INTRODUCTION
Electric scooters that require standing-up to ride have recently appeared in the public transportation system. They were first introduced in September 2017 by Bird
® Rides, Inc., an electric car-sharing company in Santa Monica, California.
1 Currently offered in hundreds of United States cities and university campuses, electric scooters are gaining huge popularity for their convenience, availability, and economy. The scooters can reach speeds just under 15 mph (24.1 kph) with a range of approximately 20 miles (32.2 km).
2
The popularity of electric scooters in Korea has grown due to their convenient and speedy means of transportation. Furthermore, the use of electric scooters has grown sharply with the introduction of scooter-sharing systems that use apps allowing the users to rent the scooters by the minute. Accordingly, the number of electric scooter-related accidents has also risen sharply over the past years.
Traumatic injuries caused by traffic accidents are diverse and often leave sequelae after treatment.
345 Although the domestic media has frequently reported accidents related to electric scooters, there are few reliable studies on related injuries. This study analyzed the patterns of electric scooter-related accidents and further evaluated the importance of wearing a helmet.
METHODS
Study design
An average of 10,000 trauma patients annually visit the regional trauma center of our institute, which covers a population of 5.0 million in the southwestern region (Gwangju and Jeolla Province) of the Korean peninsula. Since the population of our residential area is one-tenth of the Korean population of both urban and rural areas, the sample of this study is sufficiently representative. A retrospective chart review was conducted on patients who presented to the regional trauma center due to electric scooter accidents from April 2018 to October 2021.
Data collection
Helmet wearing status, sex, age, drinking status, accident timeframe, accident mechanism, electric scooter proficiency (period of use), injury severity, severe trauma, lethality, admission to the intensive care unit, surgery under general anesthesia, and the trauma region were investigated.
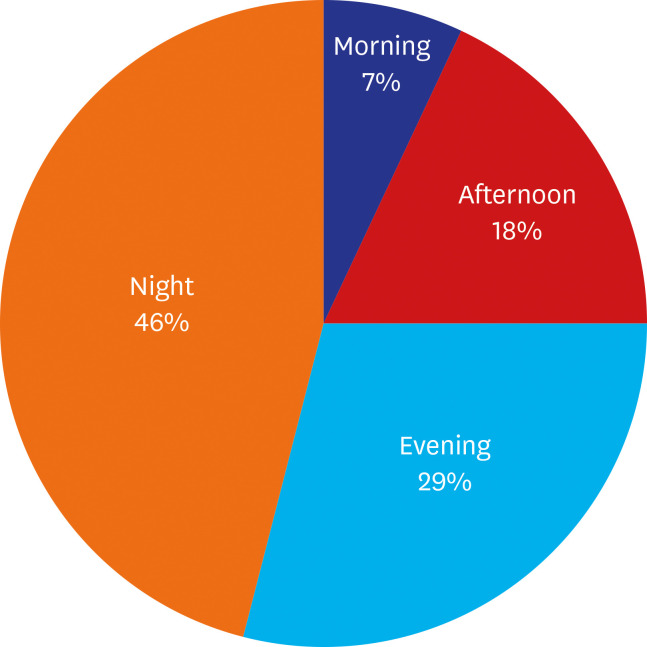
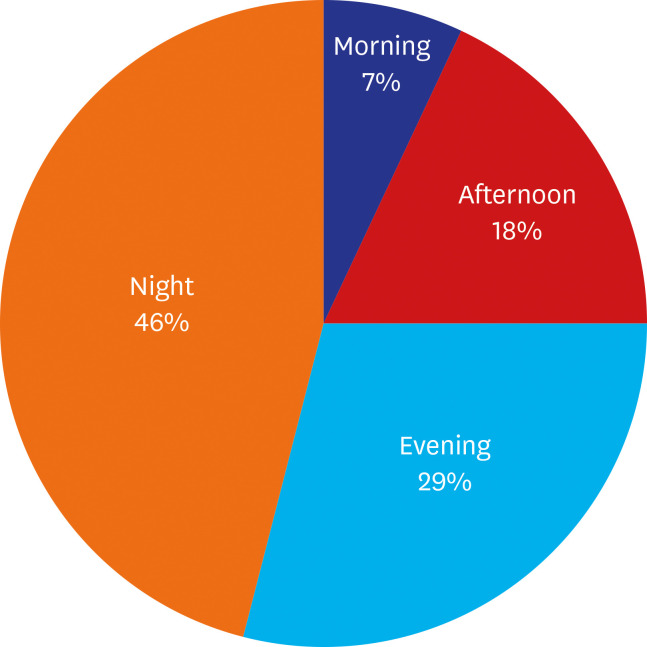
The accident time frame was categorized into morning, afternoon, evening, and night because many traffic accidents occur when it is dark.
