Abstract
Cerebral venous sinus thrombosis (CVST) following a closed head injury in pediatric patients is a rare condition, and an early spontaneous recanalization of this condition is extremely rare. A 10-year-old boy was admitted with a mild, intermittent headache and nausea five days after a bicycle accident. The brain computed tomography showed an epidural hematoma at the right occipital area with pneumocephalus due to a fracture of the occipital skull bone. The brain magnetic resonance imaging and the magnetic resonance venography demonstrated a flow signal loss from the right sigmoid sinus to the right jugular vein. The diagnosis was sigmoid sinus thrombosis, so close observations were selected as a treatment for the patient because of his gradually improving symptoms; however, he complained of vomiting 14 days the after conservative treatment. The patient was readmitted for a further examination of his symptoms. The laboratory and the gastroenterological examinations were normal. Due to concern regarding the worsening of the sigmoid sinus thrombosis, the brain magnetic resonance venography was rechecked and it revealed the recanalization of the venous flow in the sigmoid sinus and in the jugular vein.
Pediatric cerebral venous sinus thrombosis (CVST) is rare and it can significantly cause neurological adverse outcomes in patients7). The annual incidence of CVST is 0.67 per 100000 children7). Because half of the events occurred during the neonatal period, the incidence of CVST is 0.34 per 100000 in non-neonate children per year27). There are various risk factors of pediatric CVST including thrombophilic states, acute systemic illness, chronic systemic diseases, and head and neck disorders7). Head and neck disorders are more common in non-neonates (1 month to 18 years old)7). CVST following a closed head injury in particular is very rare in childhood1). The diagnosis of CVST after a minor head injury is not easy because of the rarity of occurrence, so a high degree of suspicion is the most important factor to the diagnosis of a patient presenting progressive ambiguous symptoms such as headaches, vomiting, and imbalance23). Even though anticoagulation is recommended for the treatment of pediatric CVST19), close observation can be a mainstay therapy for CVST caused by a minor head injury17). The prognosis has been reported to be relatively favorable in children17). We report on one pediatric case of early spontaneous recanalization of sigmoid sinus thrombosis after a closed minor head injury with a literature review.
A 10-year-old male fell while riding a bicycle on the road. On the day of the fall, he had no definite symptoms; however, he complained of a mild, intermittent headache and nausea five days after the incident and visited the hospital. His neurological state was normal and there were no blood stains in the ear, nose, or throat. The brain computed tomography (CT) revealed a linear fracture, small amounts of epidural hematomas and pneumocephalus in the right occipital area. When compared to the left side, a higher density lesion within the right sigmoid sinus was found (Fig. 1). The brain magnetic resonance image (MRI) showed the effusion and hemorrhage in the right mastoid air cell and a signal intensity, which was suspected to be thrombus, in the right sigmoid sinus (Fig. 2). The brain magnetic resonance venography (MRV) revealed an absence of a flow signal between the right sigmoid sinus and the jugular bulb, which was confirmed to be sigmoid sinus thrombosis (Fig. 3A). During the physical examination, he showed no papilledema, intracranial hypertension, or otogenic infections such as otitis media. His blood tests, including complete blood count, prothrombin time, partial thromboplastin time, antithrombin III, protein