This article has been
cited by other articles in ScienceCentral.
PRESENTATION OF CASE 3
Dr. Jung Wook Kim: A 81-year-old man under medication with hypertension and dyslipidemia was hospitalized with general weakness, dyspnea, and elevated blood urea nitrogen (BUN) and serum creatinine (Cr) levels. The patient had regular health check-ups, but he had never heard of abnormal renal function until the last examination, which was done 6 months ago. His prescribed agents were valsartan, rosuvastatin, and aspirin for many years. He denied alcohol abuse, smoking, or intake of herbal medications. Vital signs were stable without fever (blood pressure was 127/77 mmHg, heart rate 66 beats per minute, respiratory rate 18 breaths per minute, body temperature 36.9°C). He had no symptoms other than general weakness and dyspnea on the review of systems. Although he complained of dyspnea, physical examination revealed clear breath sounds without rales. Laboratory findings were BUN level of 74.8 mg/dL and serum Cr level of 3.92 mg/dL, spot urine protein-to-Cr ratio 1.42 g/g Cr suggesting the possibility of kidney injury. In addition, inflammatory markers, such as white blood cell count and c-reactive protein increased. Acute kidney injury (AKI) combined with infection, rather than chronic kidney disease (CKD), was highly suspected. The patient started antibiotics treatment. Chest X-ray showed emphysematous change in both lungs, suspicious of interstitial lung disease.
DIAGNOSTIC TESTS
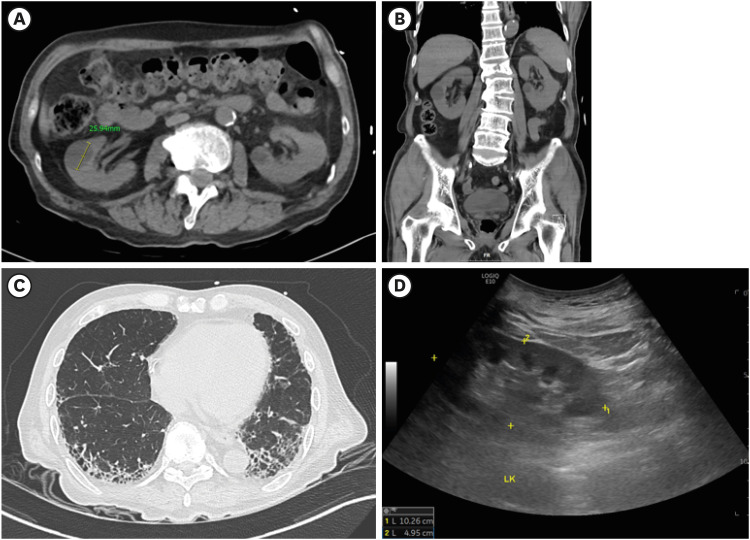
Dr. Jung Wook Kim: After admission, the patient’s inflammatory markers were not improved in spite of antibiotic treatment. For further evaluation, imaging studies were performed. There was no sign of infection on chest computed tomography (CT) or abdominopelvic CT. Kidney ultrasound suggested the possibility of AKI rather than CKD (
Fig. 1A-C). Moreover, studies suggestive of infectious diseases, such as blood culture, urinalysis, and urine culture, were all negative. Differential diagnoses of AKI, including hemorrhagic fever with renal syndrome (HFRS), rapidly progressive glomerulonephritis (RPGN), multiple myeloma (MM), and thrombotic microangiopathy (TMA) were evaluated. Despite treatments, his renal function deteriorated rapidly. He appealed uremic symptoms, such as anorexia, nausea, vomiting, and poor oral intake, and aggravation of dyspnea. On the seventh day of hospitalization, the patient-initiated hemodialysis (
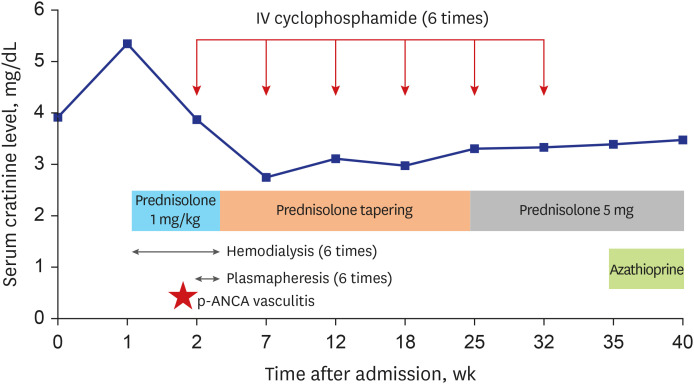
Fig. 2).