6 In spring and autumn, morning, afternoon, evening, and night are defined as 7:00 to noon, noon to 18:00, 18:00 to 22:00, and 22:00 to 7:00 of the next day, respectively. In summer, morning, afternoon, evening, and night are defined as 6:00 to noon, noon to 19:00, 19:00 to 22:00, and 22:00 to 6:00 of the next day, respectively. In winter, morning, afternoon, evening, and night are defined as 8:00 to noon, noon to 17:00, 17:00 to 22:00, and 22:00 to 8:00 of the next day, respectively (
Fig. 1).
Fig. 1
Percentage of electric scooter accidents by time.
Injury severity was determined using the Injury Severity Score (ISS) developed by Baker et al. in 1974. An ISS of 15 or more was defined as major or severe trauma. The ISS was obtained by measuring the Abbreviated Injury Scale (AIS) score in each of six body regions (head or neck, face, chest, abdominal or pelvic contents, extremities or pelvic girdle, and external areas), and among the regions, by summing the square values of the top three scores.
7 Lethality was defined as death, a persistent vegetative state, and post-coma unresponsiveness.
Statistical analysis
All data were analyzed using R version 4.0.2 (The R Foundation, Vienna, Austria). Characteristics of patients and accidents according to wearing a helmet are presented as mean or number (%). Independent t-test and χ2 test were conducted to evaluate differences in characteristics by wearing a helmet. Multivariate linear regression analyses were conducted to investigate the association between wearing a helmet and AIS score. In addition, multivariate linear regression analyses after propensity score were performed matching as sensitivity analyses of the association between wearing a helmet and AIS score. Propensity score matching was conducted in a 1:2 ratio between patients who did wear a helmet and those who did not. The distribution of injury regions and the proportion of patients who conducted surgery under general anesthesia are presented as number (%) in total patients. The distribution of facial trauma subtypes (fracture, laceration, abrasion) and characteristics of each subtype are shown as number (%).
Ethics statement
This study was approved by our Institutional Review Board (IRB) of Chonnam National University Hospital (IRB No. CNUH-2022-005) and conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was waived because of the retrospective nature of the study and the analysis used anonymous clinical data.
RESULTS
Patient demographics
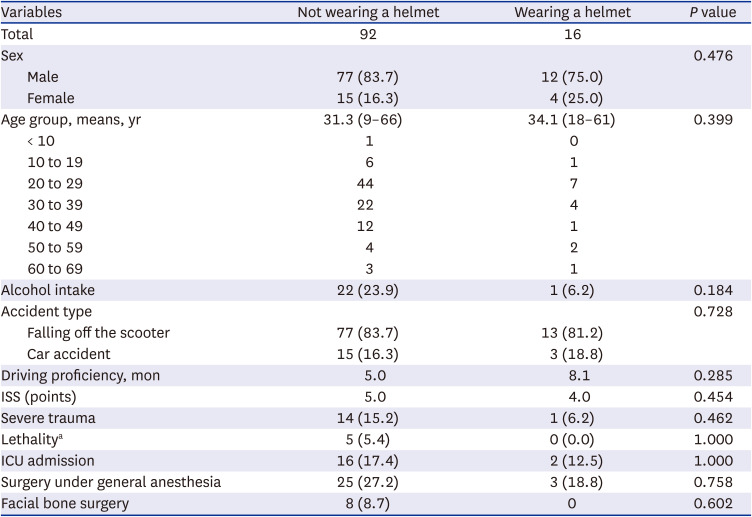
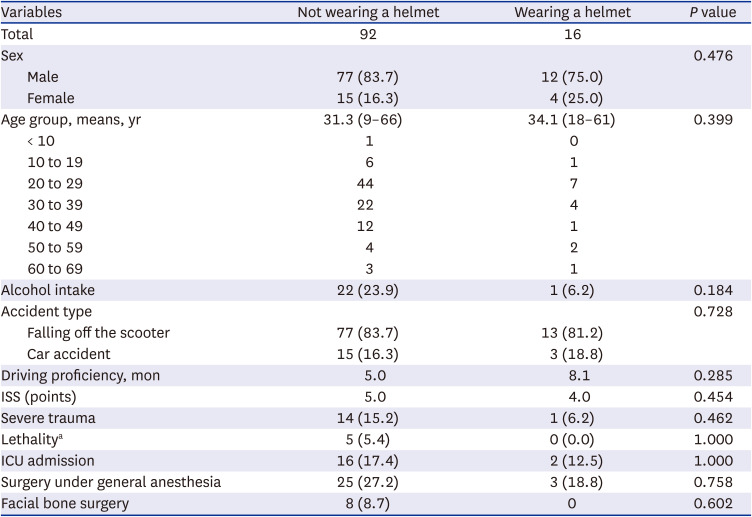