C activity, and protein S activity, were in the normal ranges. The patient was treated conservatively because the patient's symptoms were mild and gradually improved. He was discharged with a full recovery on the 4th day in the hospital. On the 10th day after discharge, the patient complained of vomiting and visited the department of pediatrics. The laboratory tests, including a prothrombotic evaluation and a physical examination, were performed. The results of the laboratory tests were normal. Due to concern regarding the progression of the previous sinus thrombosis, the brain MRV was re-checked, and it showed the recovery of the flow signal in the right sigmoid sinus (Fig. 3B). The spontaneous recanalization of sigmoid sinus thrombosis occurred within about three weeks of the trauma. His vomiting may have been caused by gastrointestinal problems, and it ceased the following day.
The exact mechanism of sinus thrombosis following a closed head injury is unknown, although several theories have been suggested16171824). One possible mechanism is a direct injury with a linear fracture crossing the wall of the dural sinus16). It may also be caused by a rupture of the small sinusoids, an injury to the endothelial lining, or an extension of thrombus from the emissary veins18). The other suggested mechanism is a temporary alteration in the coagulation after a head injury, disturbances in the blood flow (venous stasis), or damage to the capillary endothelium, all of which may predispose a person to thrombosis24). Compared with adult groups, CVST following a closed head injury in children has a number of different characteristics. For example, pediatric patients tend to be affected more often than adults by posttraumatic venous sinus thrombosis because of the immaturity of their cerebral venous collateral vasculature6).
Children with posttraumatic sinus thrombosis show delayed neurological symptoms, such as headaches, vomiting, irritability, or gait ataxia23). In another study, children were shown to be more likely to experience seizures and mental changes, while adults were more likely to experience headaches and diplopia10). The diagnosis should be made early in the course of this pathology in order to begin the treatment as well as to prevent complications that could become fatal. A high degree of clinical suspicion is the most important factor in the early diagnosis of CVST in pediatric patients23).
The confirmation of the diagnosis relies on the demonstration of thrombus by detailed neuroimaging techniques, such as a contrast CT with venography, an MRV, or a cerebral angiography. Sometimes CVST can be identified on brain CT scans as clots in the cortical veins, namely the "cord sign" and the "dense vein sign"5). This is caused by clots filled with dural sinus as well as filling defects in the superior sagittal sinus, or the so-called "empty delta sign"20). A brain MRI with the addition of an MRV is the most sensitive imaging tool for diagnosing CVST, which non-invasively provides a direct visualization of the dural sinuses and any sinus flow abnormalities21). A cerebral angiography can be performed if the previously mentioned examinations are inaccurate or ambiguous, although the interpretation can sometimes be challenging because transverse sinus hypoplasia or aplasia could be identified through the angiography in the general population22). Therefore, we suggest that an MRI with an MRV is the best choice of imaging tools. In our case, a brain CT showed a "dense vein sign" in the sigmoid sinus (Fig. 1D), and thrombus in the right sigmoid sinus demonstrated a low signal intensity in a T2-weighted image and an iso-signal intensity in a T1-weighted image on the brain MRI (Fig. 2).
