Abstract
If a ruptured blood blister-like aneurysm (BBA) arises from the lateral or superolateral wall of the internal carotid artery (ICA) at the level of the anterior choroidal artery (AChA), its proximity to the origin of the AChA presents a serious surgical challenge to preserve the patency of the AChA. Two such rare cases are presented, along with successful surgical techniques, including the application of a C-shaped aneurysm clip parallel to the ICA and a microsuture technique to repair the arterial defect. The patency of the AChA and ICA was successfully preserved without recurrence or rebleeding of the BBA during a 1-year follow-up after the operation.
Most blood blister-like aneurysms (BBAs), which are small fragile, hemispheric bulges at nonbranching sites of the supraclinoid internal carotid artery (ICA), arise from the superior or superomedial wall of the ICA apart from the anterior choroidal artery (AChA) origin1,3,10,17,19,22,25). However, if a BBA arises from the lateral or superolateral wall of the ICA at the level of the AChA, it is located close to the origin of the AChA. Based on preoperative angiograms, recognition of a BBA adjacent to the AChA origin is difficult. In addition, such a BBA presents a serious surgical challenge to preserve the patency of the AChA. Trapping the ICA or using encircling techniques, such as encircling clip placement and clip placement on wrapping material, is not appropriate to preserve the patency of the AChA.
Therefore, the author reports on 2 such cases of BBAs located close to the AChA origin and their successful treatment by direct surgical repair without compromising the AChA.
A 68-year-old man presented with a sudden headache, and an immediate computed tomography (CT) scan showed scanty subarachnoid hemorrhage (SAH) in the left carotid cistern and sylvian fissure. Subsequent digital subtraction angiography (DSA) revealed an ill-defined slight bulging in the lateral wall of the left ICA at the level of the AChA (Fig. 1A). Then, exploratory pterional craniotomy was then performed based on a diagnostic suspicion of a BBA.
Opening of the carotid and proximal sylvian cisterns in a pterional craniotomy exposed the supraclinoid ICA. A red friable bulge was found in the superolateral wall of the ICA at the level of the AChA. The AChA emitted from a lateral wall of the ICA close to the BBA. After temporary clipping of the proximal ICA, a right-angled aneurysm clip was applied to the lesion parallel to the ICA to catch part of the normal arterial wall. While this clipping produced minor stenosis of the ICA, but the rupture point was secured (Fig. 1B). The superolateral location of the BBA on a left ICA required the clip to be applied using the left hand.
The postoperative recovery was uneventful. The postoperative and 1-year follow-up angiograms confirmed the preservation of the AChA without any recurrence of the BBA (Fig. 1C).
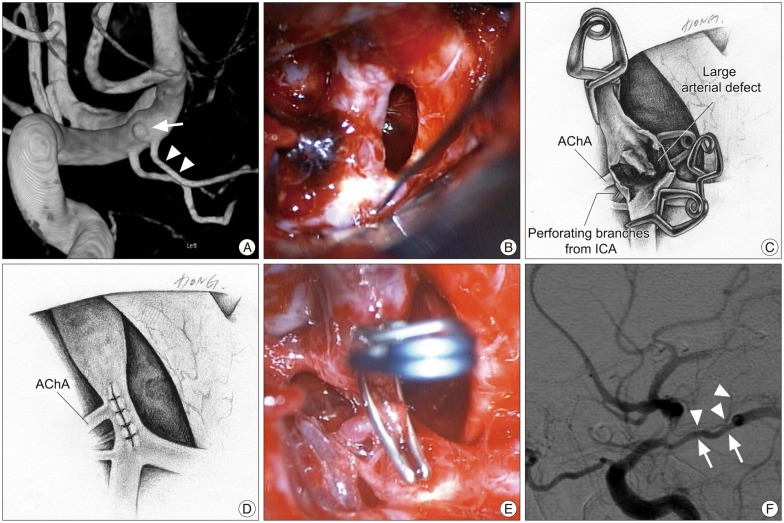
A 53-year-old man presented with a sudden severe headache and drowsy mentality. An immediate CT scan revealed a diffuse, thick subarachnoid hemorrhage in the basal cisterns. In a subsequent DSA, a very small aneurysmal lesion was noticed in the lateral wall of the distal ICA close to the AChA origin. As it had a small, hemispherical contour and located superior to the AChA origin, rather than distal to it, a BBA was suspicious (Fig. 2A). Also, associated focal dilatation of the ICA around the hemispherical bulge increased the diagnostic suspicion of a BBA. As good collateral circulation was shown through the anterior and posterior communicating arteries, the crucial surgical goal was preserving the patency of an AChA in addition to close the rupture point of an ICA.
Using a left pterional craniotomy, the affected ICA was exposed by opening the carotid cistern and proximal sylvian fissure. The superior half of the circumference of the distal ICA appeared abnormal. The lateral wall of the distal ICA was covered by a blood clot, suggesting a rupture point, while the superior and medial walls were very thin and friable (Fig. 2B). Slight manipulation of the medial wall of the ICA to obtain proximal control of the posterior communicating artery (PCoA) via an opticocarotid triangle led to iatrogenic rupture of the superomedial wall of the ICA. Thus, the rupture point was temporarily closed using a curved aneurysm clip, and then attention was paid to the primary rupture point in the lateral wall. After temporary clipping of the proximal ICA and PCoA, the blood clot covering the rupture point was cleared to demarcate the arterial defect and the adjacent AChA. The arterial defect was very close and just superior to the AChA origin. An attempt to suture the defect was failed due to the friable superior wall that was torn. When the curved aneurysm clip was removed, a large round arterial defect was finally revealed (Fig. 2C). At this point, a Yasargil aneurysm clip with C-shaped blades (Aesculap Instruments Corp., Tuttlingen, Germany), model FT 824T was applied parallel to the ICA to close the large, round arterial defect, yet this also failed to stop the leakage despite severe luminal stenosis of the ICA. Therefore, the large arterial defect of the ICA was approximated using four stitches with an 8-0 monofilament, resulting in an hourglass appearance due to severe stenosis (Fig. 2D). The suture line was then reinforced using the Yasargil aneurysm clip with C-shaped blades, thereby preserving the AChA (Fig. 2E). Intraoperative Doppler was used to ascertain the patency of the AChA, PCoA, and ICA.