Among 108 patients in electric scooter accidents, 92 patients were not wearing a helmet at the time of injury, whereas 16 patients were wearing a helmet (
Table 1). There were more male patients (n = 89) than female patients (n = 19). There was no significant difference in the average age of patients not wearing a helmet (31.3 years) and wearing a helmet (34.1 years) (
P = 0.399). The age distribution of the patients was as follows: less than 10 years old, n = 1; 10 to 19 years old, n = 7; 20 to 29 years old, n = 51; 30 to 39 years old, n = 26; 40 to 49 years old, n = 13; 50 to 59 years old; n = 6; and 60 years or more, n = 4. Twenty-three answered that they had been drinking at the time of the accident, and 22 of them were not wearing a helmet. The most frequent causes of accidents were inexperience in electric scooter operation and falling off the scooter due to obstacles (90 cases). The electric scooter proficiency was higher in helmet-wearing patients.
Table 1
Demographic characteristics of the patients involved in electric scooter accidents
|
Variables |
Not wearing a helmet |
Wearing a helmet |
P value |
|
Total |
92 |
16 |
|
|
Sex |
|
|
0.476 |
|
Male |
77 (83.7) |
12 (75.0) |
|
Female |
15 (16.3) |
4 (25.0) |
|
Age group, means, yr |
31.3 (9–66) |
34.1 (18–61) |
0.399 |
|
< 10 |
1 |
0 |
|
10 to 19 |
6 |
1 |
|
20 to 29 |
44 |
7 |
|
30 to 39 |
22 |
4 |
|
40 to 49 |
12 |
1 |
|
50 to 59 |
4 |
2 |
|
60 to 69 |
3 |
1 |
|
Alcohol intake |
22 (23.9) |
1 (6.2) |
0.184 |
|
Accident type |
|
|
0.728 |
|
Falling off the scooter |
77 (83.7) |
13 (81.2) |
|
Car accident |
15 (16.3) |
3 (18.8) |
|
Driving proficiency, mon |
5.0 |
8.1 |
0.285 |
|
ISS (points) |
5.0 |
4.0 |
0.454 |
|
Severe trauma |
14 (15.2) |
1 (6.2) |
0.462 |
|
Lethalitya
|
5 (5.4) |
0 (0.0) |
1.000 |
|
ICU admission |
16 (17.4) |
2 (12.5) |
1.000 |
|
Surgery under general anesthesia |
25 (27.2) |
3 (18.8) |
0.758 |
|
Facial bone surgery |
8 (8.7) |
0 |
0.602 |
There was no significant difference in the ISS between the helmet-wearing patient group and the non-helmet-wearing group. However, of the 15 patients with major or severe trauma, 14 patients were not wearing a helmet at the time of injury, and none of the five patients with lethal outcomes were wearing a helmet. Sixteen patients without helmets and two patients with helmets were admitted to the intensive care unit, and there was no significant statistical difference. There was no significant difference in whether surgery was performed under general anesthesia according to the use or non-use of a helmet, whereas none of the patients who underwent facial fracture surgery were wearing a helmet.
