This article has been
cited by other articles in ScienceCentral.
PRESENTATION OF CASE 1
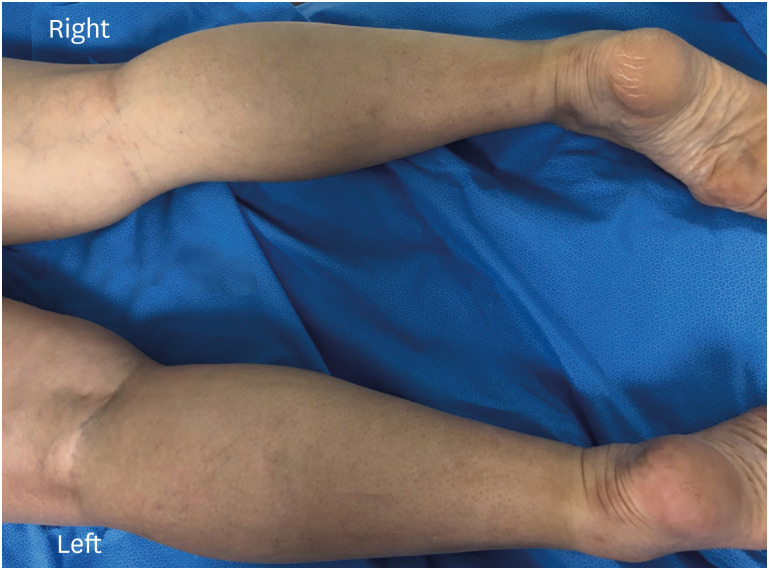
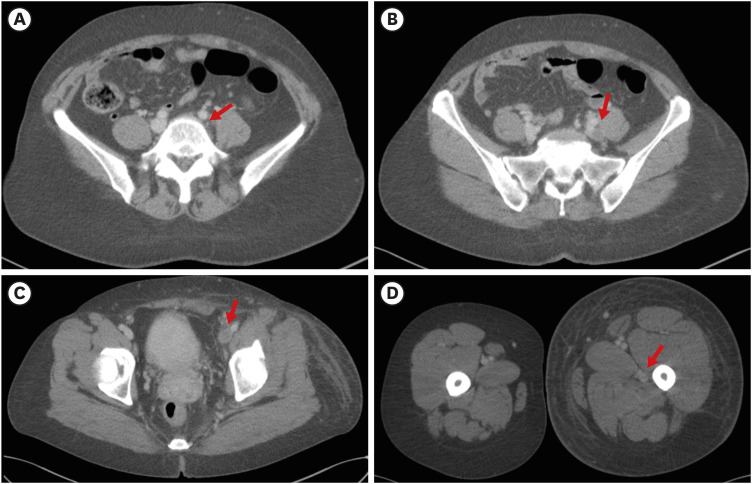
Dr. Myunhee Lee: A 44-year-old woman with no previous medical history presented with painful, gradually worsening left leg swelling for two weeks. She denied smoking, drinking alcohol, oral contraceptive use, or illicit drug use. She had no history of recent surgery, trauma, or travel leading to prolonged immobilization. She had no complaints of sexual intercourse. She had no abdominal or hip pain. On physical examination, she was afebrile and vital signs were stable (the temperature was 36.6°C, the blood pressure 122/62 mmHg, the pulse 66 beats per minute, the respiratory rate 16 breaths per minute, and the oxygen saturation 98% while the patient was breathing ambient air). The body weight was 65 kg with a body-mass index of 26.7. Both lungs were clear. The heart sounds were normal, without murmurs. Her left lower extremity from the ankle to thigh was swollen and tender with mild erythematous change but without any skin lesion (
Fig. 1). She had no swollen or palpable lymph node in groin area. Other examinations were unremarkable. Both femoral and distal pulses, motor strength, and sensations were intact. Laboratory tests, including complete blood count, complete metabolic panel, and urinalysis, were unremarkable except for an elevated D-dimer level (4.34 mg/L FEU). Antiphospholipid syndrome was ruled out as anticardiolipin antibodies, and lupus anticoagulants were normal. Coagulopathy panels including protein S, protein C, and factor V laden were within reference ranges, and thrombophilia tests were negative. An electrocardiogram showed sinus rhythm. Chest radiograph showed clear lungs and normal cardiac and mediastinal silhouette.
Fig. 1
Photograph of the patient’s lower extremity (prone position). Despite anticoagulation therapy, the patient’s left whole lower extremity shows diffuse swelling with mild erythema.
