Abstract
Tumors of the clivus and metastases to the clivus are very rare. Metastasis involving the clivus has previously been described in only two case reports. In skull metastasis, the breast and prostate are the most common primary foci, while metastasis from gastric carcinoma is extremely rare. A review of the English literature revealed only one published case of clivus metastases from gastric adenocarcinoma. There is no literature thoroughly explaining the differential diagnosis between chordoma and metastasis. Here we report a rare case of metastasis to the clivus from a gastric adenocarcinoma in a 42-year-old female patient with sudden blurry vision, presenting as bilateral cranial nerve VI palsy.
Tumors of the clivus are very rare; chordomas are the most common type of tumors in this region, representing only 0.1-0.2% of all intracranial tumors9). Common sources of bone metastases are breast, prostate, kidney, and thyroid tumors. Kistler and Pribram8) reported 11 cases with metastatic disease in the sella turcica originating from prostate, breast, lung, thyroid, or lymphosarcoma malignancies. Metastasis from gastric adenocarcinoma is extremely rare and could be explained by a rapid progression of the gastric adenocarcinoma. With regard to sites of intracranial metastasis, the clivus is a rare site. A literature review revealed only two case reports5,6) of clival metastasis from stomach cancer. To the best of our knowledge, this is the second published English case report of skull base metastasis originating from a gastric adenocarcinoma.
In this study, we report the case of a 42-year-old female patient with an adenocarcinoma of the stomach that metastasized to the clivus.
A 42-year-old female patient was admitted to our hospital with 1-month history of headaches, nausea, and vomiting. In the previous month, she had lost 2 kg of weight. She had also experienced diplopia, bilateral orbital pain, and gaze disturbance. Physical examination revealed bilateral palsy of the third and sixth cranial nerve. Laboratory examination detected abnormally elevated levels of the alpha feto-protein (1665 ng/mL), carcinoembryonic antigen (1493 ng/mL), and carbohydrate antigen 19-9 (695 U/mL). Results of other hematological, biochemical, and urine examinations were normal.
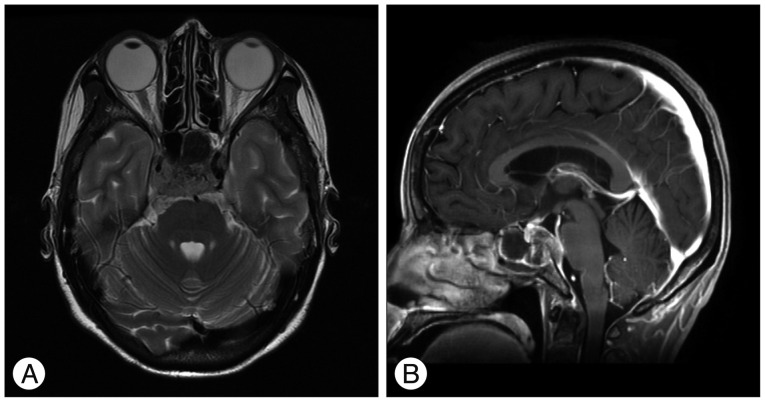
A computed tomography (CT) scan of the brain showed a bulging bony mass, which had destroyed the clivus and affected the sphenoid and cavernous sinuses (Fig. 1). Magnetic resonance imaging (MRI) scan showed an abnormal mass in the upper portion of the clivus, extending to the cavernous sinus and invasion into both carotid arteries. The mass showed cystic change and heterogeneous patterns of enhancement after intravenous injection of gadolinium (Fig. 2).
On T1-weighted MRI, a mass (approximate diameter, 2.7× 1.6×2.0 cm) was detected in the sellar region. The mass involved the sphenoid sinus, cavernous sinus, both internal carotid arteries, and the optic chiasm, but had destroyed the clivus and sphenoid corpus.
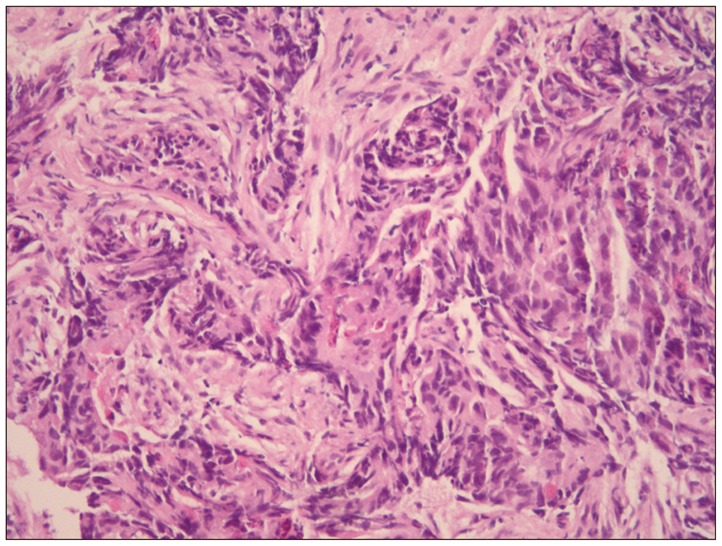
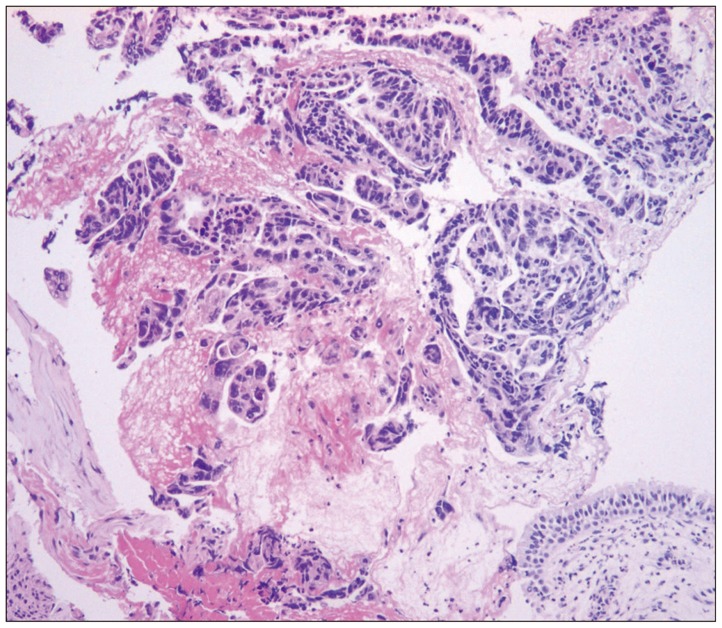
