Abstract
The most common neurologic manifestations of polycythemia vera (PV) are cerebral infarction and transient ischemic attacks, while cerebral hemorrhage or intracranial dissection has been rarely associated with PV. Here we report the first case of a 59-year-old patient with intracranial supraclinoid internal carotid artery (ICA) dissection causing cerebral infarction and concomitant subarachnoid hemorrhage due to pseudoaneurysm rupture as clinical onset of PV. This case report discusses the possible mechanism and treatment of this extremely rare condition.
Polycythemia vera (PV) is a rare, myeloproliferative disorder characterized by a great expansion of erythrocytic mass associated with an increase in leukocytes and platelets production8). The most common neurologic manifestations of PV are ischemic strokes such as cerebral infarction and transient ischemic attacks68). However, hemorrhagic stroke has been rarely associated with PV. Intracranial pseudoaneurysm formation causing subarachnoid hemorrhage in a patient with PV has not been described in the literature. In addition, simultaneous presentation of ischemic/hemorrhagic stroke in intracranial dissection is very rare condition78). Here we report the first case of a patient with intracranial supraclinoid internal carotid artery (ICA) dissection causing cerebral infarction and concomitant subarachnoid hemorrhage (SAH) due to pseudoaneurysm rupture as an initial presentation of PV.
A 59-year-old woman was admitted to our hospital 2 days after the onset of a recurrent thunderclap headache and right-side hemiparesis recovered within a day. She was drowsy, and had apparent nuchal rigidity. She had no risk factors for cerebrovascular diseases. She was in normotensive and in sinus rhythm. A computed tomography (CT) scan revealed SAH on left basal cistern (Fig. 1A). Magnetic resonance (MR) images showed an acute ischemic lesion in the territory of the left middle cerebral artery with restricted diffusion (Fig. 1B-E). Digital subtraction angiography (DSA) demonstrated an irregularly shaped aneurysm arising from left supraclinoid ICA with moderate stenosis of proximal region (Fig. 1F). Moreover, DSA revealed one of the typical findings of pseudoaneurysm. A delayed opacification and stagnation of contrast medium in the aneurysm sac even during the venous phase were observed (Fig. 1G, H). Transthoracic echocardiography with carotid duplex ultrasonography was negative.
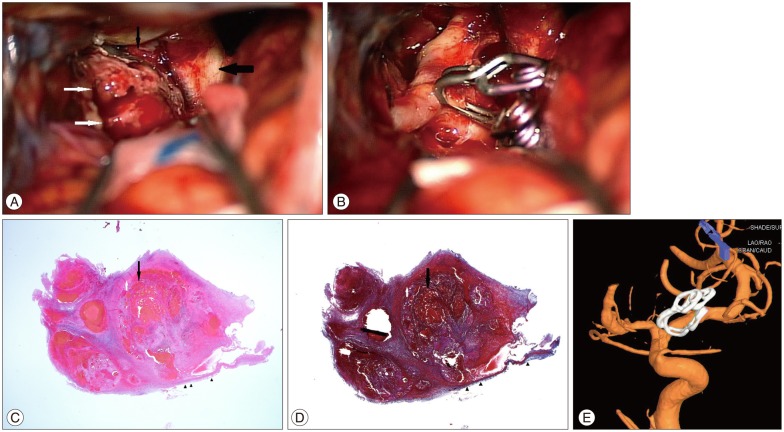
Laboratory evaluation revealed a hemoglobin concentration of 18.3 g/dL with an elevated hematocrit of 59.7%, white blood cell count of 11.4×103/µL, and platelet count of 1120×103/µL. There was no evidence of head trauma or any systemic infection signs on admission. We planned to perform surgical clipping with a vessel wall remodeling technique because pseudoaneurysm might be fragile and associated with a high risk of intraoperative rupture. During operation, a pulsatile, thin walled aneurysm adherent to the adjacent tissue was observed in the anterior wall of supraclinoid ICA (Fig. 2A). The aneurysmal sac avulsed from the parent vessel due to its friability during dissection of aneurysm. After temporary clipping of the proximal ICA, three curved clips were applied with a facing fashion to close the torn gap in order to prevent rebleeding and maintain patency of the parent vessel (Fig. 2B). Postoperative hospital course was uneventful. Pathologic examination showed that most of the lumen mainly consisted of organized blood clot and recent thrombus surrounded with a layer of fibrous connective tissue (Fig. 2C, D). These findings are compatible with pseudoaneurysm. Blood chemistry including coagulation function test and serum immunological screening for rheumatologic disease or vasculitis was all negative. However, low von Willebrand factor (vWF) antigen level and Ristocetin cofactor activity are identified in specialized vWF multimeric analysis which highly suggested acquired vWF deficiency. Transesophageal echocardiography for the detection of any embolic source showed no abnormality, and bone marrow biopsy confirmed the diagnosis of PV. The patient was prescribed low dose aspirin daily and cytotoxic therapy with hydroxyurea, and intermittent phlebotomies were performed. She was discharged 3 weeks after admission with no neurologic symptoms and near normalized hematologic parameters. Follow-up DSA after 6 months showed an improved degree of the stenosis and no sign of regrowth of the pseudoaneurysm (Fig. 2E).
