INTRODUCTION
Clinical manifestations of coronavirus disease 2019 (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, vary in adults and children.
12 In pediatric patients, COVID-19 usually presents with a fever and cough.
1
Croup is a common upper airway infection characterized by a “barking cough,” stridor, and hoarseness.
34 It is usually caused by viral infections (most commonly parainfluenza) and is generally a mild condition with a low mortality rate in children.
34
To the best of our knowledge, severe croup requiring cardiopulmonary resuscitation (CPR) has not been reported in omicron BA.2 variant patients. We report two cases of life-threatening croup that required intubation and CPR caused by the SARS-CoV-2 omicron BA.2 variant in previously healthy children.
CASE DESCRIPTION
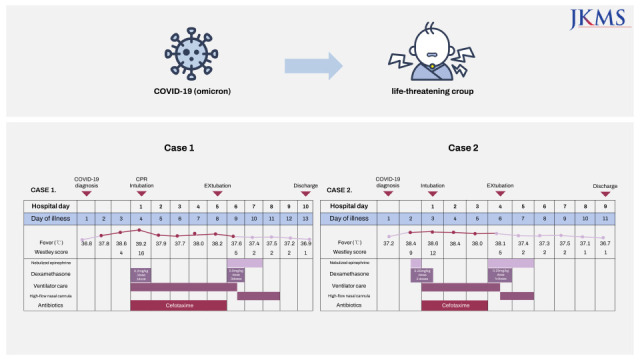
Case 1
In March 2022, a 9-month-old female who had previously been healthy visited the local hospital due to a fever, barking cough, and chest retraction for the past one day. She and her parents had been diagnosed with COVID-19 three days prior. At a local hospital, she was diagnosed with croup and received nebulized normal saline and intramuscular dexamethasone (0.2 mg/kg/dose). Approximately 4 hours later, the patient developed cyanosis, which was immediately followed by cardiac arrest due to respiratory failure. CPR was performed for two minutes, after which spontaneous circulation was restored. She was directly transferred to our emergency department (ED). Upon ED arrival, her percutaneous oxygen saturation (SpO2) was 100% with 5 L/min of oxygen delivered via a facial mask. Her blood pressure was 90/60 mmHg, and her pulse rate was 180 beats/minute. The patient’s respiratory rate was 47 breaths/minute, and her body temperature was 38°C. Her mental status was drowsy. Her height was 70.4 cm (10–25th percentile), and her weight was 7.6 kg (10th percentile). A physical examination showed notable stridor, severe chest retraction, and markedly decreased aeration at rest (Westley croup score of 16). Intubation was carried out with a size 3.5 uncuffed endotracheal tube for acute respiratory failure, and direct laryngoscopy revealed no evidence of epiglottitis. She was admitted to a negative-pressure room in the pediatric intensive care unit (PICU) and was treated with mechanical ventilation and cefotaxime administration for five days.
The initial polymerase chain reaction (PCR) test for respiratory viruses (Allplex Respiratory Panel 1/2/3; Seegene, Seoul, Korea) and SARS-CoV-2 assay (Allplex SARS-CoV-2 Assay; Seegene) was performed with a nasopharyngeal swab (eNAT; Copan Diagnostics, Brescia, Italy) and was only positive for SARS-CoV-2; no other respiratory viruses were identified. The omicron sublineage BA.2 variant (Stealth omicron) was identified by a PowerChek™ SARS-CoV-2 S-gene Mutation Detection Kit, Ver. 3.0 (Kogenebiotech, Seoul, Korea). The initial laboratory findings were as follows: white blood cell count: 13,300/μL, hemoglobin: 11.2 g/dL, platelet count: 208,000/μL, and C-reactive protein: 10.67 mg/L (range: 0–5). Electrolytes, renal function, liver function, cardiac enzymes, and lactic acid levels were within the normal ranges. An arterial blood gas analysis revealed a pH of 7.11, a pCO2 of 69.8 mmHg, a pO2 of 296 mmHg, and an HCO3 of 22.5 mmol/L with 5 L/min of oxygen administered via a facial mask. A chest X-ray was clear without consolidation in both lung fields. Electrocardiography showed sinus tachycardia, and echocardiography revealed a normal cardiac ejection fraction. Blood cultures were negative.
