Abstract
The authors report a case of symptomatic epidural gas accumulation 2 weeks after the multi-level lumbar surgery, causing postoperative recurrent radiculopathy. The accumulation of epidural gas compressing the dural sac and nerve root was demonstrated by CT and MRI at the distant two levels, L3-4 and L5-S1, where vacuum in disc space was observed preoperatively and both laminectomy and discectomy had been done. However, postoperative air was not identified at L4-5 level where only laminectomy had been done in same surgical field, which suggested the relationship between postoperative epidural gas and the manipulation of disc structure. Conservative treatment and needle aspiration was performed, but not effective to relieve patient's symptoms. The patient underwent revision surgery to remove the gaseous cyst. Her leg pain was improved after the second operation.
Free air in the spinal canal has been presented in a number of situations, but it is rare for patients to develop symptomatic epidural gas (EG) after spinal surgery. Only 3 cases of EG, after surgery on the lumbar spine followed by the operative procedure, have been reported in the literature2,8,17), but pathogenetic mechanism is still unclear so far.
The aim of this report is to alert the neurosurgeons to this potential complication, demonstrate the radiological imaging findings, especially the combined use of computed tomography (CT) and magnetic resonance imaging (MRI), in symptomatic spinal EG, following an open discectomy, and to reconsider the pathogenetic mechanism of postoperative EG in association with the vacuum phenomenon. To the best of our knowledge, this is the first case of postoperative symptomatic EG, which occurred in the distant two levels, simultaneously, after lumbar microdiscectomy. This case was illustrated by both CT and MRI.
A 68-year-old woman was presented with lower back pain and radiating pain to the anterior aspect of her left thigh and calf. CT scan showed stenosis in L3-4, herniated disc and vacuum within the disk space in L2-3 and L5-S1 where scattered gas was also observed in the extruded disc of both levels (Fig. 1A, B). MR examination confirmed the disk herniation and also exhibited the signal void areas consistent with the gas in L2-3, L5-S1 levels, but not in L3-4 level (Fig. 1C).
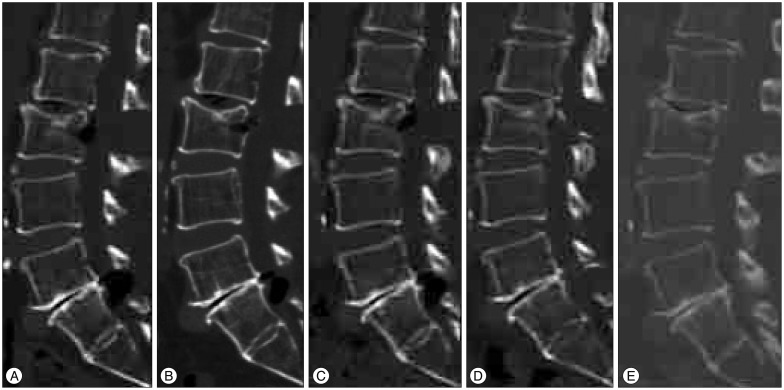
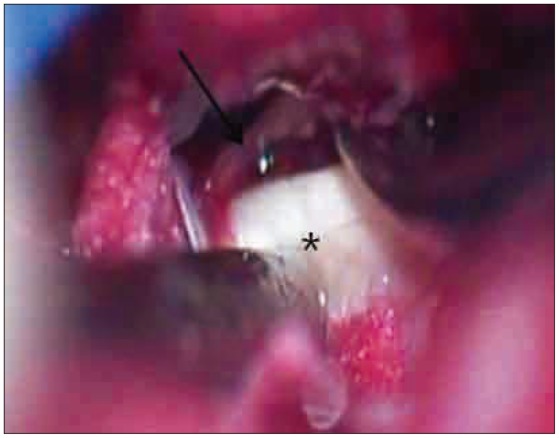
She underwent a partial hemilaminectomy, foraminotomy at L2-3, L3-4, L5-S1 three levels, and discectomy at only L2-3 and L5-S1 two levels. Her symptoms resolved during the postoperative period, but she returned to the hospital 2 weeks after discharge, with complaints of recurrent preoperative symptom. She was re-evaluated clinically and with imaging studies, including radiography, CT, and MR imaging. Her leg pain was similar to what she had experienced before the surgery. However, contrary to the previous symptoms, the patient complained of the aggravation of symptoms with weight-bearing. Partial relief of pain was gained while patient was sitting and recumbency. There was no motor or sensory deficit. Laboratory studies to rule out the possibility of infection showed no abnormal finding. Radiographs showed the narrowing of the L2-3 and L5-S1 disk space, vacuum phenomenon and post-laminectomy defect. Minimal dynamic instability was seen in L2-3 level. MR image showed epidural, signal void, space-occupying, cyst-like lesions in L2-3 and L5-S1 level, which suggested air or calcified disk fragment. Granulation tissue around the gas was observed in the surgery site (Fig. 2A). A subsequent non-contrast CT of the lumbar spine confirmed well-defined, ovoid air-attenuation in the epidural space in L2-3 and L5-S1 level (Fig. 2B). The gas was compressing the dural sac and right L3 and left S1 nerve root. The patient received conservative treatment, including absolute bed rest (ABR), steroid, nonsteroidal anti-inflammatory drug medication for 2 weeks, but her neurologic condition did not improve. Follow-up CT revealed the increased amount of EG (Fig. 3A).