We describe a stroke patient with PV initially presenting with cerebral infarction and pseudoaneurysm rupture. The radiological and laboratory examination were compatible with cerebral infarction and subarachnoid hemorrhage as clinical onset of PV. Previous reports have described ischemic stroke associated with PV, while pseudoaneurysm rupture in PV has not been reported in the literature. Therefore, a systemic infection combined with immunocompromised state in myeloproliferative disorder, traumatic aneurysm, and connective tissue disease such as hereditary hemorrhagic telangiectasia, fibromuscular dysplasia, and Ehlers-Danlos syndrome related to pseudoaneurysm formation also had to be ruled out. Diagnostic evaluation revealed no other possible factor contributing to the formation of a pseudoaneurysm or simultaneous ischemia/hemorrhage.
The natural history of PV is usually marked by significant risk of thrombotic complications68). In patients with thrombocythemia associated with PV, increased hematocrit and whole blood viscosity are believed to trigger increment of shear force at the vessel wall leading to platelet activation and/or platelet/leukocyte-endothelial cell interactions36). These effects increase the possibility of the initiation of thrombus formation and diminished cerebral blood flow in PV. Accordingly, cerebral infarction in current case may be associated with PV as stated above.
On the contrary, a paradoxical, spontaneous bleeding manifestation in PV is often associated with high platelet counts (over 1000×103/µL), platelet dysfunction, and acquired von Willebrand's disease (vWD)13). Mechanical degradation of vWF under high shear stress in patients with PV is one of the possible pathogenetic mechanisms of acquired vWD2). In this case, pseudoaneurysm formation leading to SAH seems to be affected by vWD. Since vWD involves mesenchymal derived structures such as blood vessel, and is related to the development of endothelial defect resulting from depletion of vWF12). Laboratory results support this mechanism by showing that vWF antigen level and Ristocetin cofactor activity decreased in circumstance with high platelet counts (1120×103/µL). Furthermore, intramural hemorrhage with thrombus formation and vessel fragility from increasing shear force to the vessel wall in PV, seem also to be associated with intracranial dissection causing a pseudoaneurysm formation and rupture (SAH) and aggravation of luminal narrowing (cerebral infarction)5).
As current case, PV combined with high platelet counts (over 1000×103/µL) thrombocythemia frequently related to the paradoxical occurrence of microvascular thrombotic complications and hemorrhagic manifestations3). Successful management of the underlying diseases leads to the resolution of bleeding tendency caused by acquired vWD4). In this case, acquired vWD was responded to the treatment of PV with cytotoxic agent, low-dose aspirin, and intermittent phlebotomies. In this situation, daily low-dose aspirin might prevent the thrombotic complications, but would elicit the risk of bleeding tendency indicating the urgent need to lower platelet counts3). Reduction of the platelet counts by cytotoxic agents to less than 1000×103/µL would result in the reduction of hemorrhagic risk and the improvement of acquired vWD as well as the prevention of thrombotic events.
Based on the observation in current case, we suggest that concurrent ischemic and hemorrhagic stroke in patients with PV is extremely rare, and it is important to manage simultaneously underlying hematologic cause and consequent stroke. This case highlights that a probable association between PV and intracranial dissection accompanied by an unusual pseudoaneurysm formation seems plausible, and further study is needed for clarifying this pathophysiologic mechanism.
References
1. Garaci FG, Gandini R, Romagnoli A, Fasoli F, Varrucciu V, Simonetti G. Hepatic artery pseudoaneurysm in von Willebrand's disease. Eur Radiol. 2003; 13:1913–1915. PMID: 12942294.

