INTRODUCTION
Declines in deaths from infectious or congenital disease have given way to increases in deaths from injury-related causes, including drug overdose.
123 Poisoning has been identified as one of the major causes of pediatric emergency presentations and intentionally poisoned adolescent patient rate has been increasing annually.
4567 Given the changes in the patterns and main risks of acute poisoning, epidemiological surveillance is necessary to determine the extent and characteristics of the problem, according to which related preventive measures can be taken.
28910
The coronavirus disease 2019 (COVID-19) first appeared in December 2019 and spread rapidly worldwide, prompting the World Health Organization to characterise COVID-19 as a pandemic on 11 March 2020. While continuously trying to increase the vaccination rate, many countries have implemented various social distancing measures to prevent the spread of the virus, which have changed the current way of life. The use of masks/disinfectants has become routine, with many countries imposing quarantine, leading to the closure of public parks and meeting places, including schools, recreational institutions and sport centres, which play a significant role in socialisation.
11 Consequently, people experienced forced social isolation, which can promote not only psychological distress and a depressive mood but also psychotic bouts and suicidal thoughts. Moreover, several people have dealt with the fear of falling ill while also perceiving the eventual economic stress and loss of loved ones, which promotes a growing feeling of uncertainty and anxiety.
12 These considerable and abrupt changes of social circumstances during the COVID-19 pandemic have caused substantial changes in the everyday life of children and adolescents; hence, mental health problems in this vulnerable group have been inevitable, with children also experiencing some psychological impact.
111213 Consequently, the increase in mental illness among adolescents during the COVID-19 pandemic has increased the incidence of substance use disorders and self-harm attempts.
14 However, since the start of the COVID-19 pandemic, changes in the status of acutely poisoned patients, particularly among children and adolescents, have remained unclear.
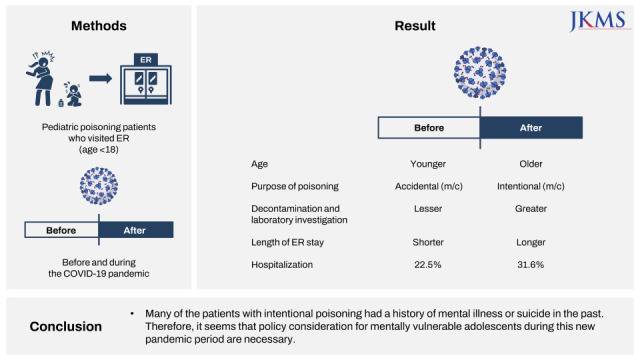
The current study was therefore conducted to investigate the changes in the epidemiology and clinical characteristics of pediatric poisoning cases who visited the emergency department (ED) before and during the COVID-19 pandemic.
METHODS
Study population
We retrospectively reviewed the medical records of pediatric patients under the age of 18 who visited the ED of Ajou University Hospital, South Korea, a regional tertiary referral centre, from January 2018 to December 2021. We included patients with the keywords ‘poisoning’ and ‘toxic effect’ in the final diagnosis on discharge from an ED. Patients who had incomplete data or visited for follow-up were excluded.
Data collection
We divided enrolled patients into the pre-COVID-19 and COVID-19 group to compare the poisoning patterns before and during the COVID-19 pandemic. The pre-COVID-19 period spanned from January 2018 to December 2019, whereas the COVID-19 period spanned from January 2020 to December 2021. The general characteristics, intentionality of poisoning, caused materials, underlying disease, history of past suicide attempts, etc. were subsequently determined. Treatment methods, the length of ED stay and treatment results were analysed. Poisonous materials were classified into therapeutic drugs, artificial poisonous materials, natural toxins and gases. The clinical characteristics of poisoning before and during the COVID-19 pandemic were then compared.
Statistical analyses
The primary purpose of this study was to compare the number of patients visiting the ED due to poisoning between the pre-COVID-19 and COVID-19 period. The secondary purpose was to compare the clinical characteristics of poisoning between both groups. Continuous variables were presented as medians or means ± standard deviations. Categorical variables were presented as frequencies or percentages. Student’s t-test was used for continuous variables with normal distribution, whereas the Mann–Whitney test was used for continuous variables without a normal distribution. The χ2 test or Fisher’s exact test was used to analyse categorical data. Statistical analyses were performed using SPSS 15.0 (SPSS, Chicago, IL, USA), with P values < 0.05 indicating statistical significance.