The patient recovered without neurological deficits and returned to his previous life. The postoperative and 6-month follow-up angiograms revealed severely stenotic distal ICA, excellent patency of the PCoA and AChA, and no recurrence of the BBA (Fig. 2F), along with good collateral circulation through the anterior communicating artery to the middle cerebral artery.
The two case reports involved uncommon BBAs located at the lateral wall of the ICA close to the AChA and explained the rescue surgical techniques for arterial repair to preserve the AChA using parallel clip placement and a microsuture technique18,21,24,26,29).
BBAs arising distant to the AChA origin can be treated with more popular surgical techniques, including trapping the ICA with or without an extracranial-to-intracranial (EC-IC) bypass, encircling clip placement, and clip placement on wrapping1,2,4,5,11,12,13,15,16,20,22,23,27,30). In the case of clip placement on wrapping, a transparent silicone sheet, strip of polytetrafluoroethylene membrane, or microsurgical cotton pad can be used to wrap the affected ICA11,14,15). However, if the BBA is located close to the AChA, these surgical strategies are limited and pose a high risk of morbidity due to AChA insufficiency, postoperative rebleeding with recurrence, and a poor outcome.
In cases of a BBA at the level of the AChA, if the BBA is located at the superior or superomedial wall of the ICA, tapping the affected ICA or clip placement on wrapping material can be applied. When trapping the affected ICA with 2 aneurysm clips, oblique clipping of the distal side of the ICA can avoid occlusion of the AChA emitting from the lateral wall of the ICA28). Alternatively, the ICA at the level of the AChA can be wrapped by cutting a slit in one end of the wrapping material to accommodate the AChA that is opposite the BBA8). However, for the current case reports, these techniques would not have avoided AChA insufficiency.
Direct surgical repair of an arterial defect can be performed by either direct clipping or a microsuture technique. For superomedial, superior, and superolateral BBAs, a C-shaped or right-angled clip can be applied to the arterial defect parallel to the ICA in order to catch both edges of the arterial defect. For a superomedial BBA, which is the most common type, a pterional craniotomy is created toward the midline to introduce a clip toward the arterial lesion. Meanwhile, for a superolateral BBA, a normal pterional craniotomy is enough to introduce a clip to the lesion, although a left-side lesion requires the clip to be applied using the left hand. If an optimal clip application is not possible due to the location or size of the BBA, arterial repair using a microsuture technique is the next resort. A few stitches approximating the edges of the arterial defect create an affectedarterial segment tubular shape and allow more optimal clip application. If normal healthy walls beyond the fragile margin of the BBA can be approximated, microsutures without clip reinforcement can be enough to repair the BBA. However, an angiographic follow-up 1 month after the surgery is required due to the risk of recurrence.
The extent of the lesion including the BBA and surrounding fragile wall of the ICA can sometimes be much greater than expected based on angiographic evaluation, and such situations can lead to trapping the affected ICA as a final resort. Thus, in preoperative angiographic examinations, the effect of ICA occlusion should be evaluated, and donor vessels for an EC-IC bypass, such as a superficial temporal artery, radial artery, or saphenous vein, need to be prepared just in case. The current two cases showed good collateral circulation through the anterior and posterior communicating arteries, and did not require donor vessel preparation.
Ruptured BBAs close to the origin of the AChA are difficult to recognize angiographically and present a serious surgical challenge to preserve the patency of the AChA and prevent a recurrent hemorrhage. However, direct arterial repair using aneurysm clips and microsuture techniques can provide good surgical results.
References
1. Abe M, Tabuchi K, Yokoyama H, Uchino A. Blood blisterlike aneurysms of the internal carotid artery. J Neurosurg. 1998; 89:419–424. PMID: 9724116.