2. Gupta PK, Kannan M, Chatterjee T, Dixit A, Mahapatra M, Choudhry VP, et al. Acquired von Willebrand's disease associated with gastrointestinal angiodysplasia : a case report. Haemophilia. 2006; 12:452–455. PMID: 16834752.

3. Michiels JJ, Berneman Z, Schroyens W, Koudstaal PJ, Lindemans J, Neumann HA, et al. Platelet-mediated erythromelalgic, cerebral, ocular and coronary microvascular ischemic and thrombotic manifestations in patients with essential thrombocythemia and polycythemia vera : a distinct aspirin-responsive and coumadin-resistant arterial thrombophilia. Platelets. 2006; 17:528–544. PMID: 17127481.

4. Mohri H. Acquired von Willebrand syndrome : its pathophysiology, laboratory features and management. J Thromb Thrombolysis. 2003; 15:141–149. PMID: 14739623.

5. Nakatomi H, Segawa H, Kurata A, Shiokawa Y, Nagata K, Kamiyama H, et al. Clinicopathological study of intracranial fusiform and dolichoectatic aneurysms : insight on the mechanism of growth. Stroke. 2000; 31:896–900.

6. Pearson TC. Hemorheologic considerations in the pathogenesis of vascular occlusive events in polycythemia vera. Semin Thromb Hemost. 1997; 23:433–439. PMID: 9387202.

7. Gruppo Italiano Studio Policitemia. Polycythemia vera : the natural history of 1213 patients followed for 20 years. Ann Intern Med. 1995; 123:656–664. PMID: 7574220.
8. Tefferi A. Polycythemia vera and essential thrombocythemia : 2013 update on diagnosis, risk-stratification, and management. Am J Hematol. 2013; 88:507–516. PMID: 23695894.

Fig. 1
Intracranial imaging. A : Initial head CT scan shows subarachnoid hemorrhage on left basal cistern. Magnetic resonance imaging showing an acute ischemic lesion in the territory of the left middle cerebral artery with restricted diffusion on diffusion-weighted sequences (B and C) and apparent diffusion coefficient map (D and E). Digital subtraction angiography with 3D-reconstructed imaging shows an irregularly shaped aneurysm arising from supraclinoid internal carotid artery with moderate stenosis of proximal region (F), and its delayed opacification (G) and stagnation of contrast medium in the aneurysm sac (arrows) even during the venous phase (H).
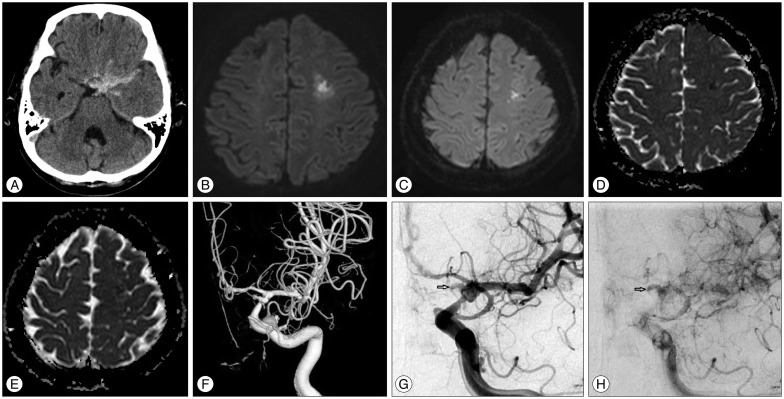
Fig. 2
A : Operative photograph showing a pulsatile, thin walled aneurysm (white arrows) adherent to the adjacent tissue in the anterior wall of supraclinoid internal carotid artery (black arrow), optic nerve (thick arrow). B : Three curved clips were applied with a crosswise fashion to close the torn gap and to maintain patency of the parent vessel. C and D : Aneurysmal body was composed of organized blood clot (black arrow) and recent thrombus (white arrow) surrounded by fibrous connective tissue (arrowheads) (hematoxylin-eosin stain & Masson-trichrome stain, original magnification ×12.5). E : Follow-up digital subtraction angiography at 6 months after surgery reveals no sign of regrowth of the pseudoaneurysm and an improved degree of the stenosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download