solitary functioning kidney RAS with acute pulmonary edema in azotemic hypertensive patients was first reported by Pickering et al.,
4 and flash pulmonary edema in patients with RAS has since been termed Pickering syndrome. And we successfully performed percutaneous transluminal angioplasty in a patient with RAS and a congenital solitary kidney. RAS has been increasingly diagnosed and is strongly associated with atherosclerotic diseases including coronary, carotid, and peripheral diseases. Among patients with atherosclerotic RAS in a previous study, 20% had significant bilateral disease.
5 The prevalence of pulmonary edema appears dependent on pressure load and degree of renal dysfunction.
5 Overall, one study reported weighted prevalence of flash pulmonary edema in patients with RAS of 15.3%.
5 Flash pulmonary edema and RAS in a solitary congenital kidney are less common.
Dr. Min-Sik Kim: Pickering et al.
4 reported a case series of 11 hypertensive patients with bilateral renovascular disease who presented with recurrent pulmonary edema. There are three major pathophysiological mechanisms of pulmonary edema in bilateral RAS: defective natriuresis,
1 increased hemodynamic burden and exacerbation of diastolic dysfunction,
2 and failure of the pulmonary capillary blood-gas barrier.
6 In a previous study including patients with Pickering syndrome, the reported mean age was 63 years, 47% were male, and 73% were smokers.
6
Dr. Su Nam Lee: The current guidelines recommend renal revascularization for patients with hemodynamically significant RAS and recurrent, unexplained heart failure.
3 Although both surgery and percutaneous revascularization have been successful in treating RAS, the ACC/AHA guidelines endorse percutaneous revascularization as a class I recommendation for hemodynamically significant RAS.
3 The procedure is successful in 82–100% of patients, and stenosis recurs in 10–11% of patients.
7
Dr. Gee-Hee Kim: Physicians should carefully monitor RAS in patients with recurrent, unexplained heart failure and uncontrolled BP. Percutaneous revascularization is the treatment of choice for hemodynamically significant RAS. Refractory HTN due to RAS in a solitary kidney has been reported in China and Japan.
89 Herein, we presented a case of recurrent pulmonary edema and uncontrolled HTN due to RAS in a patient with a congenital solitary kidney who underwent successful percutaneous transluminal renal angioplasty.
ACKNOWLEDGMENTS
The Case Conference section was prepared in the Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
References
1. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006; 113(11):e463–e654. PMID:
16549646.
2. European Stroke Organisation. Tendera M, Aboyans V, Bartelink ML, Baumgartner I, Clément D, et al. ESC guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32(22):2851–2906. PMID:
21873417.
3. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006; 47(6):1239–1312. PMID:
16545667.
4. Pickering TG, Herman L, Devereux RB, Sotelo JE, James GD, Sos TA, et al. Recurrent pulmonary oedema in hypertension due to bilateral renal artery stenosis: treatment by angioplasty or surgical revascularisation. Lancet. 1988; 2(8610):551–552. PMID:
2900930.
5. Chrysochou C, Kalra PA. Epidemiology and natural history of atherosclerotic renovascular disease. Prog Cardiovasc Dis. 2009; 52(3):184–195. PMID:
19917329.
6. Messerli FH, Bangalore S, Makani H, Rimoldi SF, Allemann Y, White CJ, et al. Flash pulmonary oedema and bilateral renal artery stenosis: the Pickering syndrome. Eur Heart J. 2011; 32(18):2231–2235. PMID:
21406441.
7. Safian RD, Textor SC. Renal-artery stenosis. N Engl J Med. 2001; 344(6):431–442. PMID:
11172181.
8. Hayashida M, Watanabe N, Imamura H, Kumazaki S, Kitabayashi H, Takahashi W, et al. Congenital solitary kidney with renovascular hypertension diagnosed by means of captopril-enhanced renography and magnetic resonance angiography. Int Heart J. 2005; 46(2):347–353. PMID:
15876820.
9. Yan X, Ding M, Li J, Zhan H, Zuo Y, Wang H, et al. Refractory hypertension due to renal artery stenosis in a solitary kidney: case report and literature review. Int J Clin Exp Med. 2018; 11(3):2778–2784.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download