DIAGNOSTIC TESTS
Dr. Myunhee Lee: Considering the patient’s age, physical examinations, laboratory findings, and absence of other signs of infection, unilateral deep vein thrombosis (DVT) of the left lower extremity was strongly suspected.
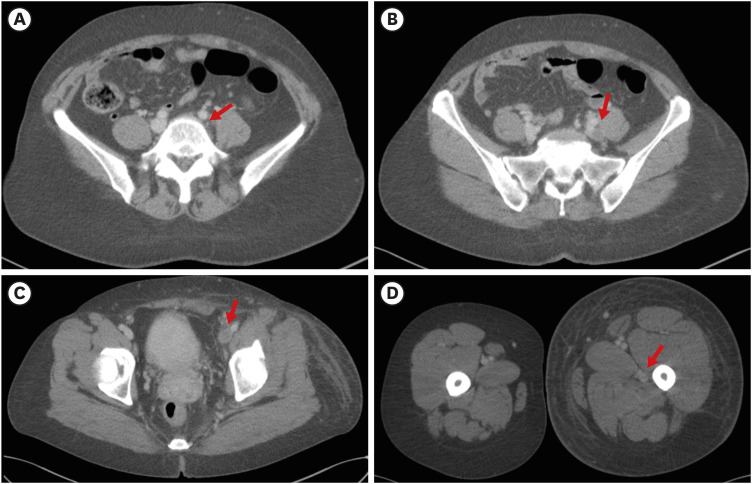
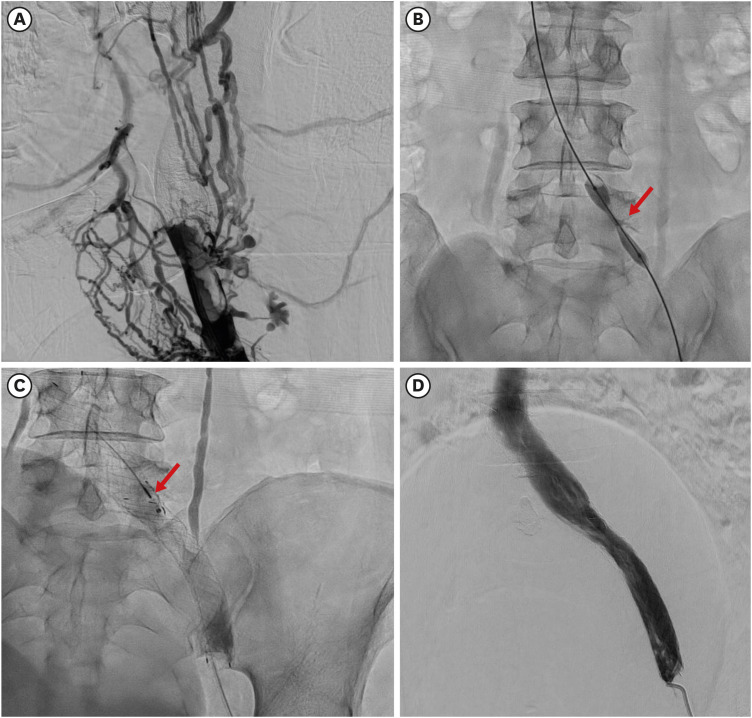
Dr. Mahn-Won Park: Non-invasive imaging such as duplex ultrasound, computed tomography (CT) angiography, or MR venography can detect DVT and identify vascular lesions or other anatomic variants. In this patient, CT angiography was ordered because it is highly sensitive and specific to find out the location and extent of DVT along with the causes of extrinsic vein compression. After 1-week of oral anticoagulation therapy with rivaroxaban, CT angiography revealed the left common iliac vein was externally compressed between the right common iliac artery and spinal body (
Fig. 2A), resulting in complete occlusion of the iliac vein with extensive DVT involving the left iliac vein, and femoral vein, and popliteal vein (
Fig. 2B–D).
Fig. 2
Initial CT of lower extremity. CT scan shows that the left iliac vein is externally compressed (arrow) between the right common iliac artery and spinal body (A), resulting in complete occlusion of the left iliac vein (B) with extensive thrombus (arrows) involving the left iliac vein (B), left femoral vein (C), and left popliteal vein (D). The patient’s left lower extremity exhibits marked swelling.
(B, C, D) Arrows indicate thrombus in the left iliac, left femoral, and left popliteal vein, respectively.
