This article has been
cited by other articles in ScienceCentral.
Abstract
On 22 June, a man who returned to South Korea from Germany tested positive for the monkeypox virus using real-time polymerase chain reaction. We identified 49 contacts concerning the first monkeypox case and classified them into two groups based on risk exposure levels. Through active monitoring of eight people in the medium-risk group and passive monitoring of 41 people in the low-risk group, we identified that no secondary transmission occurred over 21 days. The prompt active or passive monitoring of the index case of imported monkeypox could prevent community transmission in Korea.
Keywords: Monkeypox, MPX, Monkeypox Virus
Monkeypox (MPX), a zoonotic disease in which human-to-human transmission is limited, can occur through direct contact with a skin lesion of an infected person, prolonged exposure to respiratory droplets, or surfaces contaminated by the MPX virus.
123 The abrupt increase in MPX cases was first reported in Europe in May 2022, followed by unprecedented outbreaks in other non-endemic areas.
14 As per the evolving global situation, South Korea has reinforced surveillance at ports and communities to prepare a rapid response to the first outbreak of MPX.
5
On June 21, 2022, a 34-year-old man arrived at the Incheon International Airport, South Korea, from Germany. After immigration, he became aware at the airport lobby that his German male friend had received a diagnostic test as a suspicious MPX case at a hospital in Germany.
6 As soon as he heard the news, he called the Korea Disease Control and Prevention Agency (KDCA) call center for a consultation which was immediately forwarded to the MPX response team in KDCA and Incheon Airport National Quarantine Station (IANQS). The officer at the airport quarantine station promptly called him for a rapid investigation, including looking for current symptoms and epidemiological links, and then he was isolated at IANQS.
In an in-depth epidemiological investigation, he stated that he had experienced a headache 3 days before returning to South Korea and, on arrival, developed a sore throat, malaise, fatigue, and skin lesions, with a body temperature of 37.0°C.
67 His travel history involved June 1 to 21, 2022, in Germany, and he stayed with the German male friend from June 1 to 14. Based on the information found, we classified him as a suspected MPX case with suspicion of relevance to the current global MPX outbreak. Accordingly, we sent him to a state-designated hospital via ambulance for examinations.
On clinical assessment, lesions in scabbing form were found on his lips, and small papules were spread over his back and lower trunk in front. In addition, a painless and umbilicated genital lesion was observed at the one-third distal end of the penis.
6 Specimens collected from the penile ulcer, oropharynx and nasopharynx were tested using real-time polymerase chain reaction (PCR) and resulted positive on the following day.
6 The confirmation of the first MPX case led to a response by KDCA of contact tracing in collaboration with IANQS, and we assessed exposure risk to determine monitoring methods for the contacts.
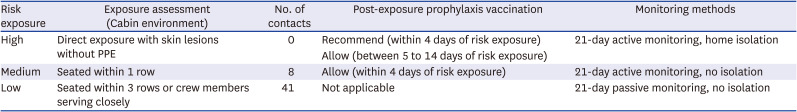
From passengers on the same flight, we identified 49 persons as contacts of the confirmed case based on the MPX response guideline (
Fig. 1).
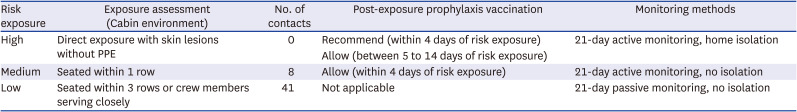
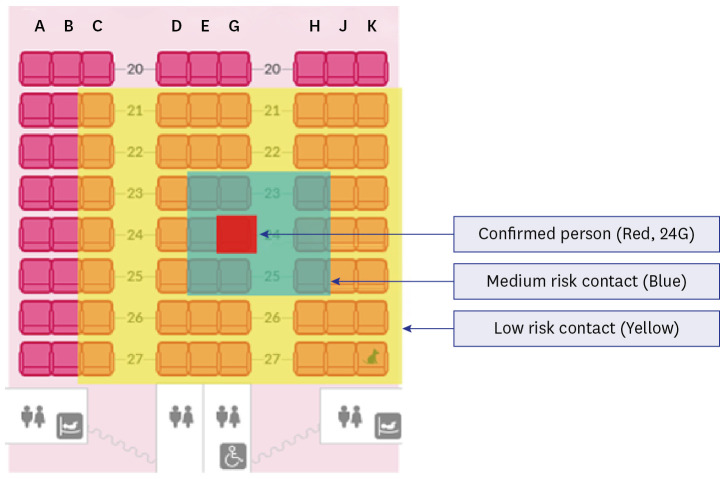
8 We classified 8 persons as the medium-risk group (passengers seated within one row from the confirmed case) and 41 persons as the low-risk group (passengers seated within 3 rows from the confirmed case and crew providing close services to the confirmed case). However, no passengers were assessed in the high-risk group (
Table 1). For additional identification of contacts at the airport, CCTV footage was collected as objective evidence; however, more contacts were not identified.