Treatment planning should be based on clinical findings and etiologies17). In cases of adult CVST, several articles generally recommend anticoagulation therapy (ACT) and even aggressive treatments such as endovascular thrombolytic therapy or surgical thrombectomy in severe cases41618). Some authors suggested the use of endovascular balloons as an alternative in cases of anticoagulation and decompressive craniectomy3); however, most pediatric patients with CSVT from minor head injury had favorable outcomes regardless of the treatment strategies17). Some authors recommended that anticoagulation be reserved for patients presenting a papilledema or complaining of persistent headache, vomiting, or disequilibrium17). We agreed with their opinions and treated our patient conservatively, because the patient's symptoms were mild and non-persistent. Anticoagulants, such as heparin, can be used to treat thrombosis; however, there is an increased risk for a venous hemorrhagic infarction21). This is especially true if the patient has a history of intracranial bleeding. Pediatric patients should be treated carefully with adequate monitoring of the complications. Therefore, some authors recommended low-molecular-weight heparin as a proper choice for treating CVST with intracranial hemorrhages instead of heparin because of concerns regarding aggressively increasing hemorrhages19).
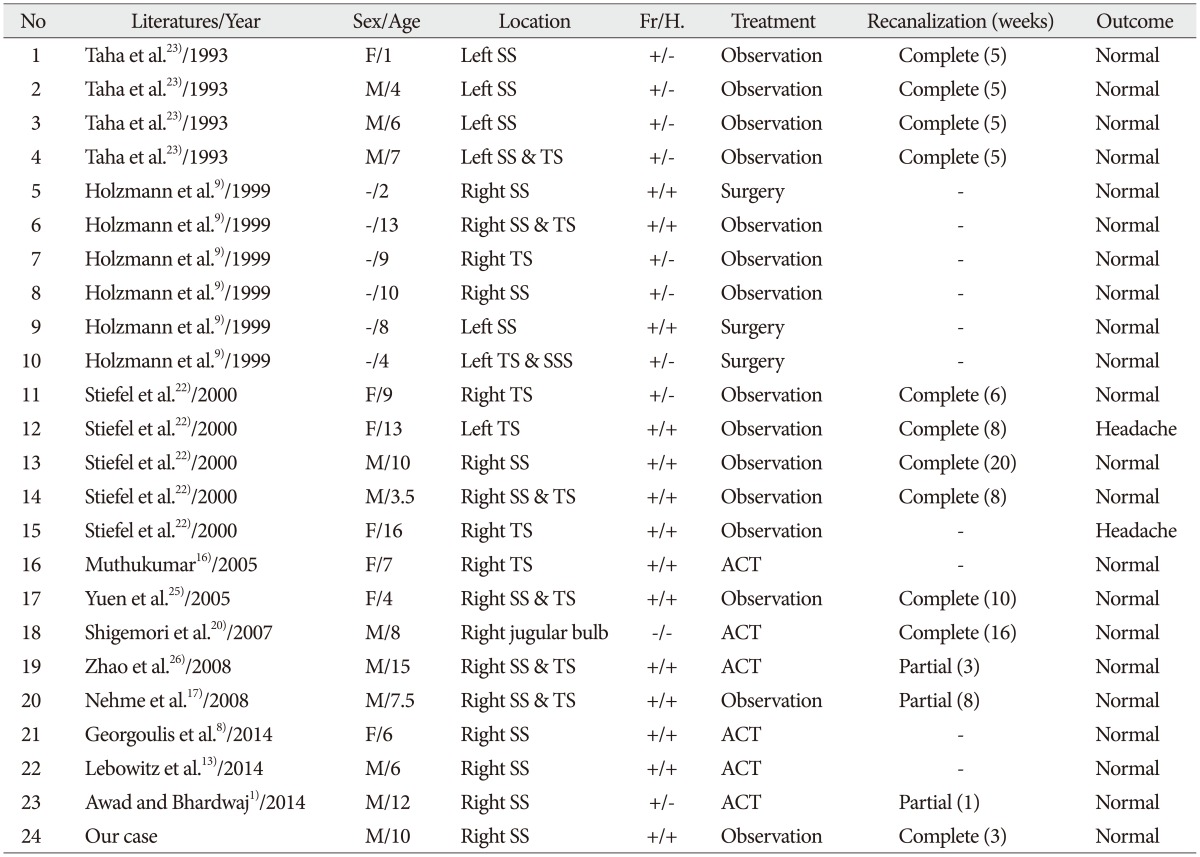
There are several studies about CVST following a closed head injury in pediatrics (Table 1). Twenty-three patients in 11 studies have been reported891316172022232526). The frequently involved locations were the sigmoid sinus (69.6%) and the transverse sinus (52.2%). In researching the literatures, it was found that most cases (60.9%) were treated conservatively and had favorable outcomes, including two cases with recurrent headaches. Five cases of ACT and three surgical cases also had favorable outcomes. The radiologic confirmation of recanalization was performed in 13 cases and most of them were diagnosed by only a brain CT or only a brain MRI rather than a combination of these tests with an MRV. There was no case of recanalization confirmed by MRV within one month. The mechanism of spontaneous recanalization is unknown. A case of spontaneous recanalization within one month in CVST is extremely rare. Even though the precise mechanism of recanalization is still obscure, an early spontaneous recanalization of deep vein thrombosis was reported in some articles1114). Recanalization can be caused by more active fibrinolytic activity than procoagulation activity. It was reported that the regression of acute deep vein thrombosis begins early and is accompanied by a significant increase in the endogenous fibrinolytic agent, tissue plasminogen activator1215). Thus, recanalization is determined by activated coagulation and impaired fibrinolysis15).
Our case is notable for several reasons. Although CVST following a closed head injury is still rare in children and spontaneous recanalization within one month has not been reported, pediatric CVST following a mild head injury and spontaneous recanalization may not be that rare because a lesion that may recover uneventfully may frequently be misread. CVST should be suspected in patients with posttraumatic symptoms, even in pediatric cases of mild head injuries, because CSVT could lead to catastrophic outcomes, such as a large venous infarction. Treatment should be based on clinical findings and outcomes and should consist of measures that counteract thrombosis.
Acknowledgements
The present research was conducted under a research fund from Dankook University in 2013.
References
1. Awad AW, Bhardwaj R. Acute posttraumatic pediatric cerebral venous thrombosis : case report and review of literature. Surg Neurol Int. 2014; 5:53. PMID: 24818060.