CT = computed tomography.
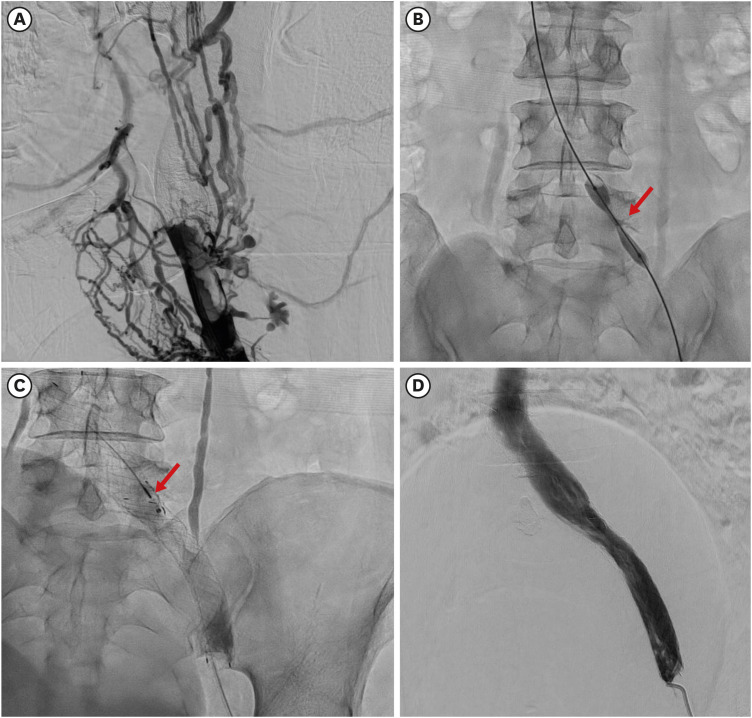
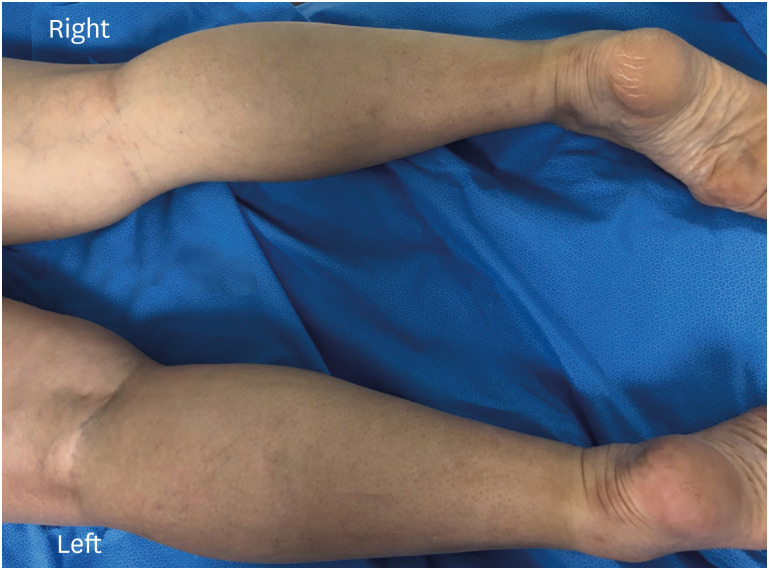
Dr. Mahn-Won Park: Catheter-based venography by a left popliteal venous approach under sonography guidance showed multiple large thrombi and complete thrombotic occlusion of the left iliac and common femoral vein with extensive pelvic venous collaterals (
Fig. 3A).
Fig. 3
Venography shows (A) the multiple large thrombi and complete occlusion of the left iliac and common femoral vein with extensive venous collaterals. (B) After advancing a guidewire into the inferior vena cava, balloon angioplasty showed a “waist” in the balloon (arrow) at the site of left common iliac vein compression by the right common iliac artery and spinal body. (C) Following balloon angioplasty, stents were implanted from the left common iliac vein to the femoral vein. Because post-stent venography revealed significant residual thrombi in the stent lumen, catheter-directed thrombolysis with alteplase (arrow) was performed. (D) The following day, venography shows well-positioned, patent stents and restored flow from the femoral vein to the inferior vena cava.