Needle aspiration was performed in L2-3 and L5-S1 level under the fluroscopic guidance. Post-procedural CT showed decreased amount of EG in both levels (Fig. 3B). Temporary relief of pain was achieved for 2 days, but she complained of recurrence of the symptoms. CT scan, which was taken 1 week after the aspiration of gas, revealed the amount of epidural gas was increased again in both levels (Fig. 3C). Open revision surgery was advised.
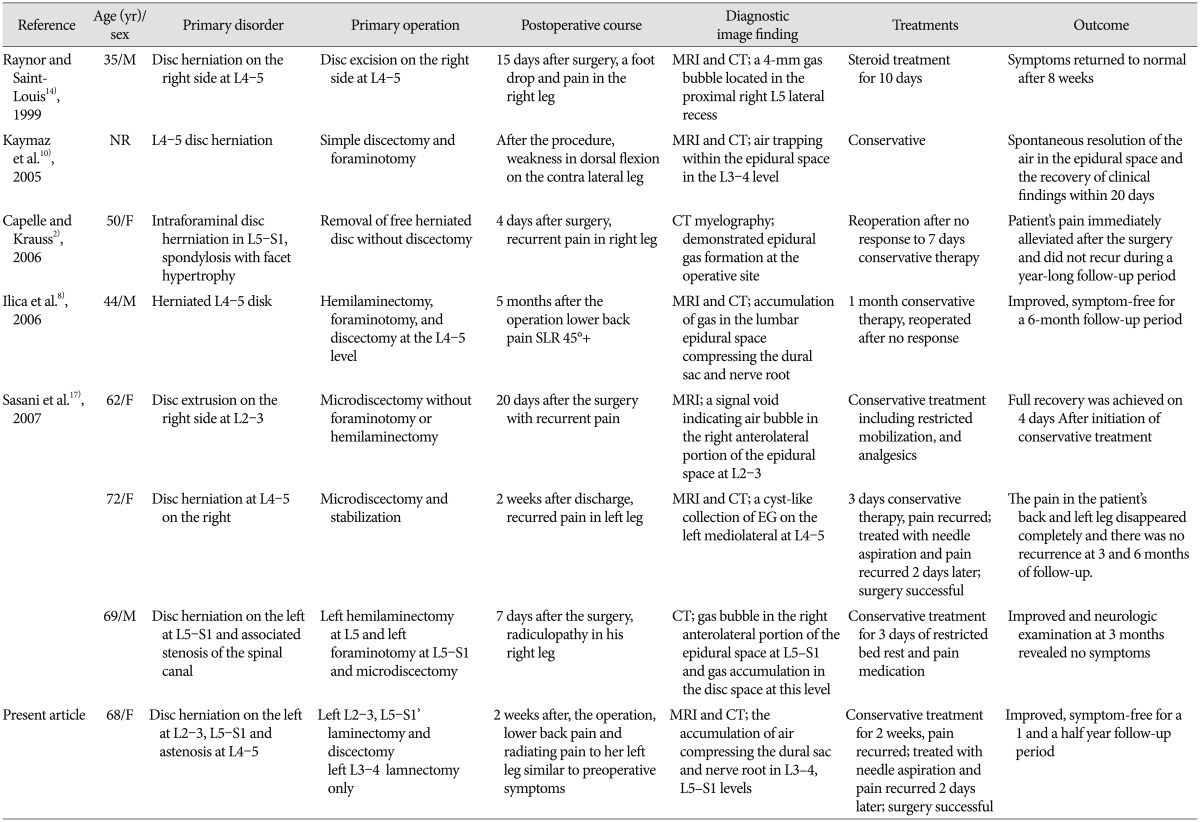
During the surgery, no herniated disk was found and gas pocket surrounded by a thin, blister like membranous structure was observed at the inferolateral portion of roots in L2-3, and L5-S1 levels (Fig. 4). Total removal of cystic structure and curettage of remnant soft tissue, as well as further discectomy in disc space were done. Surgical field, including intradiscal space was irrigated with isotonic saline at the last stage of the operation. The postoperative period was uneventful and the patient's previous symptom disappeared completely. Immediate postoperative CT revealed disappearance of gas in epidural space (Fig. 3D). Ambulation with brace was recommended for the patient. Follow-up lumbar CT taken after 1 year from the last operation showed no epidural gas (Fig. 3E). The patient remained symptom-free for 1 and a half year follow-up period.
Free air in the spinal canal has been reported in a number of situations, including craniocervical trauma, epidural anesthesia, and percutaneous spinal procedure. Other local structures and processes, such as inter-apophyseal joints, thoracic surgery, pneumothorax, penetrating chest wounds, intestinal necrosis, pyogenic infections produced by gas-forming organisms and osteonecrosis, are another potential source of gas in the spinal canal3,6,7,8,12). In most cases, the gas formation in the spinal canal is associated with disc herniation12,13), but isolated so-called pseudocyst have also been reported4,12,13).
Spinal surgery can be one of the causes of EG. Postoperative EG formation causing a severe radicular pain, however, is very unusual. As mentioned, the current literature documents 7 cases of symptomatic EG after lumbar microdiscectomy. Three of these patients have undergone a revision surgery for the removal of gas (Table 1)1,2,8,17).
Pathogenetic mechanisms of postoperative EG are still unknown. A few hypothesis were introduced to explain postoperative gas formation in the spinal canal. Sasani et al.17) suspected that, in cases of postoperative symptomatic EG, air becomes trapped during the surgical procedure within the soft tissue when blood in the surgical field causes soft tissue margins to bind. They thought that this "closure" eventually leads to the formation of a membrane that encases the gas collection. But, in the current case, postoperative MRI taken just 1 day after the primary operation didn't show any significant sign of air bubble in the spinal canal. By this radiological finding, it can be assumed that postoperative intraspinal air was originated from the spinal structure itself, not by air trapping during the operation. They might be formed insidiously sometime after the operation and had a relationship with the removal of the disc.