Fig. 1
Imaging studies of the patient. (A, B) Abdominopelvic CT included multiple simple cysts of both kidneys. (C) Chest CT suggested interstitial lung disease. (D) Kidney ultrasound observed normal size and parenchymal echogenicity of both kidneys.
CT = computed tomography.
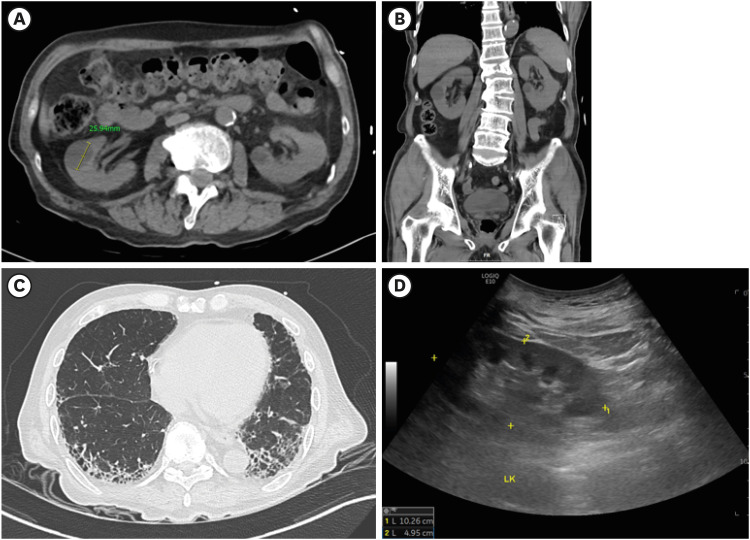
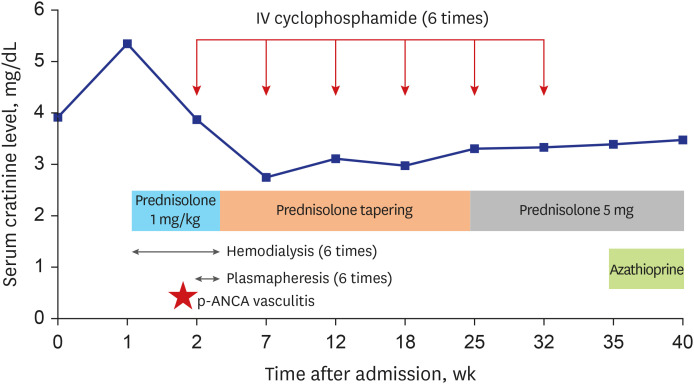
Fig. 2
Summary of treatment of the patient over time. On the 13th day after hospitalization, p-ANCA vasculitis was confirmed via kidney biopsy. As an induction treatment, the patient was treated with cyclophosphamide and plasmapheresis combined with high dose steroid. During the treatment, hemodialysis was withdrawn. Glucocorticoid was tapered for about four months. The patient was undergoing maintenance therapy with azathioprine and prednisolone.
p-ANCA = perinuclear antineutrophil cytoplasmic antibody.
Dr. Sojung Youn: Taken together, kidney biopsy was needed for a definite diagnosis. However, since he had been taking aspirin, kidney biopsy was delayed considering the bleeding risk. Meanwhile, the results for differential diagnosis of AKI were confirmed. It was found that perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) were positive (1:160), and anti-myeloperoxidase antibody titer > 134.0 IU/mL. All the other evaluations mentioned above, including those related to autoimmune diseases or both serum and urine protein electrophoreses, revealed normal results. Therefore, we implied that the cause of the diagnosis of the patient was p-ANCA-associated vasculitis with renal involvement, one of the RPGNs.