DIFFERENTIAL DIAGNOSIS OF LEG EDEMA
Dr. Myunhee Lee: This previously healthy 42-year-old woman presented with painful leg edema. The notable feature of this patient was that the patient complained of unilateral swelling of the leg without any provocative factors. The most likely diagnosis is DVT, but we need to focus on finding out the etiology of DVT because it is crucial to make an optimal treatment strategy and prevent the recurrence of DVT.
Systemic causes
Dr. Young Kyung Sa: The differential diagnosis of leg edema includes systemic illnesses such as heart failure, kidney disease, liver disease, and thyroid disorder. However, these could be ruled out based on clinical presentation (e.g., unilateral leg edema) and initial laboratory findings.
DVT with extrinsic venous compression
Dr. Young Kyung Sa: Extrinsic venous compression can also lead to unilateral leg edema. Possible causes of vein compression include pelvic mass (e.g., tumor, abscess, or hematoma), aortoiliac aneurysm, uterine enlargement, retroperitoneal fibrosis, or osteophyte. May-Thurner syndrome (MTS) is a specific form of extrinsic compression of the left iliac vein between the overlying right common iliac artery and the lumbar vertebrae, leading to venous outflow obstruction and increasing the risk of DVT. MTS should be suspected as the possible reason for acute onset unilateral DVT, especially in younger female patients.
Other-vascular causes of unilateral leg swelling
Dr. Young Kyung Sa: Unilateral leg swelling is also a feature of peripheral lymphedema or venous insufficiency. Thorough history takings and physical examination are required to distinguish these conditions. Lymphedema results from damage or an impaired flow in the lymphatic system, most caused by the removal of or damage to lymph nodes as a part of cancer treatment. Chronic venous insufficiency results from venous hypertension, mainly due to damaged valves and reflux. Risk factors for venous insufficiency include old age, obesity, pregnancy, trauma, and prolonged standing.
Final diagnosis
Dr. Myunhee Lee: Based on the CT angiography and venography findings, the final diagnosis of thrombotic MTS was made.
DISEASE MANAGEMENT
Dr. Mahn-Won Park: Most patients with MTS are asymptomatic. When symptomatic, it leads to painful, unilateral leg swelling, DVT, and pulmonary embolism (PE); therefore, it should be treated. The decision of treatment strategy depends on symptom severity and the presence of DVT. The goals of symptomatic MTS treatment are to resolve the obstruction of iliac venous outflow tract and prevent post-thrombotic syndrome (PTS). Anticoagulation with compression stocking is sufficient in patients with non-thrombotic MTS with mild symptoms. However, in patients with thrombotic MTS with moderate-severe symptoms, endovascular intervention, including angioplasty followed by stenting with or without thrombolysis, is considered a safer and more effective therapy than conventional therapy to prevent recurrent DVT and PTS.
12 Angioplasty alone is not sufficient and is associated with high recurrence rates.
3 Recently, subsequent systemic review and meta-analyses have consistently demonstrated that endovascular intervention showed an excellent success rate (94.5% to 99.6%) and reasonable long-term patency rate (at 1 year: 73.4% to 98%, at 2 years: 60% to 100%, at 5 years: 94%).
12 Balloon angioplasty followed by stenting (preferably self-expanding stent) with post-balloon dilatation (if needed) is beneficial to prevent DVT and PTS by correcting stent under-expansion.
124 Following the successful intervention, long-term anticoagulation for at least 6 months should be continued as recommended by venous thromboembolism guidelines.
56 Concurrent antiplatelet therapy, such as aspirin or clopidogrel, is reasonable after stent implantation. However, still, there is a lack of evidence of optimal combination or duration of antiplatelet therapy after the endovascular intervention.
Dr. Myunhee Lee: When balloon angioplasty was performed at the left common iliac vein, there was a “waist” in the balloon at the site of external compression (
Fig. 3B). Following balloon angioplasty, stents implantation was done from the left iliac vein to the inferior vena cava (IVC) (
Fig. 3C). Because post-stent venography revealed significant residual thrombi along the course of the stents and the left common femoral vein, the patient underwent catheter-directed thrombolysis with alteplase 0.5 mg/hr infusion for 24 hours. The next day, follow-up venography revealed well-positioned, patent left iliac vein stents with mild residual thrombus and restored flow from the iliofemoral vein to the IVC (
Fig. 3D). Post-operatively, the patient was continued on intravenous heparin drip titrated to an activated prothrombin time of 50–70 seconds for 48 hours, then was initiated on aspirin 100 mg plus clopidogrel 75 mg once daily, and oral anticoagulation with rivaroxaban 15 mg twice a day. On day 3 after the procedure, the patient’s symptoms and leg edema were entirely resolved, and the patient was discharged.
