To the Editor
We read with interest the article by Kim et al.1 on the long-term control of diabetes mellitus (DM) after visiting a tertiary university hospital. In this study, patients were categorized into 4 groups based on HbA1c changes at three months; Best (≥ 1.6% decrease), Better (0.5-1.5% reduction), Neutral (≤ 0.4% decrease or ≤ 0.4% increase), and Worst (≥ 0.5% increase). The Best group had the best control up to 7 years, regardless of the baseline Hba1c. The groups with improvement (Best and Better) had lower risk for complications (cardiac and cerebrovascular), albeit not significant. This study provided important guides for target HbA1c reductions within 3, if not 12 months (no data on 3-month HbA1c reported). The accompanying editorial stressed on this and highlighted the benefits of the ‘legacy effects’, and alluded to factors that contribute to poor control that included beta cell dysfunctions, inconsistencies with guidelines and practices, and clinical inertia especially in the primary care settings.2 Treatment at primary and even secondary care levels are usually a bottom-up approach (stepwise increase in medications) and there also may be clinical inertia on part of doctors to introduce or escalate, including use of insulin, mainly for fear of inducing hypoglycemia and patient’s reluctance to accept treatment modifications.
Interestingly in Kim et al.’s study, Fig. 2 highlighted the effects of robust management strategies, in this case following their institutional management guideline. It showed the HbA1c trends among the 4 groups according to baseline HbA1c, and the ‘Best-group’ universally achieved good control throughout. The magnitude of improvement was directly correlated with baseline HbA1c, albeit minimal in the group with HbA1C ≤ 7%. Continuing improvements seen until 12 months are most likely to be related to medications. The other three groups also showed improvement (Fig. 2; CE) but require further attention.
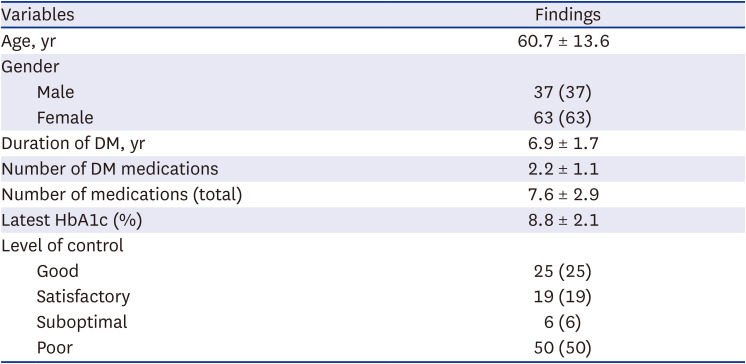
We recently looked at the HbA1c (done at 3-6 months intervals) trend of 100 consecutive patients (mean of 9.1 readings per patient) seen in a district general hospital (Table 1). For the HbA1c trends we categorized patients into controlled (Good/satisfactory; HbA1c ≤ 8.0%) and uncontrolled (Suboptimal/poor; > 8.0%) groups. Based on the latest control, 44% had good/satisfactory control. Prior HbA1c trend remained stable in 29%, while 12% showed downward trend towards being controlled, and 3% showed upward trend with slight deterioration in control. The remaining 56% of uncontrolled patients meanwhile include range bound in 28%, slight improvement and downward trend in 13%, and deterioration and upward trend in 15%. The overall mean HbA1c fluctuation from the mean of HbA1c level was 3.2 ± 2.2%, lower in the good controlled group (2.5 ± 2.4%) compared to the uncontrolled group (3.8 ± 1.9%). In our patients, suboptimal or poor controls, and fluctuations were mainly due to patients’ factors; poor compliance and impacts of other comorbid conditions. Good control is central to preventing long-term complications, and the ‘legacy effect’ is not only seen in DM but also other conditions.345 Although early good control has been shown to provide greater beneficial impact on clinical outcomes, achieving good control at any time of disease is important. As shown in our study, DM control is dynamic with fluctuations, and it is important for clinicians to be aware that even controlled patients can become uncontrolled. This will necessitate treatment adjustment such as altering dose of medications if not yet maximized, using newer agents (Sodium-Glucose Transport Protein 2 [SGLT2] Inhibitors and dipeptidyl peptidase-4 [DPP-4] inhibitor), assessment of beta cell dysfunctions (interval C-peptide assessment which is not routinely done), and most importantly, further targeted education to improve understanding, and compliance (medications, diet and lifestyle). However, being able to predict patients who need close monitoring through the early HbA1C profile as suggested by Kim et al. is welcome knowledge.
References
1. Kim H, Jung DY, Lee SH, Cho JH, Yim HW, Kim HS. Long-term changes in HbA1c according to blood glucose control status during the first 3 months after visiting a Tertiary university hospital. J Korean Med Sci. 2022; 37(38):e281. PMID: 36193638.
2. Lee N, Kim DJ. The degree of glycemic control for the first three months determines the next seven years. J Korean Med Sci. 2022; 37(38):e301. PMID: 36193642.
3. Chalmers J, Cooper ME. UKPDS and the legacy effect. N Engl J Med. 2008; 359(15):1618–1620. PMID: 18843126.
4. Parati G, Bilo G, Ochoa JE. Benefits of tight blood pressure control in diabetic patients with hypertension: importance of early and sustained implementation of effective treatment strategies. Diabetes Care. 2011; 34(Suppl 2):Suppl 2. S297–S303. PMID: 21525472.
5. Lind M, Imberg H, Coleman RL, Nerman O, Holman RR. Historical HbA1c values may explain the type 2 diabetes legacy effect: UKPDS 88. Diabetes Care. 2021; 44(10):2231–2237. PMID: 34244332.
Table 1
Characteristics of DM patients (N = 100)




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download