An abdominal CT scan suggested gastric cancer with liver and multiple lymph node (LN) metastases. A fiber endoscopic study of the stomach confirmed advanced cancer with poor differentiation at the cardia (Fig. 3). Lumbar puncture yielded a watery-clear fluid but the cerebrospinal pressure was not increased and subsequent cytological examination of the fluid revealed no malignant cells. A chest CT scan showed left supraclavicular lymphadenopathy, indicative of metastasis.
For diagnostic purposes, a punch biopsy was performed via the transnasal-transsphenoidal route. Histopathological findings of this biopsy were similar to those obtained from the tumor of the stomach (Fig. 4). Therefore, the diagnosis was confirmed as clival metastasis from gastric adenocarcinoma. The immunohistochemical analysis of the stomach specimen revealed negative results for mucin 5AC, mucin 6, and mucin 2 on a mucin stain and a positive result for the CD10 protein, which was similar to the results obtained for intestinal-type adenocarcinoma and for clivus metastasis.
External beam radiotherapy into the skull and chemotherapy were used to treat the patient. After three cycles of chemotherapy [FOLFOX : folinic acid (leucovorin), fluorouracil (5-FU), and oxaliplatin (Eloxatin)], the patient's condition deteriorated rapidly; liver and LN metastasis progressed, and she developed tumor thrombosis at the splenoportal and superior mesenteric veins and cancer peritonei. She died 6 months after metastasis to the clivus was detected.
The clivus is a single midline structure of bone comprising a part of the skull base and is formed from the sphenoid rostrally and the occiput caudally. Both benign or malignant primary tumors as well as secondary metastatic tumors may occur at the clivus. Some lesions that specifically involve the clivus are chordomas, chondrosarcomas, or lymphomas3,11).
A chordoma is a rare, slow-growing tumor that originates from remnants of the primitive notochord along the craniospinal axis, particularly at either end. Cranial chordomas constitute less than 1% of all intracranial neoplasms, and patients can present with headaches and diplopia11).
Metastasis to the clivus is very rare, and only few cases have previously been reported4). Hematogenesis is the most common route of metastasis, and most clival metastatic lesions arise from prostate, thyroid, or breast cancers13). Diplopia and headaches are the most common symptoms of sixth nerve palsy. Palsy of the sixth cranial nerve is usually progressive and rarely improves after surgery. This is in contrast to chordomas, where surgical decompression commonly results in improvements in eye movement1).
MRI and CT scans have complementary roles in the evaluation of clival tumors. CT evaluation is required to assess the degree of bone involvement or destruction and to detect patterns of calcifications within the lesion. MRI scans provide excellent 3-dimensional analysis of the posterior fossa, especially the brainstem, sella turcica, cavernous sinuses, and middle cranial fossa. CT is better than MRI to observe calcifications and the precise involvement of skull base osteolysis, especially those at the skull base foramina2).
