1. Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018; 130(4):1–18.
2. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18(1):56–87. PMID:
30497965.
3. Kim HK, Leigh JH, Lee YS, Choi Y, Kim Y, Kim JE, et al. Decreasing incidence and mortality in traumatic brain injury in Korea, 2008–2017: a population-based longitudinal study. Int J Environ Res Public Health. 2020; 17(17):6197. PMID:
32859061.
4. Te Ao B, Brown P, Tobias M, Ameratunga S, Barker-Collo S, Theadom A, et al. Cost of traumatic brain injury in New Zealand: evidence from a population-based study. Neurology. 2014; 83(18):1645–1652. PMID:
25261503.
5. Brenner LA, Grassmeyer RP, Biffl S, Kinney AR, Dise-Lewis JE, Betthauser LM, et al. Met and unmet rehabilitative needs among pediatric patients with moderate to severe TBI. Brain Inj. 2021; 35(10):1162–1167. PMID:
34554040.
6. Rassovsky Y, Levi Y, Agranov E, Sela-Kaufman M, Sverdlik A, Vakil E. Predicting long-term outcome following traumatic brain injury (TBI). J Clin Exp Neuropsychol. 2015; 37(4):354–366. PMID:
25832742.
7. Liao CC, Chiu WT, Yeh CC, Chang HC, Chen TL. Risk and outcomes for traumatic brain injury in patients with mental disorders. J Neurol Neurosurg Psychiatry. 2012; 83(12):1186–1192. PMID:
22773855.
8. Nordström A, Edin BB, Lindström S, Nordström P. Cognitive function and other risk factors for mild traumatic brain injury in young men: nationwide cohort study. BMJ. 2013; 346:f723. PMID:
23482939.
9. Daugherty J, Sarmiento K, Waltzman D, Xu L. Traumatic brain injury–related hospitalizations and deaths in urban and rural counties—2017. Ann Emerg Med. 2022; 79(3):288–296.e1. PMID:
34742590.
10. Plancikova D, Leitgeb J, Brazinova A, Melichova J, Sivco P, Nemcovska E, et al. Characteristics and outcome of severe traumatic brain injuries based on occupational status. Eur J Trauma Emerg Surg. 2021; 47(6):2035–2041. PMID:
32306121.
11. Haines KL, Nguyen BP, Vatsaas C, Alger A, Brooks K, Agarwal SK. Socioeconomic status affects outcomes after severity-stratified traumatic brain injury. J Surg Res. 2019; 235:131–140. PMID:
30691786.
12. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017; 389(10077):1475–1490. PMID:
28402829.
13. Bruns J Jr, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003; 44(s10):2–10.
14. Kraus JF, Fife D, Ramstein K, Conroy C, Cox P. The relationship of family income to the incidence, external causes, and outcomes of serious brain injury, San Diego County, California. Am J Public Health. 1986; 76(11):1345–1347. PMID:
3766837.
15. Yue JK, Upadhyayula PS, Avalos LN, Cage TA. Pediatric traumatic brain injury in the United States: rural-urban disparities and considerations. Brain Sci. 2020; 10(3):135. PMID:
32121176.
16. Schiraldi M, Patil CG, Mukherjee D, Ugiliweneza B, Nuño M, Lad SP, et al. Effect of insurance and racial disparities on outcomes in traumatic brain injury. J Neurol Surg A Cent Eur Neurosurg. 2015; 76(3):224–232. PMID:
25798799.
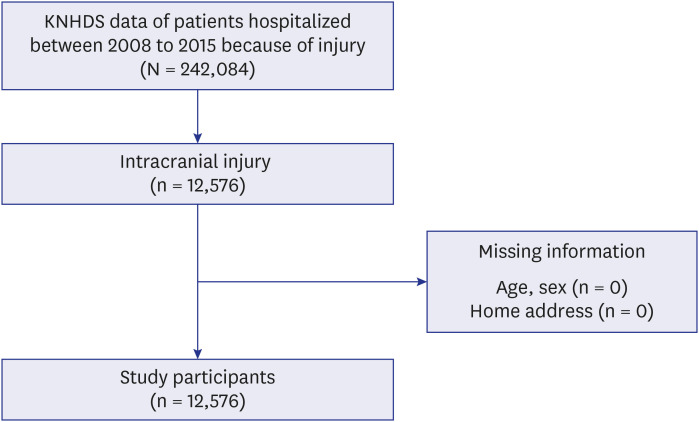
17. Hong SO, Kim B, Jo J, Kwon Y, Lee YK, Kim Y. Main results of the Korea National Hospital Discharge In-depth Injury Survey, 2004-2016. Epidemiol Health. 2020; 42:e2020044. PMID:
32580533.
18. Lee YK, Hong SO, Park SJ, Park M, Wang K, Jo M, et al. Data resource profile: the Korea National Hospital Discharge In-depth Injury Survey. Epidemiol Health. 2021; 43:e2021052. PMID:
34412448.
