INTRODUCTION
Postoperative spondylodiscitis is among the lethal complications of spinal surgery. This condition results mostly from inoculation of microbes through the incision line during posterior approach to the spine. In many cases, this inoculation primarily infects the intervertebral disc and subsequently spreads to the adjacent vertebral structures
4). Most patients with early postoperative spondylodiscitis can be treated with conservative methods, such as intravenous antibiotics, immobilization, and bracing. However, more aggressive approach or even surgical management is required in advanced or complicated cases
11). Anterior lumbar interbody fusion (ALIF) may be an effective alternative method for the management of postoperative spondylodiscitis
11). To date, however, there is no general consensus on the surgical approach in postoperative spondylodiscitis management. Since the clinical outcomes and complications after ALIF for postoperative spondylodiscitis are also poorly understood, we retrospectively analyzed the outcomes and complications of patients who received ALIF for the treatment of postoperative spondylodiscitis in this study.
MATERIALS AND METHODS
Study population and peri-operative management
From January, 1994 to August, 2013, 13251 patients received spinal surgeries at our institute. Among them, 82 (0.62%) suffered postoperative spondylodiscitis, and ALIF was done in 13 patients. Therefore, the study population consisted of 13 consecutive patients with postoperative spondylodiscitis who were treated with ALIF. Postoperative spondylodiscitis was suspected when the patients had symptoms and signs suggestive of local infection, including fever, progression of local pain, and redness or edema at the operation site. Diagnostic measures are composed of laboratory findings, X-ray, and contrast-enhanced MRI. To treat postoperative spondylodiscitis, we first tried non-operative methods such as administrating antibiotics for 6-8 weeks. However, whenever the infection was so progressive that it was insufficient to treat by antibiotics alone, such as epidural abscesses or neural compression, we operated as soon as possible.
The immediate postoperative assessment consisted of physical examination and radiologic evaluation. The Oswestry Disability Index (ODI) was used for assessment of quality of life, and the modified Visual Analogue Scale (VAS) for assessment of pain. These parameters were measured before and 6 months after the ALIF. Serial spine X-rays that included dynamic flexion-extension views were used to assess radiologic outcomes. The successful fusion was defined as : 1) absence of halo around the screws; 2) presence of bilateral continuous trabecular bone bridge between the fused segments on the anteroposterior plain film; and 3) lack of motion on the flexion-extension film. The successful fusion was confirmed by the attending surgeon using these parameters
7). At our institute, we usually follow up patients at postoperative 1, 3, and 6 months and then annually thereafter. In patients with complications, additional outpatient visits or hospital admissions are prescribed. The follow-up data were collected by medical record review and direct telephone interview using a standardized form including information about demographics, medical history, clinical presentation, results of follow-up images, and adverse clinical events. In the cases with missing values in the variables before 2000, especially in the ODI score, we approximated the values by extensive review of the previous medical records regarding patient's subjective complaint of symptoms.
Surgical techniques
Patients were positioned supine on the operating table with their arms abducted on arm boards. After a paramedian "minilaparotomy" was performed, location of the aortic bifurcation, the vena cava, and iliac arteries and veins were identified after anterior retroperitoneal approach. Cauterization was avoided near the presacral sympathetic plexus. The great vessels and their tributaries were mobilized to provide exposure of the disc space. For L5-S1 level, the midline sacral vessels were ligated, and the iliac arteries and veins were mobilized. For L3-4, L4-5 level, the iliolumbar and segmental vessels were ligated, and the aorta and vena cava were mobilized to expose the entire ventral surface of the disc space. After the infected and adhered anterior surface of the spine was exposed, a rectangular incision was made anteriorly in the annulus fibrosus, followed by a discectomy at that level. Once the ventral dura was exposed, infected tissue was debrided completely and irrigated sufficiently. After compete removal of the infected tissue, interbody fusion was performed with autologous tricortical iliac bone block or interbody fusion cages packed with autologous cancellous bone. The operative wound was closed layer by layer in a routine fashion.
Statistical analysis
All analyses were performed with Statistical Package for the Social Sciences (SPSS) version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean±SD, and categorical variables are presented as frequencies. Paired t-tests and chi-square tests were used to compare pre- and post-operative values. All p-values are two-tailed, and p<0.05 was considered statistically significant.