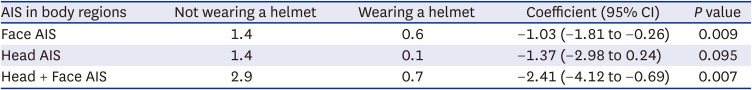
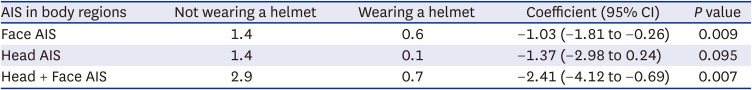
Association between AIS score and the use of a helmet
Patients who were wearing a helmet at the time of injury had lower average AIS scores in the face (1.03) and in the face and head (2.41) than those who were not wearing a helmet (
P = 0.009 and
P = 0.007, respectively) (
Table 2). The average head AIS score was 1.37 points lower in patients who were wearing a helmet, but this difference was not statistically significant (
P = 0.095).
Table 2
Association between AIS score and the use of a helmet based on linear regression analysis
|
AIS in body regions |
Not wearing a helmet |
Wearing a helmet |
Coefficient (95% CI) |
P value |
|
Face AIS |
1.4 |
0.6 |
−1.03 (−1.81 to −0.26) |
0.009 |
|
Head AIS |
1.4 |
0.1 |
−1.37 (−2.98 to 0.24) |
0.095 |
|
Head + Face AIS |
2.9 |
0.7 |
−2.41 (−4.12 to −0.69) |
0.007 |
There was a limit in that the number of patients without wearing a helmet and the number of those who did wear a helmet were more than five times different. Therefore, we balanced measured covariates by estimating the propensity score of patients using a multivariable logistic regression model after adjusted for age, gender, driving proficiency, and accident time variables. Propensity score matching was conducted at a 2:1 ratio between patients who did not wear a helmet and those who did wear a helmet (
Supplementary Table 1). In multivariate linear regression after propensity score matching as sensitivity analysis of the association between wearing a helmet and AIS score, patients who did wear a helmet had lower AIS scores in the face (1.05) and in the face and head (1.96) than those who did not wear a helmet (
P = 0.042 and
P = 0.027, respectively) (
Supplementary Table 2). The head AIS score was 0.91 lower on average in patients who did wear a helmet that in those who did not wear a helmet, although such difference was not statistically significant (
P = 0.246).
Accident timeframe and annual accident count
Accidents occurred most frequently at night (n = 50, 46%) (
Fig. 1). Most of the accidents occurred when it was dark (i.e., after sunset), and accidents occurred either in the evening or at night in 81 of the 108 patients (75%).
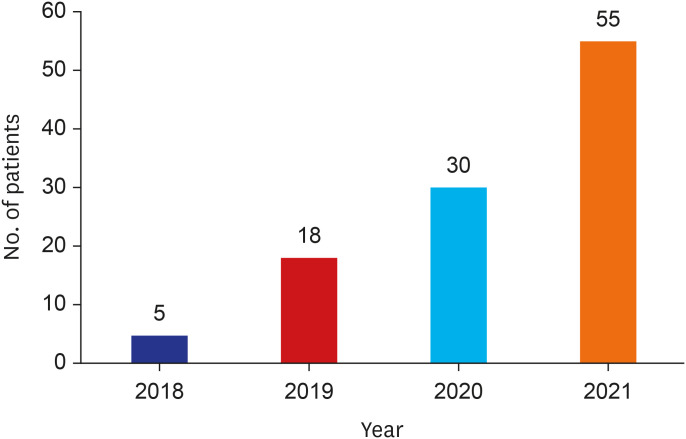
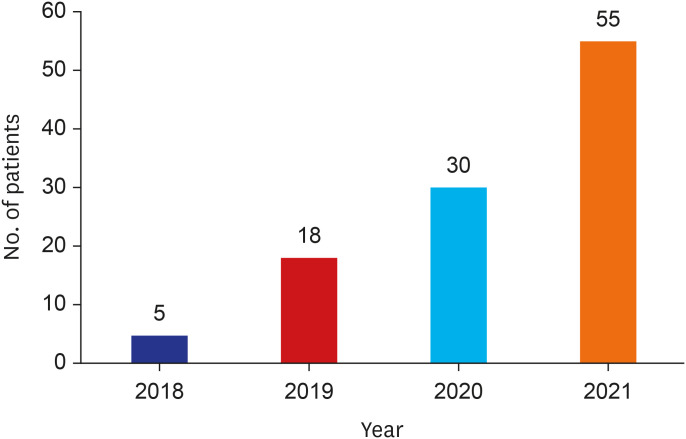
The patients who presented to the regional trauma center of our institute due to an electric scooter accident from April 2018 to October 2021 were classified by year (
Fig. 2). The number of patients seen due to electric scooter accidents annually increased from five cases in 2018 to 18, 30, and 55 cases in 2019, 2020, and 2021, respectively.