Three-dimensional gradient-echo T1-weighted sequences are helpful because they allow the tumor to be visible in 3 planes within a short time and allow a good signal analysis of the tumor2).
The radiological findings of clivus metastasis are not characteristic. Therefore, a differential diagnosis of chordoma and chondrosarcoma may be difficult1). Skull base chordomas are well delineated at the outset because they displace adjacent structures; however, more advanced tumors become invasive and have a pseudomalignant appearance with bone erosion and soft tissue invasion, mimicking malignant clival tumors including metastasis2).
One feature that may help distinguish metastases from chordoma-like tumors is hypo-intensity on T2-weighted MRI images; this would be possible because of the higher cellular density and lower cytoplasm to nuclear ratio in metastases12). Most chordomas exhibit a high-intensity signal on T2-weighted images, which is nonspecific. Fluid and gelatinous mucoid substances associated with recent and old hemorrhage and necrotic areas are found within the tumor; in some patients, calcification and sequestered bone fragments are found as well. The variety of these components may explain the signal heterogeneity observed on an MRI scan. Incomplete delineation of the tumor and microscopic distal extension of tumor cells may explain the frequency of recurrences2).
On imaging, other primary tumors of the clivus show findings similar to those of metastases of the skull. Lymphoma and plasmacytoma of the clivus, for example, may show a similar MRI signal on T2-weighted images7).
Another useful diagnostic indication on an MRI scan that may help distinguish chordomas from metastases is the heterogeneity with a honeycomb appearance shown by chordomas in lobulated areas, corresponding to low-intensity T1-signal areas within the tumor after contrast infusion. The pattern of contrast enhancement can be related to the pathologic features of the chordoma, which is organized in lobules with mucinous and gelatinous contents2).
In patients without a history of cancer, metastasis to the clivus occurring as the first indication of a primary neoplasm is difficult to identify. In addition, delayed clivus metastases are difficult to detect13). Pallini et al.12) reported metastasis to the clivus from a cutaneous melanoma 8 years after the primary tumor was detected, and Altman et al.1) described a single metastasis to the clivus that presented 12 years after treatment of a follicular thyroid carcinoma.
Our patient showed symptoms of cranial nerve palsy as the first sign of metastasis, prior to the diagnosis of the primary stomach malignancy.
The treatment of clival metastasis depends on the histology of the primary tumor.
The overall prognosis of patients with clival metastases is very poor, with a median overall survival of about 2.5 years. Cranial nerve palsies are associated with a poorer prognosis, with an average survival of only 5 months10).
References
1. Altman KW, Mirza N, Philippe L. Metastatic follicular thyroid carcinoma to the paranasal sinuses : a case report and review. J Laryngol Otol. 1997; 111:647–651. PMID: 9282206.