DISCUSSION
Dr. Mahn-Won Park: MTS was first described in 1957 when May and Thurner studied 430 cadavers and found that 22% of cadavers exhibited intimal vascular thickening (called a “Spur”) at the site of which the left common iliac vein was externally compressed by the right common iliac artery against the lumbar spine.
7 MTS, also known as iliac vein compression syndrome, Cockett’s syndrome, is responsible for only 2–5% of all cases of DVT.
8 However, clinicians should consider MTS for the differential diagnosis when younger female patients are presented with unilateral (more frequently, left) lower extremity swelling or recurrent DVTs, especially if the patient has no apparent causes. In 1995, Berger et al.
9 first reported that they successfully treated MTS patients with endovascular treatment using a venous stent. Since then, with the advancement of device technology and procedure skills, endovascular treatment of MTS has been increasing and is considered a safe and effective treatment for symptomatic thrombotic MTS patients with favorable long-term outcomes.
12
Role of IVC filter
Dr. Young Kyung Sa: Some physicians suggested that IVC filter placement is beneficial for preventing PE, especially in patients with extensive DVT. What do you think about the role of the IVC filter in MTS patients?
Dr. Myunhee Lee: Thank you for your precious comment. The effectiveness of IVS filter placement is questionable in managing DVT, including in MTS patients. The previous report showed that the prevalence of PE in patients with MTS is rare; the authors stated that venous spurs in the narrowing vessel afford protection against migration of thrombus into IVC.
10 IVC filters also have some downsides to be considered. IVC filter itself is a large foreign body. Therefore, it may lead to further DVT around the filter. Large or multiple small clots in the filter can make it harder for blood to move to the heart. For these reasons, the filter should be removed after sufficient anticoagulation therapy. So, current guidelines do not recommend prophylactic placement of IVC filter, given its potential side effects.
56 Guidelines state that IVC filter should be reserved only for patients who cannot tolerate anticoagulation because of bleeding.
56
Long-term medical management
Dr. Young Kyung Sa: After endovascular venous stent placement, how long anticoagulation therapy is needed, and what kinds of antiplatelet therapy are recommended?
Dr. Myunhee Lee: Once the venous stent is placed, anticoagulation with vitamin K antagonist (warfarin) or novel oral anticoagulants is recommended for at least 3–6 months, same as other DVT management protocols.
56 However, the optimal choice and duration of antiplatelet therapy following venous stent deployment is unknown because there are limited data about venous stents. Generally, single antiplatelet therapy (e.g., aspirin 100 mg daily) after 1 month of dual antiplatelet therapy such as aspirin and clopidogrel (if patients do not have high bleeding risk) along with 3–6 months of anticoagulation is widely used in clinical practice.
Prognosis
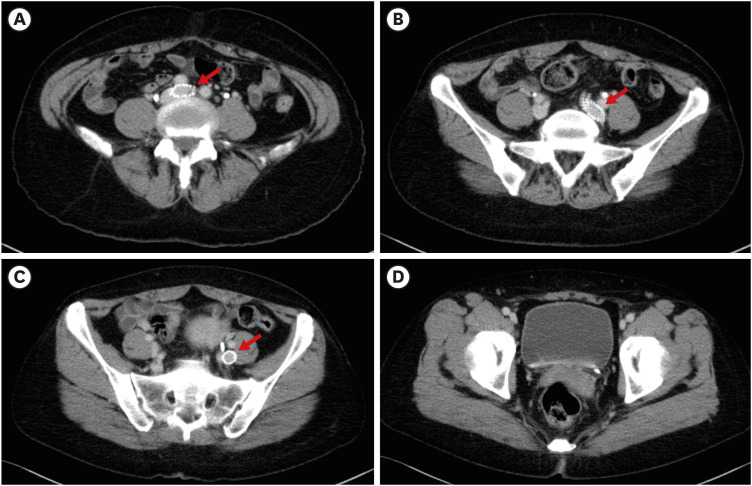
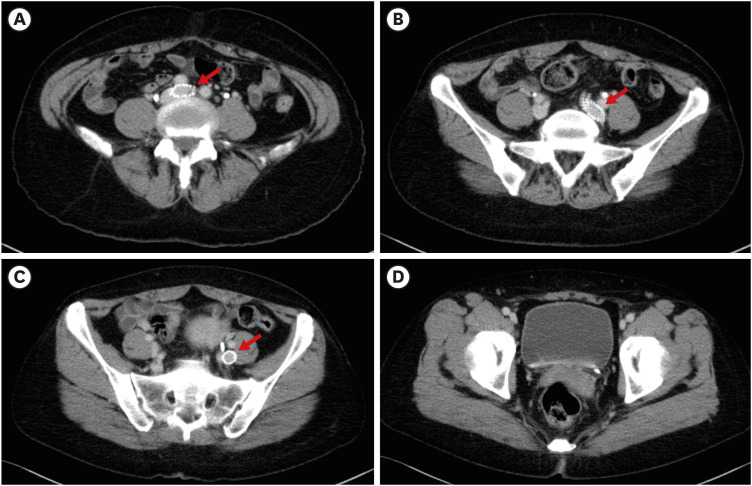
Dr. Myunhee Lee: In this case, at 6-months after the endovascular intervention and anticoagulation therapy, follow-up CT showed complete resolution of DVT in the entire left lower extremity and well-positioned iliac vein stents without stenosis (
Fig. 4A-D). After stopping anticoagulation, the patient is taking aspirin 100 mg daily and has remained symptom-free for 2 years.