Fig. 2
Number of electric scooter-related accidents by year.
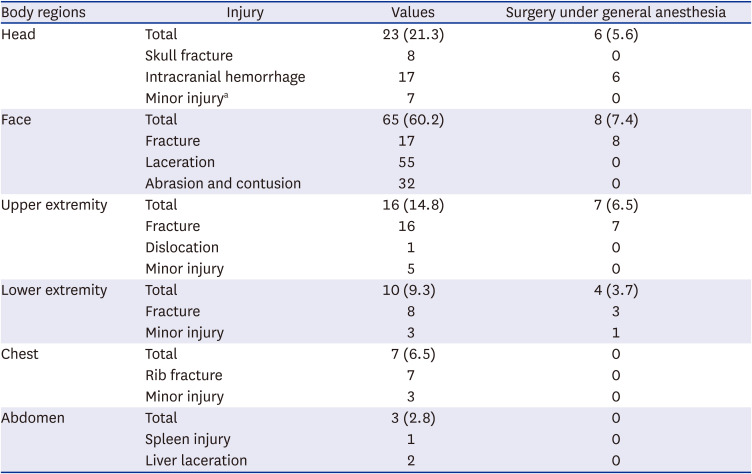
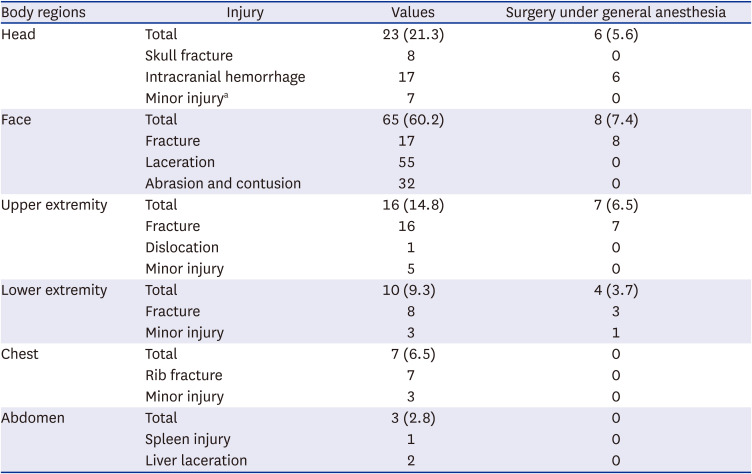
Injury patterns by body region
Injuries due to electric scooter accidents were classified by body region. The most frequent injury region was the face (n = 65, 60.2%), followed by the head (n = 23, 21.3%), and upper extremity (n = 16, 14.8%). Ten, seven, and three patients had injuries in the lower extremity, chest, and abdomen, respectively.
Six patients (5.6%) with head injuries required surgery under general anesthesia due to the presence of intracranial hemorrhage. Eight patients (7.4%) with face injuries needed surgery under general anesthesia due to the presence of facial bone fractures. Seven patients (6.5%) with upper extremity injuries required surgery under general anesthesia due to fractures. In addition, surgery under general anesthesia was required for three patients with lower extremity injuries and one patient with a minor injury. None of the patients with chest and abdomen injuries needed surgery under general anesthesia (
Table 3).