2. Başkaya MK, Ahmed AS, Ateş O, Niemann D. Surgical treatment of blood blister-like aneurysms of the supraclinoid internal carotid artery with extracranial-intracranial bypass and trapping. Neurosurg Focus. 2008; 24:E13. PMID: 18275289.

3. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF. Stent-assisted coiling in acutely ruptured intracranial aneurysms : a qualitative, systematic review of the literature. AJNR Am J Neuroradiol. 2011; 32:1232–1236. PMID: 21546464.

4. Charbel FT, Gonzales-Portillo G, Hoffman W, Cochran E. Distal internal carotid artery pseudoaneurysms : technique and pitfalls of surgical management : two technical case reports. Neurosurgery. 1999; 45:643–648. discussion 648-649. PMID: 10493387.
5. Cho TG, Hwang SN, Nam TK, Park SW. Salvage surgical treatment for failed endovascular procedure of a blood blister-like aneurysm. J Cerebrovasc Endovasc Neurosurg. 2012; 14:99–103. PMID: 23210036.

6. Dashti R, Laakso A, Niemelä M, Porras M, Hernesniemi J. Microscope-integrated near-infrared indocyanine green videoangiography during surgery of intracranial aneurysms : the Helsinki experience. Surg Neurol. 2009; 71:543–550. discussion 550. PMID: 19328531.

7. Fischer G, Stadie A, Oertel JM. Near-infrared indocyanine green videoangiography versus microvascular Doppler sonography in aneurysm surgery. Acta Neurochir (Wien). 2010; 152:1519–1525. PMID: 20623360.

8. Garrett M, Spetzler RF. Surgical treatment of blister-like aneurysms. World Neurosurg. 2012; 77:76–77. PMID: 22405389.

9. Irie T, Yoshitani K, Ohnishi Y, Shinzawa M, Miura N, Kusaka Y, et al. The efficacy of motor-evoked potentials on cerebral aneurysm surgery and new-onset postoperative motor deficits. J Neurosurg Anesthesiol. 2010; 22:247–251. PMID: 20548170.