Fig. 4
The follow-up CT of the lower extremity at 6-months after endovascular intervention. CT shows complete resolution of thrombus in the entire left lower extremity and well-positioned vein stents (arrows in A, B, and C) without stenosis.
CT = computed tomography.
Learning points
1. Clinicians should consider MTS for their differential diagnosis when the patient is presented with unexplained lower limb swelling or with extensive left lower limb DVT.
2. CT angiography or venography is the gold standard for diagnosing MTS. It can identify stenotic lesions, thrombus burden, or causes of extrinsic venous compression.
3. Conservative management with compression stockings and pharmacotherapy with anticoagulation is recommended for mild non-thrombotic MTS patients. However, in thrombotic MTS patients with severe symptoms, endovascular treatment, including percutaneous balloon angioplasty and stenting combined with catheter-directed thrombolysis, is safe and effective in alleviating symptoms and preventing the recurrence of DVT.
ACKNOWLEDGMENT
The Case Conference section is prepared from monthly case conference of Department of Internal Medicine, the Catholic University of Korea College of Medicine, Seoul, Korea.
References
1. Rodrigues LD, Bertanha M, El Dib R, Moura R. Association between deep vein thrombosis and stent patency in symptomatic iliac vein compression syndrome: Systematic review and meta-analysis. J Vasc Surg Venous Lymphat Disord. 2021; 9(1):275–284. PMID:
32827731.

2. Bashar K, Shalan A, Sharafat Ali S, Tang T, Tiwari A. Endovascular versus medical treatment of venous compression syndrome of the iliac vein - a systematic review. Vasa. 2021; 50(1):22–29. PMID:
33047662.

3. Mickley V, Schwagierek R, Rilinger N, Görich J, Sunder-Plassmann L. Left iliac venous thrombosis caused by venous spur: treatment with thrombectomy and stent implantation. J Vasc Surg. 1998; 28(3):492–497. PMID:
9737459.

4. Gloviczki P, Lawrence PF. Iliac vein stenting and contralateral deep vein thrombosis. J Vasc Surg Venous Lymphat Disord. 2017; 5(1):5–6. PMID:
27987610.

5. Kakkos SK, Gohel M, Baekgaard N, Bauersachs R, Bellmunt-Montoya S, Black SA, et al. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2021 Clinical Practice Guidelines on the management of venous thrombosis. Eur J Vasc Endovasc Surg. 2021; 61(1):9–82. PMID:
33334670.

6. Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011; 123(16):1788–1830. PMID:
21422387.

7. May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957; 8(5):419–427. PMID:
13478912.

8. Taheri SA, Williams J, Powell S, Cullen J, Peer R, Nowakowski P, et al. Iliocaval compression syndrome. Am J Surg. 1987; 154(2):169–172. PMID:
3631389.

9. Berger A, Jaffe JW, York TN. Iliac compression syndrome treated with stent placement. J Vasc Surg. 1995; 21(3):510–514. PMID:
7877235.

10. Hager ES, Yuo T, Tahara R, Dillavou E, Al-Khoury G, Marone L, et al. Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord. 2013; 1(3):270–275. PMID:
26992586.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download