Table 3
Distribution of injury regions and surgery under general anesthesia in patients involved in electric scooter accidents
|
Body regions |
Injury |
Values |
Surgery under general anesthesia |
|
Head |
Total |
23 (21.3) |
6 (5.6) |
|
Skull fracture |
8 |
0 |
|
Intracranial hemorrhage |
17 |
6 |
|
Minor injurya
|
7 |
0 |
|
Face |
Total |
65 (60.2) |
8 (7.4) |
|
Fracture |
17 |
8 |
|
Laceration |
55 |
0 |
|
Abrasion and contusion |
32 |
0 |
|
Upper extremity |
Total |
16 (14.8) |
7 (6.5) |
|
Fracture |
16 |
7 |
|
Dislocation |
1 |
0 |
|
Minor injury |
5 |
0 |
|
Lower extremity |
Total |
10 (9.3) |
4 (3.7) |
|
Fracture |
8 |
3 |
|
Minor injury |
3 |
1 |
|
Chest |
Total |
7 (6.5) |
0 |
|
Rib fracture |
7 |
0 |
|
Minor injury |
3 |
0 |
|
Abdomen |
Total |
3 (2.8) |
0 |
|
Spleen injury |
1 |
0 |
|
Liver laceration |
2 |
0 |
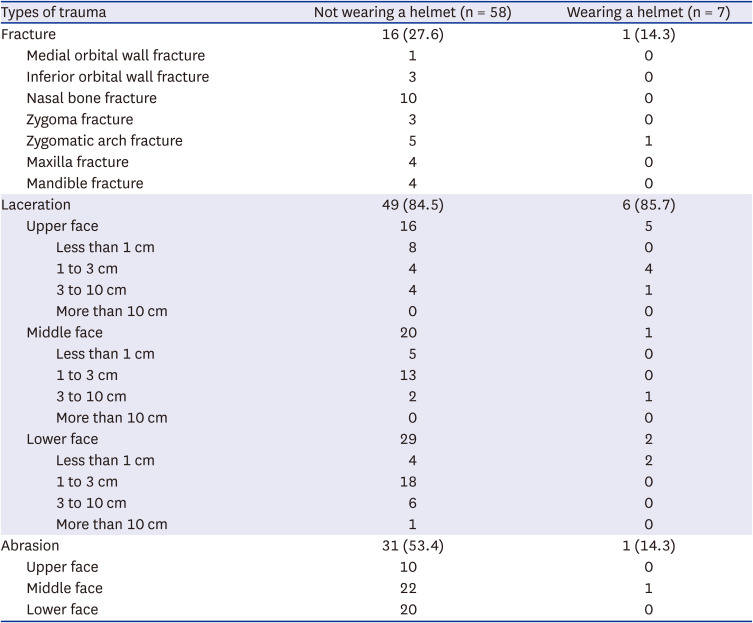
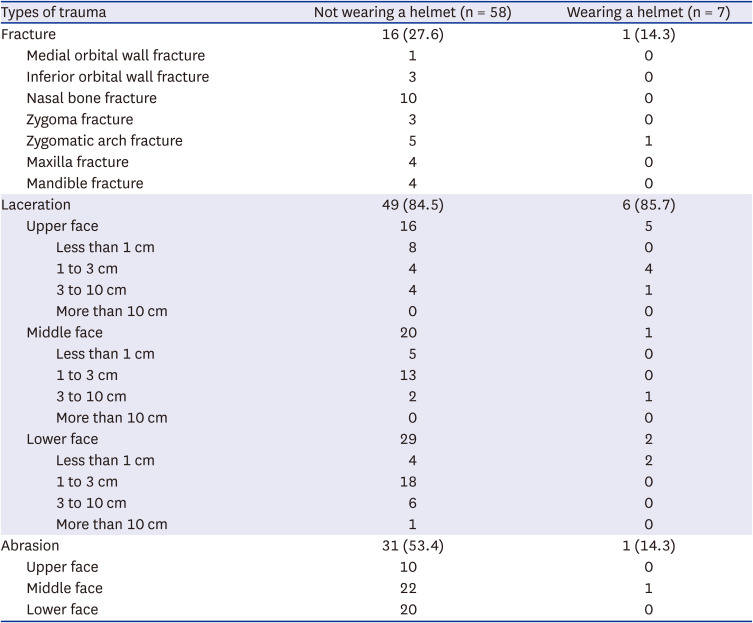
Injury patterns by face part depending upon helmet use
The 65 patients (60.2%) with facial trauma due to electric scooter accidents were subdivided depending upon the use or non-use of a helmet (
Table 4). The 17 patients with facial bone fractures were classified by fracture region. In the patients who were not wearing a helmet, nasal bone fractures were the most frequent, followed by zygomatic arch, maxilla, and mandible fractures. One patient who was wearing a helmet experienced a zygomatic arch fracture.