DIFFERENTIAL DIAGNOSIS OF AKI
Dr. Jung Wook Kim: If renal function is suspected to be aggravated within only a few weeks or months, it is more likely to suggest AKI rather than CKD. Kidney biopsy is required to help confirm differential diagnosis of AKI in many cases.
Dr. Sojung Youn: Due to the limitation that an early kidney biopsy could not be performed for safety reasons, we first made the following differential diagnoses based upon the available information. Based on the patient’s history and calculated results of the fractional excretion of sodium and the fractional excretion of urea, intrinsic AKI seemed to be more probable than prerenal AKI. Therefore, the differential diagnosis included the following conditions.
1 The residence and travel history suggested the possibility of HFRS, which confirmed to be negative. From old age and the laboratory findings including anemia, albumin-to-globulin ratio reversal, and significant proteinuria, light chain deposition diseases including MM were considered. His blood pressure fluctuation indicated the possibility of secondary TMA caused by malignant hypertension. As the renal function deteriorated rapidly within a few months without intake of toxic agents, RPGN was highly suspected. Nevertheless, the possibility of acute tubulointerstitial nephritis could not be ruled out as well.
Final diagnosis
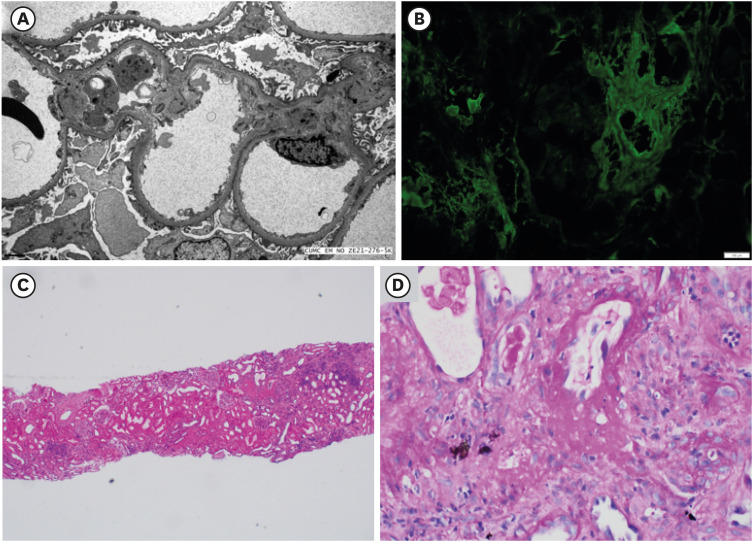
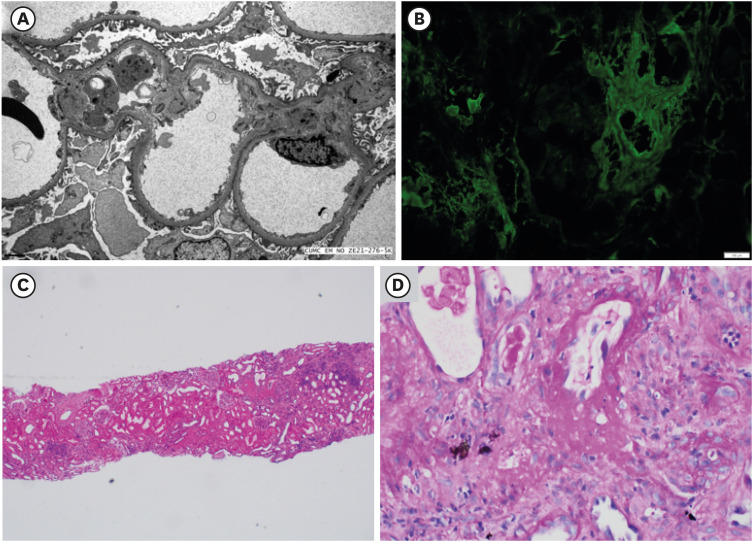
Dr. Tae Hyun Ban: After withdrawal of aspirin for a week, the patient received a kidney biopsy. First, subendothelial edema was found through electron microscopy. Immunofluorescence (IF) microscopic findings did not express any deposition, while a glomerular crescent was observed in IF study for fibrinogen. Light microscopic findings via Periodic-acid Schiff stain showed a glomerulus with crescent, glomerular sclerosis of 15.4%, and interstitial inflammation including mononuclear cell infiltration and neutrophilic infiltration, but eosinophilic infiltration was not found. In addition, fibrinoid necrosis of vessel walls was observed (
Fig. 3A-D). Considering the above results all together, we confirmed the final diagnosis of p-ANCA-associated vasculitis.