Ethics statement
Ethical approval was obtained from the Institutional Review Board of Ajou University Hospital (AJIRB-MED-MDB-21-721) which waived the need for informed consent. The study was also conducted in accordance with the principles of the Helsinki Declaration.
DISCUSSION
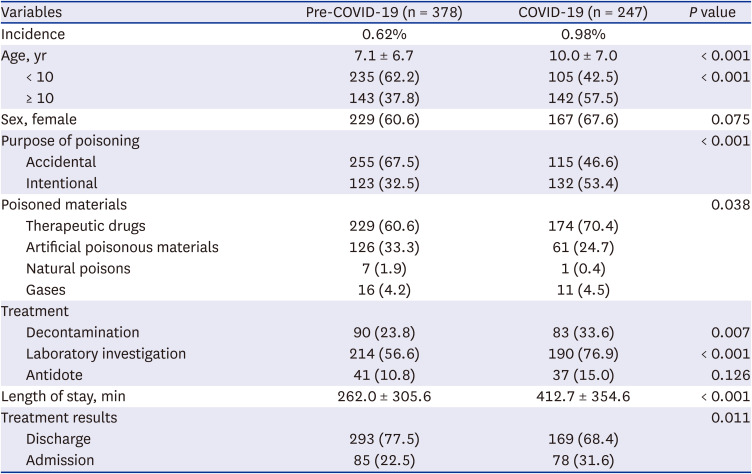
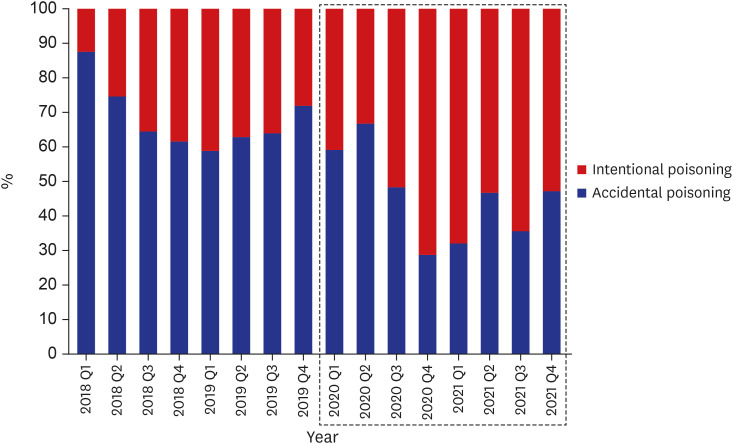
The current study has been the first to analyse the changes in poisoning characteristics among children and adolescents visiting the ED before and during the COVID-19 pandemic. During the COVID-19 period, the number of visits to the pediatric ED due to poisoning increased to 0.98%. In particular, the number of adolescent patients increased to 57.5% and intentional poisoning events accounted for 53.4% of all poisoning cases. The results of a previous study at the same hospital showed a significant difference compared to 33.6% of adolescents and 16.8% of intentional poisoning. Although not confirmed in previous studies, our study found that patients with many suicide attempts in the past tend to be more exposed to intentional poisoning during the COVID-19 pandemic.
Owing to the COVID-19 pandemic, the government had implemented various quarantine policies. In line with this, wearing of masks has become commonplace, whereas social distancing, suspension of schools, remote education and social activities had a considerable impact on the life patterns of children and adolescents.
111213 As such, the epidemiology of childhood and adolescent diseases also changed significantly, and the number of pediatric patients visiting the ED also plummeted as the incidence of infectious disease shared by near-field droplet transmission decreased.
15 However, several studies have suggested an increase in mental health problems among children and adolescents due to the prolonged social distancing.
1213 Changes in the living environment have been confirmed to include an increase in patients with sleep disorders, post-traumatic stress disorder, depression, anxiety, increased suicidal thoughts, increased actual suicide attempts and addiction.