Table 4
Distribution of facial trauma according to helmet use
|
Types of trauma |
Not wearing a helmet (n = 58) |
Wearing a helmet (n = 7) |
|
Fracture |
16 (27.6) |
1 (14.3) |
|
Medial orbital wall fracture |
1 |
0 |
|
Inferior orbital wall fracture |
3 |
0 |
|
Nasal bone fracture |
10 |
0 |
|
Zygoma fracture |
3 |
0 |
|
Zygomatic arch fracture |
5 |
1 |
|
Maxilla fracture |
4 |
0 |
|
Mandible fracture |
4 |
0 |
|
Laceration |
49 (84.5) |
6 (85.7) |
|
Upper face |
16 |
5 |
|
|
Less than 1 cm |
8 |
0 |
|
|
1 to 3 cm |
4 |
4 |
|
|
3 to 10 cm |
4 |
1 |
|
|
More than 10 cm |
0 |
0 |
|
Middle face |
20 |
1 |
|
|
Less than 1 cm |
5 |
0 |
|
|
1 to 3 cm |
13 |
0 |
|
|
3 to 10 cm |
2 |
1 |
|
|
More than 10 cm |
0 |
0 |
|
Lower face |
29 |
2 |
|
|
Less than 1 cm |
4 |
2 |
|
|
1 to 3 cm |
18 |
0 |
|
|
3 to 10 cm |
6 |
0 |
|
|
More than 10 cm |
1 |
0 |
|
Abrasion |
31 (53.4) |
1 (14.3) |
|
Upper face |
10 |
0 |
|
Middle face |
22 |
1 |
|
Lower face |
20 |
0 |
Lacerations were classified depending upon their total length in the corresponding region after subdividing the facial region into the upper face (the top of the forehead to the glabella), middle face (the glabella to the subnasale), and lower face (the subnasale to the bottom of the chin). Lacerations in the lower face (n = 29) were found most frequently in patients who were not wearing a helmet, whereas the upper face (n = 5) was the most frequently lacerated area in patients who were wearing a helmet.
Abrasions were classified according to whether they occurred on the upper, middle, or lower face. Abrasions were most commonly found on the middle face (n = 22) in patients who were not wearing a helmet and in patients who were wearing a helmet (n = 1).
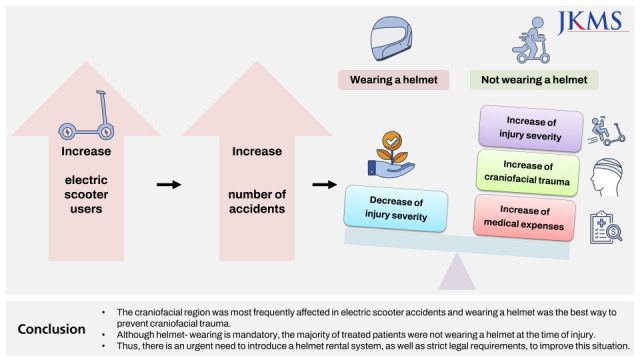
DISCUSSION
Electric scooters have gained considerable popularity recently as a swift and convenient means of mobility, and the number of users is increasing. However, with the increasing number of electric scooter-related accidents and associated medical expenses, there is a growing interest in safety issues and institutional regulations for electric scooters.
8 Bloom et al.
9 have surveyed 248 electric scooter patients and found that only eight (3%) wear helmets in Los Angeles. They suggested that it would be necessary to make the use of safety equipment mandatory and that related policies should be further investigated and supplemented. Shichman et al.
10 have reported that the number of patients visiting emergency room has increased rapidly since the introduction of electric scooters. In addition, they reported that the effect of using electric scooters on both emergency and surgical departments increased the burden of the medical system. Lavoie-Gagne et al.
11 have reported that it is necessary to use head protection to reduce injuries caused by electric scooters.
In Korea, a driver’s license is required to use an electric scooter in accordance with the revised Road Traffic Act as of May 13, 2021. More specifically, a class 2 driver’s license for motorcycles or a permit for other types of vehicles, available for people aged 16 or over, is needed to use an electric scooter. Furthermore, helmet-wearing while riding is mandatory for the safety of the riders. The tightened regulations further include a ban on the act of driving on sidewalks and a requirement to have lights on when driving at night.
Despite this revision of the Road Traffic Act, injuries have increased annually due to the low proficiency of users and poor compliance with the revised Act because the electric scooter is a new means of mobility that was recently introduced. According to the Korea Transportation Safety Authority, the helmet utilization rate was 16.1% of domestic electric scooter users, and five out of six people did not wear a helmet.