19. Korea Centers for Disease Control & Prevention. Korean Standard Classification of Disease. Version 5. Seoul, Korea: Korea Centers for Disease Control & Prevention;2008.
20. Park HA, Lee HA, Park JO. Association between area-level socioeconomic deprivation and prehospital delay in acute ischemic stroke patients: an ecological study. Int J Environ Res Public Health. 2020; 17(20):7392.
21. Statistics Korea. Ten Percent Sample of 2010 Population and Housing Census. MDIS, RAS. Daejeon, Korea: Statistics Korea;2011.
22. Choi MH, Cheong KS, Cho BM, Hwang IK, Kim CH, Kim MH, et al. Deprivation and mortality at the town level in Busan, Korea: an ecological study. J Prev Med Public Health. 2011; 44(6):242–248. PMID:
22143174.
23. Kwak M, Kim C. Disparities by age, sex, tumor stage, diagnosis path, and area-level socioeconomic status in survival time for major cancers: results from the Busan Cancer Registry. J Korean Med Sci. 2017; 32(12):1974–1983. PMID:
29115079.
24. Yun JW, Kim YJ, Son M. Regional deprivation index and socioeconomic inequalities related to infant deaths in Korea. J Korean Med Sci. 2016; 31(4):568–578. PMID:
27051241.
25. Benach J, Yasui Y, Borrell C, Sáez M, Pasarin MI. Material deprivation and leading causes of death by gender: evidence from a nationwide small area study. J Epidemiol Community Health. 2001; 55(4):239–245. PMID:
11238578.
26. Bedrick EJ. Adjusted chi-squared tests for cross-classified tables of survey data. Biometrika. 1983; 70(3):591–595.
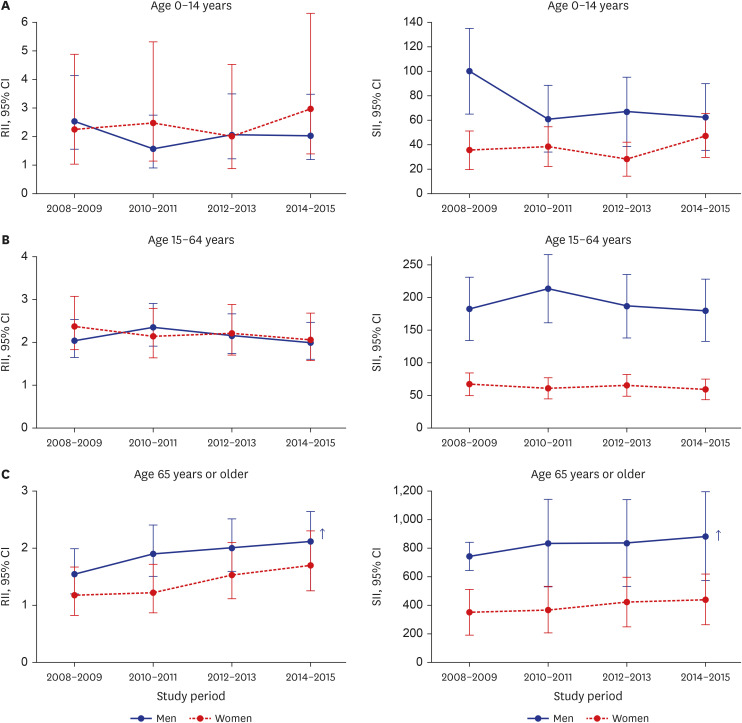
27. Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997; 44(6):757–771. PMID:
9080560.
28. Pamuk ER. Social class inequality in mortality from 1921 to 1972 in England and Wales. Popul Stud (Camb). 1985; 39(1):17–31. PMID:
11611750.
29. Moreno-Betancur M, Latouche A, Menvielle G, Kunst AE, Rey G. Relative index of inequality and slope index of inequality: a structured regression framework for estimation. Epidemiology. 2015; 26(4):518–527. PMID:
26000548.
30. Ernstsen L, Strand BH, Nilsen SM, Espnes GA, Krokstad S. Trends in absolute and relative educational inequalities in four modifiable ischaemic heart disease risk factors: repeated cross-sectional surveys from the Nord-Trøndelag Health Study (HUNT) 1984-2008. BMC Public Health. 2012; 12(1):266. PMID:
22471945.
31. Lefevre-Dognin C, Cogné M, Perdrieau V, Granger A, Heslot C, Azouvi P. Definition and epidemiology of mild traumatic brain injury. Neurochirurgie. 2021; 67(3):218–221. PMID:
32387427.
32. Yamamoto S, Levin HS, Prough DS. Mild, moderate and severe: terminology implications for clinical and experimental traumatic brain injury. Curr Opin Neurol. 2018; 31(6):672–680. PMID:
30379702.