16 The current study confirmed that the total number of pediatric patients visiting the ED decreased by less than half during the COVID-19, whereas the proportion of patients visiting due to poisoning increased from 0.62% to 0.98%. Moreover, the increase in the frequency of intentional poisoning cases during the COVID-19 period reaffirmed the results of several previous studies showing that suicide attempts of poisoning were increasing.
Poisoning among younger children can be characterised as highly accidental, whereas adolescents suffer from highly intentional poisoning, with the frequency being greater in females.
1678 During the COVID-19 period, the average age of the patients increased with females comprising most of the cases, reflecting the increased number of adolescents visiting due to intentional poisoning. In addition, therapeutic drug poisoning increased during the COVID-19 period, which also reflects the characteristics observed in intentional poisoning. In fact, an epidemiological study on pediatric poisoning conducted at the same hospital more than a decade ago revealed that artificial poisonous materials accounted for 32.1% of all poisoning cases.
1 While the proportion of artificially poisonous materials accounted 33.3% during the pre-COVID-19 period, we found a gradual decrease in the proportion (24.7%) during the COVID-19 period. Given the need for social distancing due to the COVID-19 pandemic, parents spent more time directly caring for infants and toddlers. Notably, with the increase in parental education regarding safety accidents at home compared to the past, accidental poisoning may have decreased.
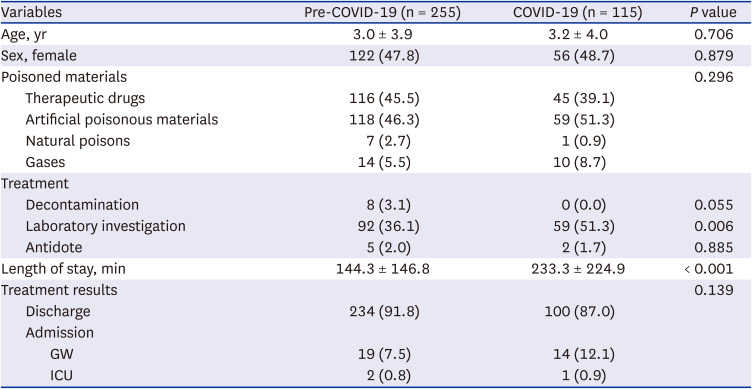
We conducted a sub-analysis of patients according to poising purposes before and during COVID-19. Accordingly, among those who suffered accidental poisoning, no difference in age and sex ratio was observed between the pre-COVID-19 and COVID-19 groups. During both periods, several therapeutic drugs and artificial toxins had been involved in accidental poisoning cases. In the case of therapeutic drugs, a difference in the frequency of detailed drug types was noted during the two periods. Notably, antipyretics/NSAIDs, respiratory drugs and antibiotics were more frequent in the pre-COVID-19 group. Our findings on the common therapeutic drugs involved in poisoning during the pre-COVID-19 period were similar to that reported in previous studies.
13 On the other hand, iron/vitamin supplements, cardiovascular drugs and hormones were most frequent during the COVID-19 period. The different frequencies of poisonous drugs may be attributed to the decrease in infectious diseases rates during the COVID-19 pandemic.
15 During the pre-COVID-19 period, many children had suffered from infectious diseases, such as common colds, with visits largely being due to misuse and accidental ingestion of their prescribed drugs.
1 During the COVID-19 period, the frequency of pediatric medication decreased as infection rates slowed and the number of patients visiting the hospital due to drug misuse itself decreased. On the other hand, iron/vitamin supplements, which are personal health products, are taken more often. Accordingly, their guardian’s drugs have been considered the primary cause of majority of the accidental poisoning cases among children. Among the COVID-19 group, more children visited the ED due to exposure to drugs that may have toxic effects, such as hypertension drugs and hormones, consequently increasing the frequency of blood tests and observation time at the ED. No difference was observed in other treatment or hospitalisation rates. We can reaffirm that toddlers rarely suffer fatal consequences with small amounts of toxic material.