12 This study revealed that there was an annual increase in the number of patients with electric scooter accidents, from five patients in 2018 to 18, 30, and 55 patients in 2019, 2020, and 2021, respectively. Of the 108 patients in electric scooter accidents, 16 were wearing a helmet, corresponding to a helmet utilization rate of only 14.8%.
Among the 16 patients who were wearing a helmet, 14 patients were wearing a half-face helmet and only two patients were wearing a full-face helmet. The highest number of patients without a helmet were those in their 20s, with 44 people, followed by those in their 30s, with 22 people. The highest number of patients who were wearing a helmet was also found among those in their 20s, with seven patients, followed by those in their 30s, with four patients. Due to the high number of accidents among young people in their 20s and 30s, it is considered important to reduce the number of accidents by actively promoting the safe operation of electric scooters among young people.
In this study, craniofacial trauma was the most frequent, followed by upper extremity trauma. In particular, the AIS score in the face and head region was significantly lower in patients who were wearing a helmet than in those who were not wearing a helmet, implying that wearing a helmet could reduce the severity of craniofacial injuries. Because the electric scooter rider operates it while standing on the platform, the center of gravity is shifted forward and upward. Due to the lack of a rigid pivotal connection between the rider and the electric scooter, an interruption by an obstacle or sudden deceleration leads the rider to fall from the head and upper body to the ground.
13 Overseas studies have analyzed injury patterns of electric scooter accidents and shown a similar trend. Alwani et al.
2 have analyzed injury patterns of 89 patients with electric scooter accidents in Indianapolis, Indiana, USA and reported a high rate of head and neck injury (42.7%). Faraji et al.
14 have analyzed 203 craniofacial injuries from electric scooter accidents in San Diego, California, USA and reported that the most common injury area in the face is the midface. Störmann et al.
15 have reported that upper extremity injury (47.4%), head and face injury (38.2%), and lower extremity injury (36.8%) among 76 patients in electric scooter accidents in Frankfurt, Germany. The study of Störmann et al.
15 found that electric scooters with relatively small wheels and lower body characteristics than bicycles caused injuries mainly in the head and extremities than the chest and abdomen due to their low falling height compared to fast speed and too short reaction time in the event of an accident.
As of October 2021, our city government has provided approximately 5,700 shared electric scooters. Shared electric scooters placed on the street are freely available to anyone, and the utilization rate of helmets is quite low. To increase the helmet-wearing rate, it is necessary to develop a system that allows individuals to conveniently rent and use a helmet while operating an electric scooter without carrying their own helmet.
Although drunk driving is regulated by law in Korea, electric scooter accidents under the influence of alcohol are frequent. In this study, 23 (21.3%) of the 108 electric scooter accident patients were operating the devices under the influence of alcohol. Reports from other countries have described many electric scooter accidents after drinking or using other drugs.
1516 Driving an electric scooter under the influence of alcohol can lead to serious accidents because drinking prevents the driver from making sound judgments and properly controlling their actions. Although driving electric scooters while drunk is subject to the same administrative punishment as that of automobiles since the revision of the Road Traffic Act, users frequently engage in drunk driving without an awareness of the risk of serious accidents.
In this study, 81 patients (75%) were involved in accidents in the evening or at night. As daylight diminishes after sunset, the average speed of drivers and their recognition rate of road signs drops significantly.
17 To reduce accidents at night, it is necessary to improve headlights and taillights on electric scooters.
Although this is the first study on electric scooter-related accidents according to whether a helmet is worn in Korea, it has several limitations. First, not many patients were wearing helmets in this study. The number of patients who did not wear a helmet was corrected through multivariate analysis and propensity matching. However, it is necessary to analyze trauma patterns by accumulating a large number of patients after long-term observation. Second, since this study relied on medical records of patients who visited the regional trauma center, patients without severe wounds or fractures who visited other local clinics might have been omitted.
In conclusion, the increasing number of electric scooter users has resulted in a rise in the number of patients presenting to the emergency room due to related injuries. The most frequent trauma region in electric scooter accidents was the craniofacial region, and wearing a helmet was determined to be the best way to prevent craniofacial trauma. Because the helmet-wearing rate was remarkably low despite the current regulations mandating that riders wear them, there is an urgent need to introduce a system for renting a helmet along with an electric scooter to encourage helmet use.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download