Extubation was successful after five days of endotracheal intubation with intravenous dexamethasone administration (0.5 mg/kg) and nebulized racemic epinephrine (NRE). After extubation, she required a high-flow nasal cannula (HFNC) and NRE for two additional days for stridor and mild chest retraction with agitation. Medical teams used personal protective equipment including N95 mask, gown, latex gloves, and face shield. On the 10th day of admission, the patient was discharged in good general condition without any neurologic sequelae.
Case 2
In March 2022, a previously healthy 11-month-old male manifested a fever, a barking cough, chest retraction, and cyanosis. He and his parents had been diagnosed with COVID-19 two days before his admission. He was given NRE and intramuscular dexamethasone (0.25 mg/kg/dose) for croup at the ED and developed lethargy despite repeated NRE. The patient was subsequently transferred to our ED due to airway concerns. Upon arrival at our ED, his SpO2 was 85% on 5 L/min of oxygen via nasal prongs; his blood pressure was 103/58 mmHg, and his pulse rate was 205 beats/minute. The patient’s respiratory rate was 49 breaths/minute, his body temperature was 38°C, and the Westley croup score was 12 points. His height was 80 cm (90–95th percentile), while his weight was 11 kg (75–90th percentile). He was intubated with a size 4.0 uncuffed endotracheal tube for acute respiratory failure and was admitted to the PICU. The epiglottis showed normal findings upon direct laryngoscopy. A respiratory viral PCR panel obtained via a nasopharyngeal swab was positive only for SARS-CoV-2, and the omicron sublineage BA.2 was identified. Chest radiographs showed normal findings.
On the fourth day after admission, the patient was extubated with the administration of intravenous dexamethasone (0.25 mg/kg) and NRE. After extubation, he was given HFNC and NRE for one more day for stridor with agitation. On the ninth day after admission, he was discharged and doing well without any complications.
Ethics statement
The Institutional Review Board (IRB) of Jeonbuk National University Hospital approved this study (IRB No. 2022-04-011). The requirement of informed consent for publishing was renounced.
DISCUSSION
To the best of our knowledge, this is the first report of life-threatening croup resulting from the omicron BA.2 variant and confirmed by reverse transcription polymerase chain reaction (RT-PCR) in pediatric patients. Our patients developed acute respiratory failure that was unresponsive to dexamethasone and multiple NRE treatments. They were treated with mechanical ventilation, dexamethasone, and NRE in the PICU. Their intubation durations were 112 hours and 80 hours, respectively. Our patients were discharged without complications.
Croup, also known as acute laryngotracheobronchitis, is characterized by the sudden onset of a barking cough that is usually accompanied by inspiratory stridor, hoarseness, and respiratory distress as a result of upper airway obstruction.
34 Symptom onset is usually sudden and most often occurs at night.
34 Croup is typically caused by viral infections, and parainfluenza is the most commonly responsible pathogen.
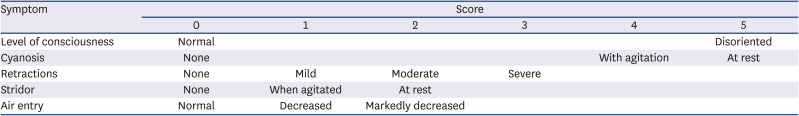
34 The diagnosis is mainly clinical; the Westley score, which is based on a history and physical examination, is widely used to evaluate the severity of croup (
Table 1).
3456 Croup usually resolves within 48 hours, but severe croup rarely may lead to acute respiratory failure and respiratory arrest.
7 Of those admitted with croup, < 3% require intubation.
34 Dexamethasone should be administered to all patients with croup of any severity, and NRE is recommended for moderate to severe croup.