Intraspinal air was thought to have the relationship with vacuum phenomenon by many authors5,6). Some authors demonstrated the existence of communication between the intradiscal gas and the intraspinal gas by confirming the flow of contrast media into the pseudocyst using a CT after discography9,13). Intradiscal gas can migrate into the epidural space, through this communication, as a result of normal movements of the lumbar spine acting as a piston, and this can, albeit infrequently, lead to nerve root compression20).
In this case, postoperative intraspinal air was seen just only in the L2-3 and L5-S1 levels, where the preoperative intradiscal vacuum phenomenon had been shown and a discectomy was performed, but not in the L3-4 level where only a laminectomy had been done and preoperative intradiscal air was not seen. Authors also could find some scattered gas, which had already been in the extruded disc in L2-3 and L5-S1 levels. These findings correspond to previous reports that the presence of the gas in the intervertebral disk was at the same level as the postoperative bubble2,8), and support the hypothesis of vacuum phenomenon as the cause of postoperative EG, as other authors mentioned. We suggest that annular tear, which had already existed and had the role of the channel between intradiscal and epidural space, was enlarged by a discectomy procedure during the operation, and intradiscal air was expelled to the spinal canal through this channel more easily. It caused postoperative intraspinal air trapping.
Regarding the characteristics of recurred pain, aggravation of symptoms when weight-bearing, while sitting and recumbency are associated with pain relief, was also observed in this case, as previous reports had described4,18). The mechanism of reversible root compression was thought to be a back and forth movement of air through the channel by a piston-like pneumatic compression, and distraction of the vertebral body in a closed system consist of intradiscal space and encapsulated cyst. This mechanism could be the rationale for ABR and immobilization with brace which was done in this case as the one of the therapeutic strategies for this complication.
There is another question that still remains. It's why the amount of gas in the spinal canal increased again after the needle aspiration and previous symptom recurred after just 2 days. Some authors mentioned the "valve-pump mechanism" or "ball-valve effect" as the cause of increased amount of gas in the spinal canal15,20). If the total amount of the air in disc space and spinal canal is constant, the air movement from disc space to spinal canal would lead to decreased amount of intradiscal air by this mechanism. However, based on the imaging data when symptom recurred after the aspiration procedure, the amount of intradiscal air was not decreased, even seemed to be a little bit increased. It means more intradiscal gas had been being produced since the needle aspiration, and there is another mechanism to make further gas formation in the disc space. The vacuum phenomenon is explained by several physiologic and anatomic factors. Various reported observations have demonstrated or suggested the reversible formation and absorption of gas and fluid in the disc space11,15,19,20). Biomechanically, negative pressure is produced by enlarging the clefts in the disc