We notified each public health center of the list of contacts for day-to-day management based on the residential address of the contacts. We applied active monitoring for the medium-risk group involving twice-daily telephone communication for 21 days after the last exposure to the confirmed case, without quarantine. Simultaneously, the low-risk group was under passive surveillance by self-screening for symptoms such as fever, lymphadenopathy, rash, and other relevant symptoms for 21 days without quarantine.
In addition, we recommended that the 8 persons in the medium-risk group comply with prevention measures; to limit contact with immunocompromised people, pregnant women, and children under the age of 6; and to immediately report any symptoms. Furthermore, we informed them about Post-exposure prophylaxis with a second-generation smallpox vaccine
7; however, none of them accepted a vaccination.
9
One person in the medium-risk group developed symptoms during active monitoring. She sought an emergency department, suspecting MPX with complaints of fever (37.9°C) and feeling heavy in the chest. She tested negative in PCR for COVID-19 and showed normal ranges in blood tests. One day after, she had recurring subjective fever, headache, and nausea; however, symptoms were soon alleviated, and no other symptoms, including rash, were observed. We ruled out MPX through a case re-assessment, and she remained in the same risk group.
By July 11, the end of the 21-day monitoring period, there was no report of clinical symptoms indicating MPX among the contacts, and the outbreak ended. In this outbreak, we concluded that secondary transmission did not occur where susceptible people were exposed to a symptomatic MPX case in the cabin environment with adequate personal protection such as wearing masks. Finally, the first MPX case received treatments to alleviate symptoms and was released from isolation after recovery.
10
In conclusion, it is worth noting that prevention of community transmission was achieved beforehand by taking prompt public health measures given a voluntary report of the confirmed patient at the airport. It implies the importance of increasing awareness of MPX and promoting appropriate action to be taken by individuals when suspecting relevant symptoms.
Ethics statement
The study was conducted as a legally obligated public health investigation by the Korea Disease Control and Prevention Agency (KDCA), given authority under Article 18 of the Korean Infectious Disease Prevention Act (No. 18893). The study was reviewed and approved by the Institutional Review Board of the Korea Disease Control and Prevention Agency and the requirement for informed consent was waived (Approval No. 2022-09-08-PE-A).
Fig. 1
The aircraft sitting arrangement of confirmed case and the contacts.
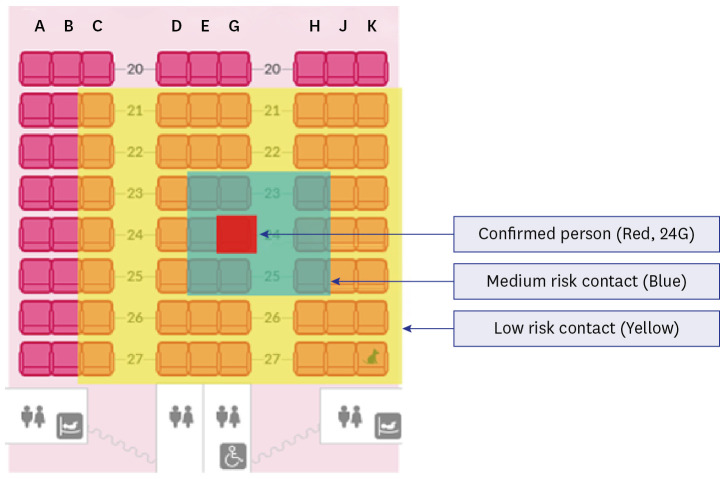
Table 1
Management guidelines and characteristics of contacts of the first monkeypox case
|
Risk exposure |
Exposure assessment (Cabin environment) |
No. of contacts |
Post-exposure prophylaxis vaccination |
Monitoring methods |
|
High |
Direct exposure with skin lesions without PPE |
0 |
Recommend (within 4 days of risk exposure) |
21-day active monitoring, home isolation |
|
Allow (between 5 to 14 days of risk exposure) |
|
Medium |
Seated within 1 row |
8 |
Allow (within 4 days of risk exposure) |
21-day active monitoring, no isolation |
|
Low |
Seated within 3 rows or crew members serving closely |
41 |
Not applicable |
21-day passive monitoring, no isolation |




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download