2. Barnes C, Newall F, Furmedge J, Mackay M, Monagle P. Cerebral sinus venous thrombosis in children. J Paediatr Child Health. 2004; 40:53–55. PMID: 14718006.

3. Bishop FS, Finn MA, Samuelson M, Schmidt RH. Endovascular balloon angioplasty for treatment of posttraumatic venous sinus thrombosis. Case report. J Neurosurg. 2009; 111:17–21. PMID: 19326975.

4. Brors D, Schäfers M, Schick B, Dazert S, Draf W, Kahle G. Sigmoid and transverse sinus thrombosis after closed head injury presenting with unilateral hearing loss. Neuroradiology. 2001; 43:144–146. PMID: 11326560.

5. Buonanno FS, Moody DM, Ball MR, Laster DW. Computed cranial tomographic findings in cerebral sinovenous occlusion. J Comput Assist Tomogr. 1978; 2:281–290. PMID: 263491.

6. Dalgiç A, Seçer M, Ergüngör F, Okay O, Akdağ R, Ciliz D. Dural sinus thrombosis following head injury : report of two cases and review of the literature. Turk Neurosurg. 2008; 18:70–77. PMID: 18382983.
7. deVeber G, Andrew M, Adams C, Bjornson B, Booth F, Buckley DJ, et al. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001; 345:417–423.

8. Georgoulis G, Alexiou G, Prodromou N. Sigmoid sinus thrombosis as a sequela of head injury in children and its management. World Neurosurg. 2014; 81:e7.

9. Holzmann D, Huisman TA, Linder TE. Lateral dural sinus thrombosis in childhood. Laryngoscope. 1999; 109:645–651. PMID: 10201757.

10. Jackson BF, Porcher FK, Zapton DT, Losek JD. Cerebral sinovenous thrombosis in children : diagnosis and treatment. Pediatr Emerg Care. 2011; 27:874–880. quiz 881-883PMID: 21926891.
11. Killewich LA, Bedford GR, Beach KW, Strandness DE Jr. Spontaneous lysis of deep venous thrombi : rate and outcome. J Vasc Surg. 1989; 9:89–97. PMID: 2911146.
12. Killewich LA, Macko RF, Cox K, Franklin DR, Benjamin ME, Lilly MP, et al. Regression of proximal deep venous thrombosis is associated with fibrinolytic enhancement. J Vasc Surg. 1997; 26:861–868. PMID: 9372826.

13. Lebowitz DC, Ko MW, Cameron EK, Ko PY. Cerebral sinus thrombosis in a 6-year-old boy after a minor head injury. Pediatr Emerg Care. 2014; 30:177–179. PMID: 24589805.

14. Markel A, Meissner M, Manzo RA, Bergelin RO, Strandness DE Jr. Deep venous thrombosis : rate of spontaneous lysis and thrombus extension. Int Angiol. 2003; 22:376–382. PMID: 15153822.
15. Meissner MH, Zierler BK, Bergelin RO, Chandler WL, Strandness DE Jr. Coagulation, fibrinolysis, and recanalization after acute deep venous thrombosis. J Vasc Surg. 2002; 35:278–285. PMID: 11854725.

16. Muthukumar N. Uncommon cause of sinus thrombosis following closed mild head injury in a child. Childs Nerv Syst. 2005; 21:86–88. PMID: 15168052.

17. Nehme J, Dcarie JC, Saliba I. Lateral sinus thrombosis : complication of minor head injury. Int J Pediatr Otorhinolaryngol. 2009; 73:629–635. PMID: 19084283.
18. Ochagavia AR, Boque MC, Torre C, Alonso S, Sirvent JJ. Dural venous sinus thrombosis due to cranial trauma. Lancet. 1996; 347:1564. PMID: 8684142.

19. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis : a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:1158–1192. PMID: 21293023.

20. Shigemori Y, Koshinaga M, Suma T, Nakamura S, Murata Y, Kawamata T, et al. Jugular bulb venous thrombosis caused by mild head injury : a case report. Surg Neurol. 2007; 68:660–664. discussion 664PMID: 18053865.

21. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005; 352:1791–1798. PMID: 15858188.

22. Stiefel D, Eich G, Sacher P. Posttraumatic dural sinus thrombosis in children. Eur J Pediatr Surg. 2000; 10:41–44. PMID: 10770246.

23. Taha JM, Crone KR, Berger TS, Becket WW, Prenger EC. Sigmoid sinus thrombosis after closed head injury in children. Neurosurgery. 1993; 32:541–545. discussion 545-546PMID: 8474644.

24. Tamimi A, Abu-Elrub M, Shudifat A, Saleh Q, Kharazi K, Tamimi I. Superior sagittal sinus thrombosis associated with raised intracranial pressure in closed head injury with depressed skull fracture. Pediatr Neurosurg. 2005; 41:237–240. PMID: 16195674.

25. Yuen HW, Gan BK, Seow WT, Tan HK. Dural sinus thrombosis after minor head injury in a child. Ann Acad Med Singapore. 2005; 34:639–641. PMID: 16382251.
26. Zhao X, Rizzo A, Malek B, Fakhry S, Watson J. Basilar skull fracture : a risk factor for transverse/sigmoid venous sinus obstruction. J Neurotrauma. 2008; 25:104–111. PMID: 18260793.