that attracts gas from the surrounding extracellular spaces6). Authors assume that in company with normal movement of the lumbar spine, leakage of intradiscal gas to the spinal canal can contribute to this negative pressure in disc space, which could lead to further recruitment of gas in the disc space, which results in a more accumulation of gas in the spinal canal in conjunction with "valve-pump mechanism". This assumption should be further investigated and considered on the biomechanical and physiologic background, which was mentioned above in order to understand the exact pathogenesis of postoperative EG in the spinal canal.
Treatment options for postoperative intraspinal air range from nonoperative to operative, depending on the clinical symptoms presented. Based on the current case and those previously reported, we think that conservative management should always be attempted first, when clinical signs of EG appear after lumbar surgery. As noted, postoperative EG may resolve spontaneously with time9,10). But, if the patient does not improve with conservative treatment, more invasive procedure, including the needle aspiration, or surgery, is needed.
Needle aspiration is one of the therapeutic options, but was reported to have the chance of recurrence1,16,20). Some authors stressed complete removal of the cyst wall as the preventive measure of recurrence of air collection. Just simple aspiration of the air, through the encapsulated cyst, seems not to be enough to resolve this problem because the closed system formed by encapsulated cyst and intradiscal space may not be collapsed, and air could be collected in the pseudocyst again. Some authors also suggest the presence of granulation tissue surrounding the epidural gas is a predictor for surgery. Authors think it's in line with this closed system concept8). Open surgery is most reliable in cases where there is no response to conservative therapy, and is definitely required to remove chronic encapsulated air and the cyst wall totally, and break this closed system1,16). Although further gas was formed in the spinal canal, it may be absorbed by the adjacent soft tissue after the removal of the cyst wall. Other authors suggested that the treatment needs to be targeted to the disc, as well as the gaseous cyst, and recommended ensuring adequate foraminotomy, carefully removing the membranous soft tissue near the nerve root during the operation in order to prevent reaccumulation or persistence of air in the lumbar epidural space16,20). Irrigating the surgical field well with isotonic saline and longer stay of the drain, postoperatively, during the revision surgery was also mentioned as surgical tips10). The ABR and immobilization with brace to restrict the motion in pathologic segments are also advisable, in order to lower the chances of radicular compression by the re-accumulation of the air.
Although symptomatic EG is rare clinically, it should be considered as one of the possible causes for postoperative radiculopathy. Combined use of CT and MRI is helpful to diagnose the EG in the spinal canal, and differentiate other pathological lesions. Open revision surgery is the most reliable method to treat the postoperative EG, by removing the encapsulated cyst wall totally if conservative treatment fails.
References
1. Bosser V, Dietemann JL, Warter JM, Granel de Solignac M, Beaujeux R, Buchheit F. L5 radicular pain related to lumbar extradural gas-containing pseudocyst. Role of CT-guided aspiration. Neuroradiology. 1990; 31:552–553. PMID: 2352640.