RESULTS
Baseline characteristics and surgical indications
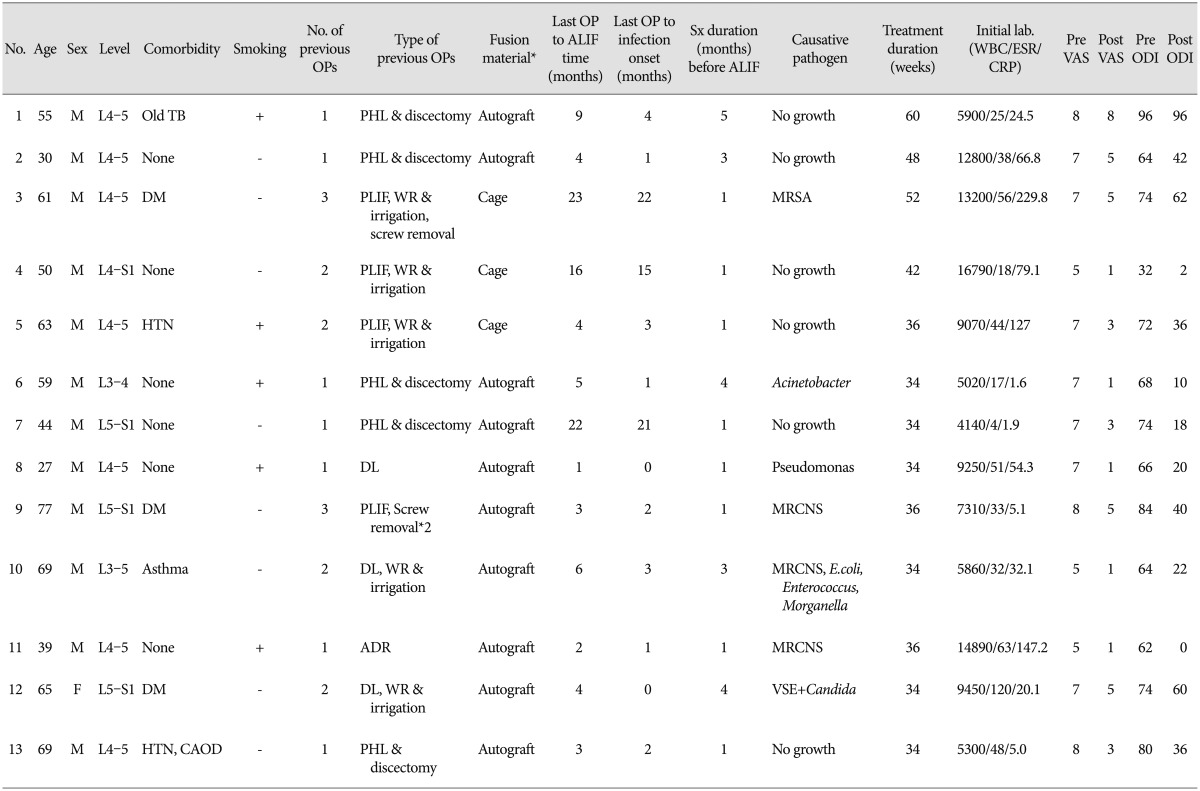
The baseline characteristics, surgical indications, and clinical outcomes are summarized in
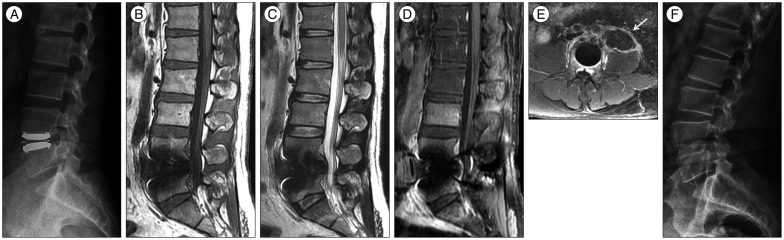
Table 1, and a representative case is described in
Fig. 1. Most patients were men (92.3%, 12/13), and the mean age was 54.5 years old (27-77 years). Seven out of 13 patients underwent spine surgery once, four underwent spine surgery twice, and two underwent spine surgery more than three times before ALIF at our institute. The previous surgical procedures were partial hemilaminectomy and discectomy in five patients, decompressive laminectomy in three patients, posterior lumbar interbody fusion in four patients, and artificial disc replacement in one patient.
Among the 13 total patients, 10 had revision surgery within 1 year after the primary surgery; three had revision surgery 1-3 years after the primary surgery. The mean interval from the primary surgery to ALIF was 7.8 months (1-23 months), and the average duration of symptoms before ALIF was 2.1 months (1-5 months). The mean interval from the primary surgery to postoperative spondylodiscitis was 5.8 months (1-22 months). After ALIF, the patients were followed up for an average of 112 months (8-234 months).
Surgical levels and materials
The 13 patients underwent surgery on a total of 15 segments. Eleven patients underwent single-level fusion, and two patients underwent two-level fusions. The levels fused included L5-S1 (4 cases), L4-5 (9 cases), and L3-4 (2 cases). Decisions regarding the surgical levels fused were made at the attending surgeon's discretion. Autologous tricortical bone block was used in cases with endplate destruction from the discitis, whereas interbody fusion cages were used in cases without endplate destruction after the antimicrobial therapy. The autologous iliac bone block was used as the interbody fusion material in 10 out of 13 cases. Titanium threaded cages were used in the other three cases.