Fig. 1
Brain computed tomography (CT) showed a linear fracture in the right occipital bone (A) and a suspicious intracranial hematoma (B, white arrow) with pneumocephalus (C) around the fracture site. Additionally, a high-density lesion located in right sigmoid sinus was revealed (D, black arrow, "dense vein sign").
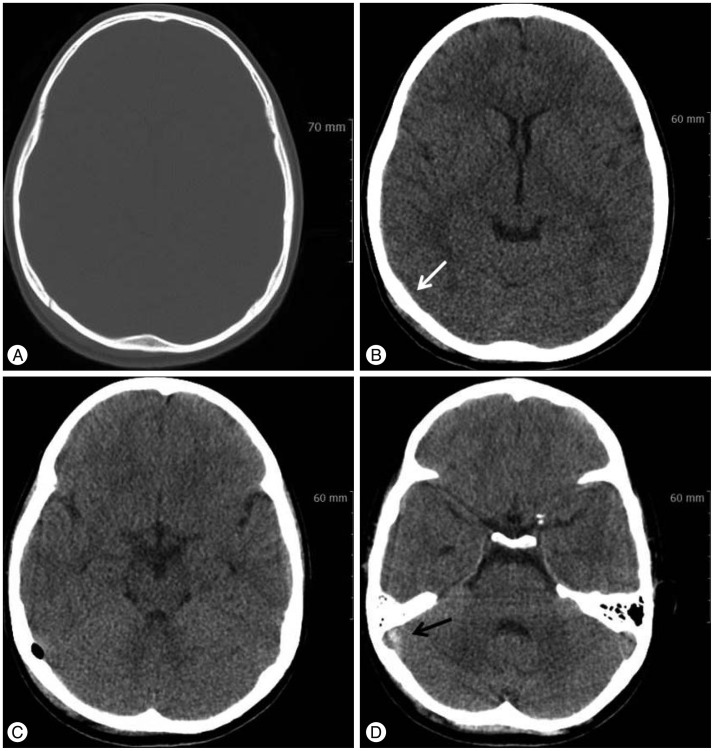
Fig. 2
In contrast with left side, the thrombus in the right sigmoid sinus demonstrated low signal intensity in a T2-weighted image (A, black arrow) and iso-signal intensity in a T1-weighted image (B, white arrow) on brain magnetic resonance image (MRI).
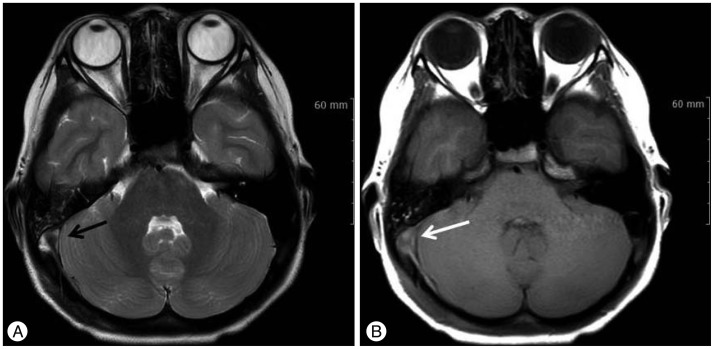
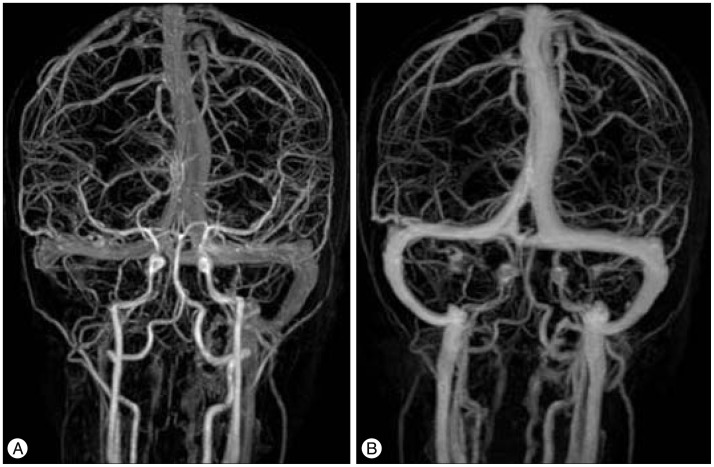
Fig. 3
A : Initial brain magnetic resonance venography (MRV) demonstrated a loss of the flow signal from the right sigmoid sinus to the distal (white arrow). B : After about three weeks, a follow-up brain MRV demonstrated a recanalization of the sinus, which was a recovery of the signal from the right sigmoid sinus to the distal jugular vein.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download