10. Ishikawa T, Nakamura N, Houkin K, Nomura M. Pathological consideration of a "blister-like" aneurysm at the superior wall of the internal carotid artery : case report. Neurosurgery. 1997; 40:403–405. discussion 405-406. PMID: 9007879.

11. Joo SP, Kim TS, Moon KS, Kwak HJ, Lee JK, Kim JH, et al. Arterial suturing followed by clip reinforcement with circumferential wrapping for blister-like aneurysms of the internal carotid artery. Surg Neurol. 2006; 66:424–428. discussion 428-429. PMID: 17015131.

12. Kamijo K, Matsui T. Acute extracranial-intracranial bypass using a radial artery graft along with trapping of a ruptured blood blister-like aneurysm of the internal carotid artery. Clinical article. J Neurosurg. 2010; 113:781–785. PMID: 19929189.

13. Kazumata K, Nakayama N, Nakamura T, Kamiyama H, Terasaka S, Houkin K. Changing treatment strategy from clipping to radial artery graft bypass and parent artery sacrifice in patients with ruptured blister-like internal carotid artery aneurysms. Neurosurgery. 2014; 10(Suppl):66–72. discussion 73. PMID: 23842547.

14. Kim YB, Hong CK, Chung J, Joo JY, Huh SK. Long-term clinical and angiographic outcomes of wrap-clipping strategies for unclippable cerebral aneurysms. Yonsei Med J. 2014; 55:401–409. PMID: 24532510.

15. Kubo Y, Ogasawara K, Tomitsuka N, Otawara Y, Watanabe M, Ogawa A. Wrap-clipping with polytetrafluoroethylene for ruptured blisterlike aneurysms of the internal carotid artery. Technical note. J Neurosurg. 2006; 105:785–787. PMID: 17121147.

16. Kurokawa Y, Wanibuchi M, Ishiguro M, Inaba K. New method for obliterative treatment of an anterior wall aneurysm in the internal carotid artery : encircling silicone sheet clip procedure--technical case report. Neurosurgery. 2001; 49:469–472. PMID: 11504127.

17. Lim YC, Kim BM, Suh SH, Jeon P, Kim SH, Ihn YK, et al. Reconstructive treatment of ruptured blood blister-like aneurysms with stent and coil. Neurosurgery. 2013; 73:480–488. PMID: 23728453.

18. McLaughlin N, Laroche M, Bojanowski MW. Surgical management of blood blister-like aneurysms of the internal carotid artery. World Neurosurg. 2010; 74:483–493. PMID: 21492599.

19. Meling TR, Sorteberg A, Bakke SJ, Slettebø H, Hernesniemi J, Sorteberg W. Blood blister-like aneurysms of the internal carotid artery trunk causing subarachnoid hemorrhage : treatment and outcome. J Neurosurg. 2008; 108:662–671. PMID: 18377243.

20. Murai Y, Mizunari T, Umeoka K, Tateyama K, Kobayashi S, Teramoto A. Ischemic complications after radial artery grafting and aneurysmal trapping for ruptured internal carotid artery anterior wall aneurysm. World Neurosurg. 2012; 77:166–171. PMID: 22405395.

21. Nakagawa F, Kobayashi S, Takemae T, Sugita K. Aneurysms protruding from the dorsal wall of the internal carotid artery. J Neurosurg. 1986; 65:303–308. PMID: 3734880.

22. Ogawa A, Suzuki M, Ogasawara K. Aneurysms at nonbranching sites in the surpaclinoid portion of the internal carotid artery : internal carotid artery trunk aneurysms. Neurosurgery. 2000; 47:578–583. discussion 583-586. PMID: 10981744.

23. Ohkuma H, Nakano T, Manabe H, Suzuki S. Subarachnoid hemorrhage caused by a dissecting aneurysm of the internal carotid artery. J Neurosurg. 2002; 97:576–583. PMID: 12296641.