2. Capelle HH, Krauss JK. Recurrent sciatica due to periligamentous trapped epidural gas after spinal sequestrectomy. J Neurosurg Spine. 2006; 4:75–77. PMID: 16506470.

3. Charles RW, Mody GM, Govender S. Pyogenic infection of the lumbar vertebral spine due to gas-forming organisms. A case report. Spine (Phila Pa 1976). 1989; 14:541–543. PMID: 2727800.

4. Cheng TM, Link MJ, Onofrio BM. Pneumatic nerve root compression : epidural gas in association with lateral disc herniation. Report of two cases. J Neurosurg. 1994; 81:453–458. PMID: 8057154.

5. Ford LT, Gilula LA, Murphy WA, Gado M. Analysis of gas in vacuum lumbar disc. AJR Am J Roentgenol. 1977; 128:1056–1057. PMID: 414544.

6. Gulati AN, Weinstein ZR. Gas in the spinal canal in association with the lumbosacral vacuum phenomenon : CT findings. Neuroradiology. 1980; 20:191–192. PMID: 7465037.

7. Hidalgo-Ovejero AM, García-Mata S, Gozzi-Vallejo S, Izco-Cabezón T, Martínez-Morentín J, Martínez-Grande M. Intradural disc herniation and epidural gas : something more than a casual association? Spine (Phila Pa 1976). 2004; 29:E463–E467. PMID: 15480124.
8. Ilica AT, Kocaoglu M, Bulakbasi N, Kahraman S. Symptomatic epidural gas after open discectomy : CT and MR imaging findings. AJNR Am J Neuroradiol. 2006; 27:998–999. PMID: 16687531.
9. Kakitsubata Y, Theodorou SJ, Theodorou DJ, Yuko M, Ito Y, Yuki Y, et al. Symptomatic epidural gas cyst associated with discal vacuum phenomenon. Spine (Phila Pa 1976). 2009; 34:E784–E789. PMID: 19934800.

10. Kaymaz M, Oztanir N, Emmez H, Ozköse Z, Paşaoğlu A. Epidural air entrapment after spinal surgery. Clin Neurol Neurosurg. 2005; 107:421–424. PMID: 16023539.

11. Malghem J, Maldague B, Labaisse MA, Dooms G, Duprez T, Devogelaer JP, et al. Intravertebral vacuum cleft : changes in content after supine positioning. Radiology. 1993; 187:483–487. PMID: 8475295.

12. Mortensen WW, Thorne RP, Donaldson WF 3rd. Symptomatic gas-containing disc herniation. Report of four cases. Spine (Phila Pa 1976). 1991; 16:190–192. PMID: 2011775.

13. Pak KI, Hoffman DC, Herzog RJ, Lutz GE. Percutaneous intradiscal aspiration of a lumbar vacuum disc herniation : a case report. HSS J. 2011; 7:89–93. PMID: 22294964.