Fig. 3
Pathologic findings of kidney biopsy. (A) Subendothelial edema found through electron microscopy. (B) No evidence of deposition seen in immunofluorescence microscopic findings. Light microscopic findings via (C) Hematoxylin and eosin stain showing interstitial inflammation including mononuclear cell and neutrophilic infiltration, and (D) Periodic-acid Schiff stain showing a glomerulus with crescent and fibrinoid necrosis of vessel walls.
DISEASE MANAGEMENT
Dr. Tae Hyun Ban: Guidelines of ANCA-associated vasculitis (AAV) with kidney involvement is divided into two parts for treatment; induction therapy and maintenance therapy. A patient’s age, sex, renal function, and adherence should be considered all together to select an adequate medication for induction therapy. For those patients with AAV who are in relatively less life-threatening condition, mycophenolate mofetil is considered. In general, such a case is rare. In most cases, a majority of the patients initiate induction therapy using high dose glucocorticoids in combination with either cyclophosphamide or rituximab. For severe cases presenting as a vital organ or life-threatening condition, plasmapheresis is recommended. When the induction therapy is completed successfully, maintenance therapy is started subsequently. Glucocorticoids should be tapered over time, and the maintenance therapy combines azathioprine or rituximab with low-dose glucocorticoids.
Dr. Sojung Youn: In our case, the induction therapy was initiated with high dose glucocorticoids and intravenous cyclophosphamide. Since his serum Cr level increased rapidly with uremic symptoms, plasmapheresis was started with hemodialysis. Plasmapheresis was performed a total of six times. While his urine output and serum Cr level were well maintained during the treatment, his symptoms were relieved. On the 24th day of hospitalization, he withdrew hemodialysis. Thereafter, he received the induction therapy as six times of intravenous cyclophosphamide. Currently, he is under maintenance therapy with azathioprine and low-dose glucocorticoids.
DISCUSSION
Dr. Tae Hyun Ban: AAV is divided into 3 clinical diseases (granulomatosis with polyangiitis; microscopic polyangiitis; eosinophilic granulomatosis with polyangiitis). Classification of AAV is associated with antigens targeting proteinase 3 and myeloperoxidase. AAV has an annual incidence of 20 per million people.
23 The incidence rate increases with age and peaks at the 60–70 years.
23 Although AAV is associated with renal involvement in many cases, diagnosis should also be considered even when pulmonary, head and neck, gastrointestinal, neurologic, musculoskeletal, and even cutaneous symptoms are present. In the case of AAV with kidney involvement, kidney biopsy is needed to confirm diagnosis.
4 After the biopsy is performed, glomeruli with crescents, suggesting RPGN, were seen through light microscopic findings. However, there is no specific finding in IF images.
Dr. Eun Sil Koh: As an induction therapy for AAV with kidney involvement and vital organ or life-threatening condition, cyclophosphamide and plasmapheresis were considered in the past. However, rituximab is more widely used today. Is there any reason to consider cyclophosphamide rather than rituximab treatment for the patient?
Dr. Bum Soon Choi: The Kidney Disease Improving Global Outcomes clinical practice guideline for the management of glomerular diseases updated in 2021 recommends cyclophosphamide or rituximab for induction therapy.
4 MMF and glucocorticoids are included as well. Thus, recommended combinations of treatment are 1) MMF only, 2) cyclophosphamide + high dose glucocorticoids, and 3) rituximab + high dose glucocorticoids.
567 In addition, plasmapheresis should be considered in vital organ or life-threatening situations. Such situations include serum Cr > 5.7 mg/dL requiring dialysis, rapidly increasing serum Cr, and diffuse alveolar hemorrhage causing hypoxemia.
489 Whether to select between rituximab and cyclophosphamide as an induction agent is individualized for each patient.
4 Groups who prefer rituximab include children and adolescents, pre-menopausal women, men concerned about their fertility, and frail older adults. For patients whose serum Cr > 4 mg/dL, cyclophosphamide is rather preferred. After an induction of remission, maintenance therapy is recommended with either azathioprine or rituximab in addition to low-dose glucocorticoids.