24. Park J. Maintenance of cerebral blood flow during microsuture repair of the superior wall of the intracranial internal carotid artery. World Neurosurg. 2013; 80:436.e1–436.e5. PMID: 23563099.

25. Park JH, Park IS, Han DH, Kim SH, Oh CW, Kim JE, et al. Endovascular treatment of blood blister-like aneurysms of the internal carotid artery. J Neurosurg. 2007; 106:812–819. PMID: 17542524.

26. Regelsberger J, Matschke J, Grzyska U, Ries T, Fiehler J, Köppen J, et al. Blister-like aneurysms--a diagnostic and therapeutic challenge. Neurosurg Rev. 2011; 34:409–416. PMID: 21584689.

27. Sekula RF Jr, Cohen DB, Quigley MR, Jannetta PJ. Primary treatment of a blister-like aneurysm with an encircling clip graft : technical case report. Neurosurgery. 2006; 59(1 Suppl 1):ONSE168. discussion ONSE168. PMID: 16894653.
28. Shimizu H, Matsumoto Y, Tominaga T. Non-saccular aneurysms of the supraclinoid internal carotid artery trunk causing subarachnoid hemorrhage : acute surgical treatments and review of literatures. Neurosurg Rev. 2010; 33:205–216. PMID: 20521339.

29. Sim SY, Shin YS, Cho KG, Kim SY, Kim SH, Ahn YH, et al. Blood blister-like aneurysms at nonbranching sites of the internal carotid artery. J Neurosurg. 2006; 105:400–405. PMID: 16961134.

30. Yanaka K, Meguro K, Nose T. Repair of a tear at the base of a blister-like aneurysm with suturing and an encircling clip : technical note. Neurosurgery. 2002; 50:218–221. PMID: 11844255.

Fig. 1
Case 1. A : Left carotid angiogram showing an ill-defined, slight bulging (arrow) in the lateral wall of the ICA at the level of the AChA. B : In-traoperative photograph showing a right-angled aneurysm clip applied parallel to the ICA to catch the edges of the arterial defect, producing mild stenosis of the ICA. C : 1-year follow-up DSA demonstrating preservation of the AChA (arrow) without recurrence of the BBA and the stenotic ICA induced by clip application. ICA : internal carotid artery, DSA : digital subtraction angiography, AChA : anterior choroidal artery, BBA : blood blister-like aneurysm.
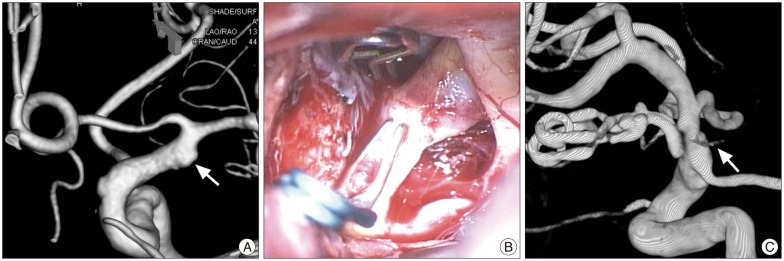
Fig. 2
Case 2. A : A 3D reconstruction of DSA images revealing the BBA (arrow) close to the origin of the AChA (arrowheads) without relation to the AChA. B : Intraoperative photograph showing the lesioned distal ICA harboring a rupture point covered by a blood clot in the lateral wall and friable anterior and medial walls. C : Illustration demonstrating a large arterial defect and adjacent AChA in the distal ICA. D : Illustration showing severe stenosis of the distal ICA after microsuturing the arterial defect. E : Intraoperative photograph showing the AChA emitting from the stenotic distal ICA after reinforcement using an aneurysm clip. F : 6-month follow-up DSA showing the severely stenotic ICA and preservation of the patency of the AChA (arrowheads) and PCoA (arrows) without recurrence. DSA : digital subtraction angiography, BBA : blood blister-like aneurysm, AChA : anterior choroidal artery, PCoA : posterior communicating artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download