2. Doucet V, Peretti-Viton P, Figarella-Branger D, Manera L, Salamon G. MRI of intracranial chordomas. Extent of tumour and contrast enhancement : criteria for differential diagnosis. Neuroradiology. 1997; 39:571–576. PMID: 9272494.

3. Géhanne C, Delpierre I, Damry N, Devroede B, Brihaye P, Christophe C. Skull base chordoma : CT and MRI features. JBR-BTR. 2005; 88:325–327. PMID: 16440571.
4. Greenberg HS, Deck MD, Vikram B, Chu FC, Posner JB. Metastasis to the base of the skull : clinical findings in 43 patients. Neurology. 1981; 31:530–537. PMID: 6972014.

5. Harada S, Toya S, Iisaka Y, Ohtani M, Nakamura Y. [Basal skull metastasis of stomach cancer presenting with Garcin's syndrome--a case report]. No Shinkei Geka. 1987; 15:765–769. PMID: 3670546.
6. Hirai O, Kikuchi H, Hashimoto N. Skull base metastasis from gastric cancer--case report. Neurol Med Chir (Tokyo). 1992; 32:908–910. PMID: 1282684.
7. Jung CS, Zimmermann M, Seifert V. Clivus lymphoma. Acta Neurochir (Wien). 2004; 146:533–534. PMID: 15118895.

8. Kistler M, Pribram HW. Metastatic disease of the sella turcica. Am J Roentgenol Radium Ther Nucl Med. 1975; 123:13–21.

9. Korten AG, ter Berg HJ, Spincemaille GH, van der Laan RT, Van de Wel AM. Intracranial chondrosarcoma : review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry. 1998; 65:88–92. PMID: 9667567.

10. Laigle-Donadey F, Taillibert S, Martin-Duverneuil N, Hildebrand J, Delattre JY. Skull-base metastases. J Neurooncol. 2005; 75:63–69. PMID: 16215817.

11. Movsas TZ, Balcer LJ, Eggenberger ER, Hess JL, Galetta SL. Sixth nerve palsy as a presenting sign of intracranial plasmacytoma and multiple myeloma. J Neuroophthalmol. 2000; 20:242–245. PMID: 11130748.

12. Pallini R, Sabatino G, Doglietto F, Lauretti L, Fernandez E, Maira G. Clivus metastases : report of seven patients and literature review. Acta Neurochir (Wien). 2009; 151:291–296. discussion 296. PMID: 19259614.
13. Ulubaş B, Ozcan C, Acka G, Aydn O, Saritaş E. Clivus metastasis of squamous cell carcinoma : a rare location. J Clin Neurosci. 2005; 12:97–98. PMID: 15639426.
Fig. 1
A : Pre-contrast axial computed tomography (CT) scan showing a calcified mass in the sellar region. The involvement of the sphenoid and cavernous sinuses and the destruction of the clivus. B : Post-contrast axial CT scan after contrast injection demonstrating heterogeneous enhancement with invasion into both carotid arteries.
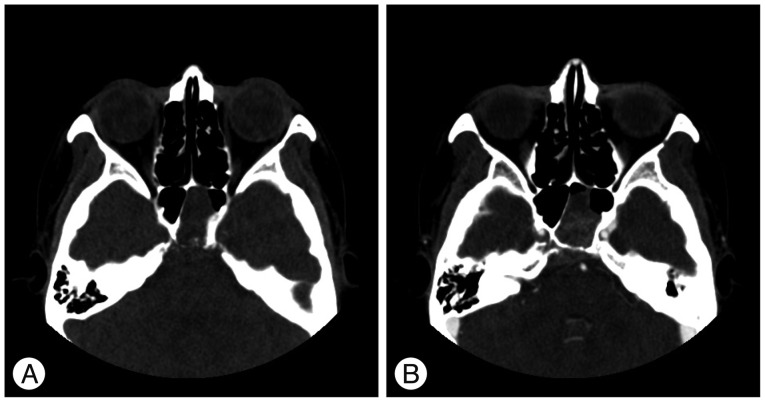
Fig. 2
A : Axial T2-weighted image showing a heterogeneous, hypo-intense, space-occupying lesion at the level of the clivus, invading into the cavernous and sphenoid sinuses and both carotid arteries. B : T1-weighted sagittal images after contrast administration showing heterogeneous enhancement and a cystic portion within the mass. The neoplastic tissue that replaced the normal fatty bone marrow and infiltrated the dura.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download