36
Table 1
The Westley croup score
|
Symptom |
Score |
|
0 |
1 |
2 |
3 |
4 |
5 |
|
Level of consciousness |
Normal |
|
|
|
|
Disoriented |
|
Cyanosis |
None |
|
|
|
With agitation |
At rest |
|
Retractions |
None |
Mild |
Moderate |
Severe |
|
|
|
Stridor |
None |
When agitated |
At rest |
|
|
|
|
Air entry |
Normal |
Decreased |
Markedly decreased |
|
|
|
The initial outbreak of COVID-19, which is caused by the SARS-CoV-2 virus, first occurred in December 2019.
18 In contrast with adults, children typically experience milder clinical courses with this disease.
12 The clinical findings of COVID-19 in children are diverse, and the most common reported symptoms are fever and cough.
1 While pediatric patients often require close observation or symptomatic treatment, only a few children require intensive care for COVID-19.
2 During the COVID-19 pandemic, the infectivity, virulence, and clinical manifestations of novel variants of SARS-CoV-2 have been dynamic and unique.
9 The SARS-CoV-2 omicron variant became dominant during early 2022.
10 Before the omicron variant surge, few cases of croup caused by COVID-19 were reported in children.
111213141516 Previously reported cases indicate that COVID-19-associated croup can be treated in the same manner as other viral causes of croup.
11131516 In two cases, endotracheal intubation was performed due to secondary bacterial tracheitis and multisystem inflammatory syndrome in children.
1214 Three retrospective analyses of COVID-19-associated croup have demonstrated that the incidence of croup significantly increased during periods where the omicron variant was circulating.
91718
To the best of our knowledge, there have been no case reports of life-threatening croup induced by the omicron variant and confirmed by RT-PCR during the omicron variant surge. In our case 1, a barking cough and chest retraction occurred at night on the third day of her COVID-19 home isolation, and she visited the hospital the next morning. Although dexamethasone was administered at the local hospital, respiratory difficulty and cardiac arrest still occurred. Case 2 presented with a barking cough, chest retraction, and cyanosis at night on the second day of his COVID-19 home isolation, and he visited the ED. Although dexamethasone and repeated NRE were administered, the patient’s respiratory difficulty was aggravated, and he was intubated. Both patients were treated with invasive ventilation, dexamethasone, and NRE and were later discharged without complications. Brewster et al.
9 reported that the observed rates of hospitalization and re-dosing of croup treatments in COVID-19-associated croup might be due to more severe manifestations than croup caused by other viruses. Also, Tunç et al.
17 and Choi et al.
18 found that croup patients were more likely to receive NRE during the omicron variant surge, which suggests that the early symptoms of croup with omicron are more severe than they were during the Delta variant surge. But no patients required invasive ventilation or died.
918 In three retrospective studies, the COVID-19 variant and the omicron subtype were not identified.
91718 However, in our cases, a COVID-19 variant analysis was performed, and omicron sublineage BA.2 variants (Stealth omicron) were identified. Lyngse et al.
10 found that BA.2 was substantially more transmissible than BA.1. However, there are no data thus far to suggest that BA.2 leads to more severe disease than previous omicron subvariants. Therefore, it is difficult to say that the omicron BA.2 variant was the cause of severe croup in our patients. It is important to monitor novel variants of SARS-CoV-2 during the COVID-19 pandemic.
19 In addition, children with existing underlying diseases are most likely to show manifestations of severe COVID-19.
20 However, our case report suggests the possibility that serious illness can result from COVID-19 croup even in children without underlying diseases.
Our limited experience with COVID-19 croup requiring endotracheal intubation and CPR suggests that the SARS-CoV-2 variant may cause severe croup that may not be improved by conventional treatment, especially for the omicron BA.2 variant. We recommend that infants presenting with COVID-19 croup receive a timely diagnosis and prompt intervention. Additionally, if symptoms of croup develop in pediatric patients during the COVID-19 pandemic, their parents must bring them to the hospital immediately. Further research is needed to identify the pathophysiology of COVID-19 croup compared to other types of viral croup.