4 The duration of maintenance therapy is known to be at least 12 months. However, an optimal duration of maintenance therapy is still unclear.
101112 Maintenance therapy with azathioprine demonstrated a reduction in both relapse rate and incidence of kidney failure, in the 4-year-treated group compared to the 12-month-treated group. However, studies on the optimal duration of maintenance therapy are scarce, and therefore more studies are needed in the future.
Prognosis
Dr. Sojung Youn: The patient was treated six times with intravenous infusions of cyclophosphamide at 1-month intervals as the induction therapy. After achievement of remission, maintenance therapy was initiated with azathioprine and low-dose glucocorticoids. The patient is remaining tolerable without any side effects. At 9 months after diagnosis of p-ANCA-associated vasculitis, his last serum Cr level was 3.47 mg/dL. His p-ANCA serology was negative for the past 6 months.
Learning points
1. Clinicians should consider ANCA-associated vasculitis for differential diagnosis when they encounter an elderly patient with abnormal renal function, who is unaware of his or her past examination results or who is suspected of sudden worsening of renal function.
2. Kidney biopsy and positive results of ANCA serology play key roles in making a diagnosis of ANCA-associated vasculitis.
3. For ANCA-associated vasculitis, glucocorticoids in combination with cyclophosphamide or rituximab are recommended as induction therapy. After induction of remission, either rituximab or azathioprine and low-dose glucocorticoids are recommended as maintenance therapy.
ACKNOWLEDGMENTS
The Case Conference section is prepared from monthly case conference of Department of Internal Medicine, the Catholic University of Korea College of Medicine, Seoul, Korea.
References
1. Zappitelli M. Epidemiology and diagnosis of acute kidney injury. Semin Nephrol. 2008; 28(5):436–446. PMID:
18790363.

2. Geetha D, Jefferson JA. ANCA-associated vasculitis: core curriculum 2020. Am J Kidney Dis. 2020; 75(1):124–137. PMID:
31358311.

3. Salvador F. ANCA associated vasculitis. Eur J Intern Med. 2020; 74:18–28. PMID:
32005600.

4. Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, et al. KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int. 2021; 100(4S):S1–S276. PMID:
34556256.
5. Jones RB, Tervaert JW, Hauser T, Luqmani R, Morgan MD, Peh CA, et al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010; 363(3):211–220. PMID:
20647198.

6. Stone JH, Merkel PA, Spiera R, Seo P, Langford CA, Hoffman GS, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010; 363(3):221–232. PMID:
20647199.

7. Jones RB, Hiemstra TF, Ballarin J, Blockmans DE, Brogan P, Bruchfeld A, et al. Mycophenolate mofetil versus cyclophosphamide for remission induction in ANCA-associated vasculitis: a randomised, non-inferiority trial. Ann Rheum Dis. 2019; 78(3):399–405. PMID:
30612116.

8. Jayne DR, Gaskin G, Rasmussen N, Abramowicz D, Ferrario F, Guillevin L, et al. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. J Am Soc Nephrol. 2007; 18(7):2180–2188. PMID:
17582159.

9. Walsh M, Merkel PA, Peh CA, Szpirt W, Guillevin L, Pusey CD, et al. Plasma exchange and glucocorticoid dosing in the treatment of anti-neutrophil cytoplasm antibody associated vasculitis (PEXIVAS): protocol for a randomized controlled trial. Trials. 2013; 14(1):73. PMID:
23497590.

10. Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaître O, Cohen P, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014; 371(19):1771–1780. PMID:
25372085.
11. Karras A, Pagnoux C, Haubitz M, Groot K, Puechal X, Tervaert JW, et al. Randomised controlled trial of prolonged treatment in the remission phase of ANCA-associated vasculitis. Ann Rheum Dis. 2017; 76(10):1662–1668. PMID:
28546260.
12. Charles P, Terrier B, Perrodeau É, Cohen P, Faguer S, Huart A, et al. Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann Rheum Dis. 2018; 77(8):1143–1149. PMID:
29695500.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download