33. Andriessen TM, Horn J, Franschman G, van der Naalt J, Haitsma I, Jacobs B, et al. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: a prospective multicenter study. J Neurotrauma. 2011; 28(10):2019–2031. PMID:
21787177.
34. Bellner J, Jensen SM, Lexell J, Romner B. Diagnostic criteria and the use of ICD-10 codes to define and classify minor head injury. J Neurol Neurosurg Psychiatry. 2003; 74(3):351–352. PMID:
12588924.
35. Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien). 2006; 148(3):255–268. PMID:
16311842.
36. Warwick J, Slavova S, Bush J, Costich J. Validation of ICD-10-CM surveillance codes for traumatic brain injury inpatient hospitalizations. Brain Inj. 2020; 34(13-14):1763–1770. PMID:
33280404.
37. Barker-Collo S, Theadom A, Jones K, Feigin VL, Kahan M. Accuracy of an International Classification of Diseases code surveillance system in the identification of traumatic brain injury. Neuroepidemiology. 2016; 47(1):46–52. PMID:
27504965.
38. Bazarian JJ, Veazie P, Mookerjee S, Lerner EB. Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad Emerg Med. 2006; 13(1):31–38. PMID:
16365331.
39. Carroll CP, Cochran JA, Guse CE, Wang MC. Are we underestimating the burden of traumatic brain injury? Surveillance of severe traumatic brain injury using centers for disease control International Classification of Disease, Ninth Revision, clinical modification, traumatic brain injury codes. Neurosurgery. 2012; 71(6):1064–1070. PMID:
22922677.
40. Andelic N, Anke A, Skandsen T, Sigurdardottir S, Sandhaug M, Ader T, et al. Incidence of hospital-admitted severe traumatic brain injury and in-hospital fatality in Norway: a national cohort study. Neuroepidemiology. 2012; 38(4):259–267. PMID:
22678449.
41. Southern DA, McLaren L, Hawe P, Knudtson ML, Ghali WA. APPROACH Investigators. Individual-level and neighborhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care. 2005; 43(11):1116–1122. PMID:
16224305.
42. Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001; 55(2):111–122. PMID:
11154250.
43. Laflamme L, Burrows S, Hasselber M. Socioeconomic Differences in Injury Risks: A Review of Findings and a Discussion of Potential Countermeasures. Copenhagen, Denmark: WHO Regional Office for Europe;2009.
44. Zoni AC, Domínguez-Berjón MF, Esteban-Vasallo MD, Velázquez-Buendía LM, Blaya-Nováková V, Regidor E. Socioeconomic inequalities in injuries treated in primary care in Madrid, Spain. J Public Health (Oxf). 2017; 39(1):45–51. PMID:
26869695.
45. Cubbin C, Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health. 2002; 23(1):349–375. PMID:
11910067.
46. Morency P, Gauvin L, Plante C, Fournier M, Morency C. Neighborhood social inequalities in road traffic injuries: the influence of traffic volume and road design. Am J Public Health. 2012; 102(6):1112–1119. PMID:
22515869.
47. Merom D, Pye V, Macniven R, van der Ploeg H, Milat A, Sherrington C, et al. Prevalence and correlates of participation in fall prevention exercise/physical activity by older adults. Prev Med. 2012; 55(6):613–617. PMID:
23064022.
48. Sengoelge M, Leithaus M, Braubach M, Laflamme L. Are there changes in inequalities in injuries? A review of evidence in the WHO European region. Int J Environ Res Public Health. 2019; 16(4):653. PMID:
30813329.
49. Magid A, Leibovitch-Zur S, Baron-Epel O. Increased inequality in mortality from road crashes among Arabs and Jews in Israel. Traffic Inj Prev. 2015; 16(1):42–47. PMID:
24679219.
50. Huh KR, Kim JY, Choi SH, Yoon YH, Park SJ, Lee ES. Comparison of traumatic brain injury patients with brain computed tomography in the emergency department by age group. Clin Exp Emerg Med. 2020; 7(2):81–86. PMID:
32635698.
51. Choi SW, Woo JH, Hyun SY, Jang JH, Choi WS. Factors associated with injury severity among users of powered mobility devices. Clin Exp Emerg Med. 2021; 8(2):103–110. PMID:
34237815.
52. Munivenkatappa A, Agrawal A, Shukla DP, Kumaraswamy D, Devi BI. Traumatic brain injury: does gender influence outcomes? Int J Crit Illn Inj Sci. 2016; 6(2):70–73. PMID:
27308254.
53. Yang BM, Kim J. Road traffic accidents and policy interventions in Korea. Inj Control Saf Promot. 2003; 10(1-2):89–94. PMID:
12772491.
54. Gao S, Kumar RG, Wisniewski SR, Fabio A. Disparities in health care utilization of adults with traumatic brain injuries are related to insurance, race, and ethnicity: a systematic review. J Head Trauma Rehabil. 2018; 33(3):E40–E50. PMID:
28926481.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download