14. Raynor RB, Saint-Louis L. Postoperative gas bubble foot drop. A case report. Spine. 1999; 24:299–301. PMID: 10025027.
15. Ricca GF, Robertson JT, Hines RS. Nerve root compression by herniated intradiscal gas. Case report. J Neurosurg. 1990; 72:282–284. PMID: 2295923.
16. Righini A, Lucchi S, Reganati P, Zavanone M, Bettinelli A. Percutaneous treatment of gas-containing lumbar disc herniation. Report of two cases. J Neurosurg. 1999; 91(1 Suppl):133–136. PMID: 10419361.
17. Sasani M, Ozer AF, Oktenoglu T, Cosar M, Karaarslan E, Sarioglu AC. Recurrent radiculopathy caused by epidural gas after spinal surgery : report of four cases and literature review. Spine (Phila Pa 1976). 2007; 32:E320–E325. PMID: 17471081.
18. Tsitouridis I, Sayegh FE, Papapostolou P, Chondromatidou S, Goutsaridou F, Emmanouilidou M, et al. Disc-like herniation in association with gas collection in the spinal canal : CT evaluation. Eur J Radiol. 2005; 56:1–4. PMID: 16168257.

19. Wang HJ, Chen BB, Yu CW, Hsu CY, Shih TT. Alteration of disc vacuum contents during prolonged supine positioning : evaluation with MR image. Spine (Phila Pa 1976). 2007; 32:2610–2615. PMID: 17978662.
20. Yoshida H, Shinomiya K, Nakai O, Kurosa Y, Yamaura I. Lumbar nerve root compression caused by lumbar intraspinal gas. Report of three cases. Spine (Phila Pa 1976). 1997; 22:348–351. PMID: 9051898.
Fig. 1
Preoperative sagittal CT and magnetic resonance imaging findings. A sagittal computed tomography (A : L2-3, B : L5-S1) and magnetic resonance image (C) reveal disc herniation containing air in L2-3, L5-S1 level. Vacuum phenomenon is also noted within intervertebral disk space in L2-3, L5-S1 level.

Fig. 2
Postoperative sagittal computed tomography and magnetic resonance imaging findings (2 weeks after the first operation). A : A sagittal T2-weighted magnetic resonance image demonstrates a signal void compressing thecal sac and nerve roots at L3 body and L5-S1 disc level. Granulation tissue (arrow) around the cyst is seen. B : A sagittal computed tomography shows the mass of low density indicating air bubble at L3 body and L5-S1 disc level.
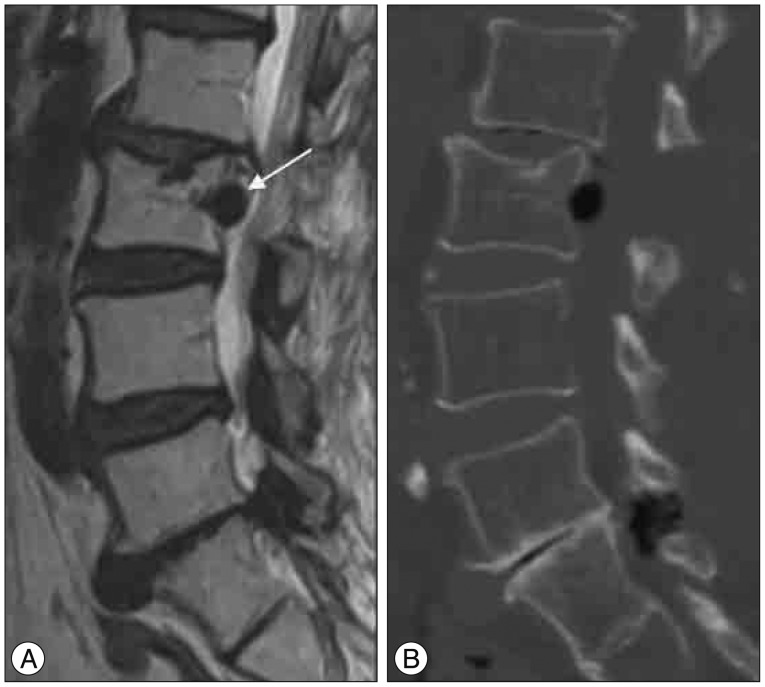
Fig. 3
Series of computed tomography finding. A : Postoperative computed tomography imaging findings (2 weeks after the first operation). B : Computed tomography imaging (after needle aspiration) : the amount of epidural gas was decreased. C : Computed tomography imaging (1 week after the needle aspiration) : the amount of epidural gas increased again. D : Computed tomography imaging findings (after the revision surgery). E : Computed tomography imaging findings (1 year after the revision surgery).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download