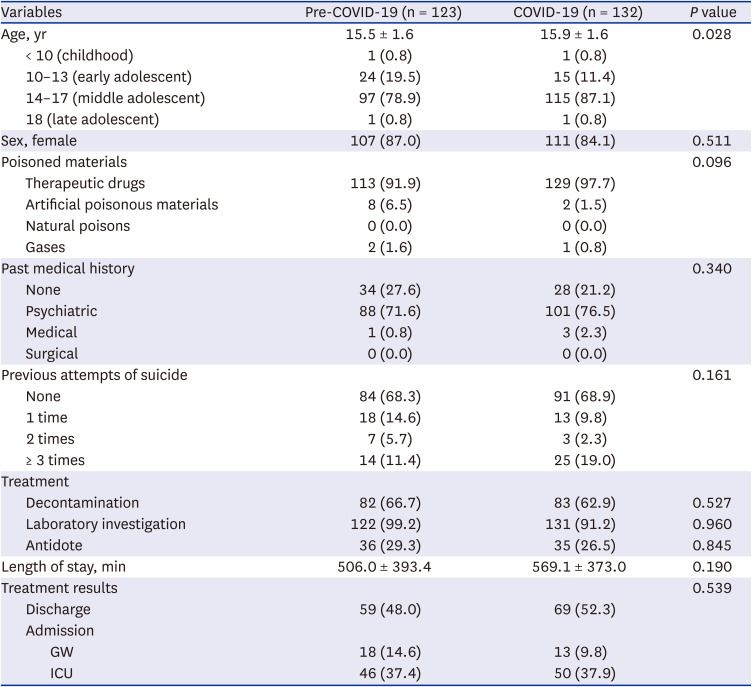
Previous studies have reported that intentional poisoning occurs mainly in adolescents aged 13–18, with more than half occurring among girls and acetaminophen, carbon monoxide, alcohol and psychiatric drugs involved in majority of the causes.
134678 The current study found similar results in both the pre- and COVID-19 groups. In particular, we observed an increase in the proportion of multi-drug poisoning. Unlike previous studies, we investigated whether patients with intentional poisonings had a history of psychiatric illnesses or past suicide attempts. However, no difference was observed between the pre- and COVID-19 groups, although more than 70% of the patients had a psychiatric illness and more than 30% had previously attempted suicide in both groups. According to studies published during the COVID-19 period, stronger social distancing protocols made it challenging for patients with an existing psychiatric illness to receive regular psychological care from specialised institutions, which increases the risk of developing psychiatric symptoms among these groups.
1718 The results presented herein showed that 19.0% of the patients in the COVID-19 group had a history of more than three suicide attempts. This suggests that adolescents with underlying psychiatric diseases may be more vulnerable to social isolation during this pandemic and can be repeatedly exposed to psychiatric emergencies, such as suicide attempts. Adolescence is an important period where individuals transition into social adults. Throughout this process of maturity, a sense of belonging and interaction with friends are absolutely necessary.
18 However, during severe social disasters, social isolation paralyses daily life, such as school and play, with fear of infection and death of a loved one potentially increasing the risk of poisoning attempts in vulnerable adolescents. Should there be a major interest in implementing quarantine policies to prevent the spread of infection at present, the results of our study may help form the basis for evaluating the impact of such policies on adolescents’ mental development and preparing supplementary measures for children with underlying mental diseases in social panic.
This study has some limitations worth noting. First, given that this study was conducted at a regional emergency centre, it does not represent the results of all children and adolescents. In addition, considering the retrospective nature of the study, some information could not be investigated, such as the amount of poisonous substances or the duration from ingestion to visitation. In the future, additional research is needed by prospectively collecting large-scale data.
In conclusion, this study confirmed an increase in the incidence of pediatric poisoning patients visiting the ED and a higher rate of intentional poisoning during the COVID-19 pandemic. Also, the frequency of adolescence and girls’ incidence increased, and the use of treatment resources and hospitalization rate increased. Many of the patients with intentional poisoning had a history of mental illness or suicide in the past. Therefore, it seems that policy consideration for mentally vulnerable adolescents during this new pandemic period are necessary.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download