Causative pathogens and infection control
Bacterial pathogens were identified in seven out of 13 patients (53.8%). One patient was co-infected with fungus. The most common pathogens were staphylococcus species, including one methicillin-resistant staphylococcus aureus and three methicillin-resistant coagulase-negative staphylococci. The next common pathogen was Gram-negative rods (2 cases). The culture results were negative in six patients. In one patient (No. 12), vancomycin-sensitive enterococcus was initially identified, but candida albicans was also isolated thereafter. This patient was treated with combination of vancomycin and amphotericin B.
In the laboratory findings, the initial average erythrocyte sedimentation rate (ESR) level was 42.2±28.8 mm/h (0-15 mm/h), C-reactive protein (CRP) level was 61.1±69.4 mg/L (0-5.3 mg/L), and the leukocyte count was 9152±4111/mm3. Initial intravenous (IV) antibiotic therapy was started immediately after the clinical diagnosis was made. The average duration of intravenous antibiotic therapy in the study population was 8 weeks (4-15 weeks) after the ALIF. After 6 months, inflammatory markers (WBC, ESR, and CRP) were within the normal range for all patients.
Pain control and successful bony fusion
Mean VAS for back and leg pain before ALIF was 6.8±1.1, which improved to 3.2±2.2 after ALIF (p<0.001). The mean ODI score before was 70.0±14.8, which improved to 34.2±27.0 at 6 months after ALIF. Bony fusion at 6 months after the surgery occurred in 11 out of 13 patients. The remaining two patients did not meet the definition of bony fusion which used for the assessment in this study; however, all patients had no related symptoms and could be managed conservatively.
Postoperative complications
There were no specific post-ALIF complications during the follow-up in the study population.
DISCUSSION
Early treatment of postoperative spondylodiscitis usually consists of bed rest, immobilization, and broad-spectrum antibiotics. For advanced disease, a posterior approach such as laminectomy has been considered a standard procedure
12). However, this procedure has some drawbacks, including failure to manage the infection components anterior to the vertebrae and postoperative instability
12).
This retrospective analysis revealed that ALIF led to successful management of postoperative spondylodiscitis in terms of infection control and symptom improvement. In addition, ALIF provided optimal symptomatic improvement and stabilization of the vertebrae in most cases
5,
11). ALIF has many benefits in postoperative spondylodiscitis management of the previous infected vertebral structures compared to a posterior approach. First, it causes minimal or no epidural bleeding and no dural tears
15). Second, it provides surgeons with wide exposure of the entire disc space through unscarred passage. Third, it avoids dissection of perineural scar tissue, retraction of the scarred nerve root and dura, and removal of the facets usually associated with repeated discectomy
3). Fourth, it allows more efficient restoration of intervertebral disc height and indirect decompression of the intervertebral foramen in case of foraminal stenosis
3). Accessing the entire disc space allows for greater distraction, the placement of bigger interbody devices, and greater possibilities of arthrodesis
14). In addition, ALIF preserves all remaining posterior paraspinal tissues (lamina, facets, ligaments, and muscle), thereby preserving spinal stability, which may help reduce the degeneration of adjacent motion segments
3). From a biomechanical standpoint, the interbody fusion device can be placed at the weight-bearing center of the spine across the degenerated disc space, where 80% of axial load occurs
13). Furthermore, disc height and sagittal balance can be more effectively restored in ALIF than in posterior lumbar surgery in terms of creating preferable fusion conditions by placing the interbody fusion device as extensively as possible under compression with a voluminous blood supply from the adjacent vertebral endplates
1,
3). In terms of onset of postoperative spondylodiscitis, it could be classified as early (<20 weeks) and late (>20 weeks) infections
2). In our series, although all patients were operated at the mean of 7.7 months after initial surgery, some patients received delayed operation due to late onset infection and they also successfully treated using ALIF.
The goals of treatment for postoperative spondylodiscitis are as follow : 1) eradicate the infected tissue, 2) prevent neurological damage, 3) restore spinal balance, and 4) relieve pain
6,
8,
9). Patients with mild infection can be managed with 6-8 weeks of intravenous antibiotics
6). Moreover, if possible, surgery can be delayed for 2 weeks to decrease inflammation, which allows for better demarcation of tissue planes for surgical dissection and decreases the risks from anesthesia in acutely ill patients
12). Regarding the timing of the surgery, there are several critical indications of emergent surgery, including progressive neurologic deterioration, epidural abscess, and symptoms of spinal cord compression
10). As the patient's prognosis cannot be improved after 48 hours of established paralysis, prompt surgical intervention is warranted in these "emergent" cases
10).
The primary limitation of the current study was its retrospective design. For this reason, indications of surgery, antibiotic treatment, and general care of patients varied from surgeon to surgeon, and the independent impact of ALIF on the management of postoperative spondylodiscitis could not be verified. In addition, this study focused only on a descriptive analysis of ALIF without a control group; thus, we cannot firmly state that ALIF is better or even equivalent to traditional posterior approaches. Although the recruiting period spanned two decades, only 13 patients could be enrolled, which limits the generalization and the prospectiveness of this study.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download