Abstract
Objective
The technique of short segment pedicle screw fixation (SSPSF) has been widely used for stabilization in thoracolumbar burst fractures (TLBFs), but some studies reported high rate of kyphosis recurrence or hardware failure. This study was to evaluate the results of SSPSF including fractured level and to find the risk factors concerned with the kyphosis recurrence in TLBFs.
Methods
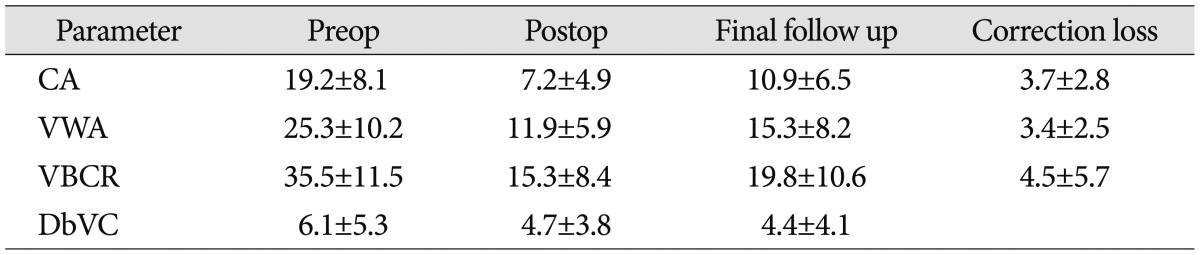
This study included 42 patients, including 25 males and 17 females, who underwent SSPSF for stabilization of TLBFs between January 2003 and December 2010. For radiologic assessments, Cobb angle (CA), vertebral wedge angle (VWA), vertebral body compression ratio (VBCR), and difference between VWA and Cobb angle (DbVC) were measured. The relationships between kyphosis recurrence and radiologic parameters or demographic features were investigated. Frankel classification and low back outcome score (LBOS) were used for assessment of clinical outcomes.
Results
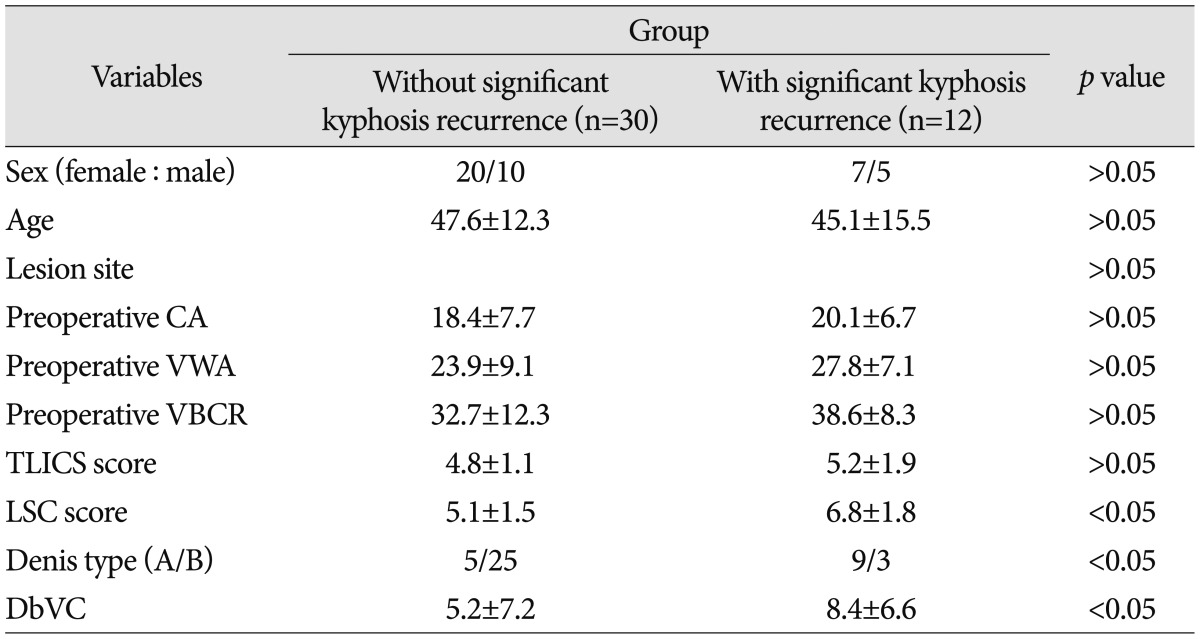
The mean follow-up period was 38.6 months. CA, VWA, and VBCR were improved after SSPSF, and these parameters were well maintained at the final follow-up with minimal degree of correction loss. Kyphosis recurrence showed a significant increase in patients with Denis burst type A, load-sharing classification (LSC) score >6 or DbVC >6 (p<0.05). There were no patients who worsened to clinical outcome, and there was no significant correlation between kyphosis recurrence and clinical outcome in this series.
Thoracolumbar vertebral body fractures are common spinal injuries, and fractures of burst type account for 21 to 58% of all thoracolumbar spinal fractures9,10). Burst fractures occur predominantly in young patients, and are associated with kyphotic deformity and neurological injury caused by retropulsion of fractured fragments. Therefore, inadequate treatment for burst fractures can have a significant impact on patient's physical and occupational activities21).
Treatment goals for thoracolumbar burst fractures (TLBFs) include restoration of spinal stability and alignment, correction of kyphotic deformity and decompression of the spinal canal. For achievement of these desired results, most authors believe that burst fractures require surgical intervention; however, controversy with regard to treatment continues15,16,17). Various surgical techniques, including posterior short segment or long segment pedicle screw fixation, direct anterior decompression through corpectomy, and combined methods through anterior and posterior spinal approaches, have since arisen for treatment of TLBFs2,16,23,26,28). However, the decision of surgical methods still remains controversy6,16,26).
Short-segment pedicle screw fixation (SSPSF) via a posterior spinal approach is the most common and simple treatment option among surgical methods for TLBFs2,9,23,27). However, many reports have shown that SSPSF alone led to a high incidence of implant failure and kyphosis recurrence, and it accounts for approximately 9% to 54%1,22,30). In order to reduce previously mentioned complications after SSPSF, the technique of SSPSF including instrumentation for fractured vertebra was introduced19).
The purpose of the current study was to investigate the efficacy and results of SSPSF including fractured level and to determine preoperative factors contributing to kyphosis recurrence in TLBFs.
In this study we enrolled 42 patients with TLBFs who were treated by SSPSF including fractured level between January 2003 and December 2009 in our department. The criteria of Denis was used for classification of thoracolumbar body fractures10). Indications of SSPSF included regional kyphosis >30 degrees, vertebral body collapse >40%, spinal canal compromise with neurologic deficits, or three column injury. Only isolated fractures were included, and patients with multiple spinal fractures, previous spinal surgery, or severe osteopenia (bone mineral density T-score in dual-energy X-ray absorptiometry <-2.5) were excluded from this study.
The conventional posterior approach was performed with the patient in a prone position. After clean exposure of bilateral posterior elements, pedicle screws were inserted into the vertebral body one level above and below the fractured vertebra. We also inserted pedicle screws into the fractured vertebra. If necessary, partial laminectomies were performed for decompression of the encroached spinal canal caused by fractured bony fragments. Following insertion of the pedicle screws, surfaces of posterior elements, including lamina and wall of the facet, were decorticated by use of a high speed drill. Bilateral posterior or posterolateral fusion was then added. All patients were braced postoperatively by thoracolumbosacral orthesis (TLSO) for 3 months, and early ambulation was encouraged.
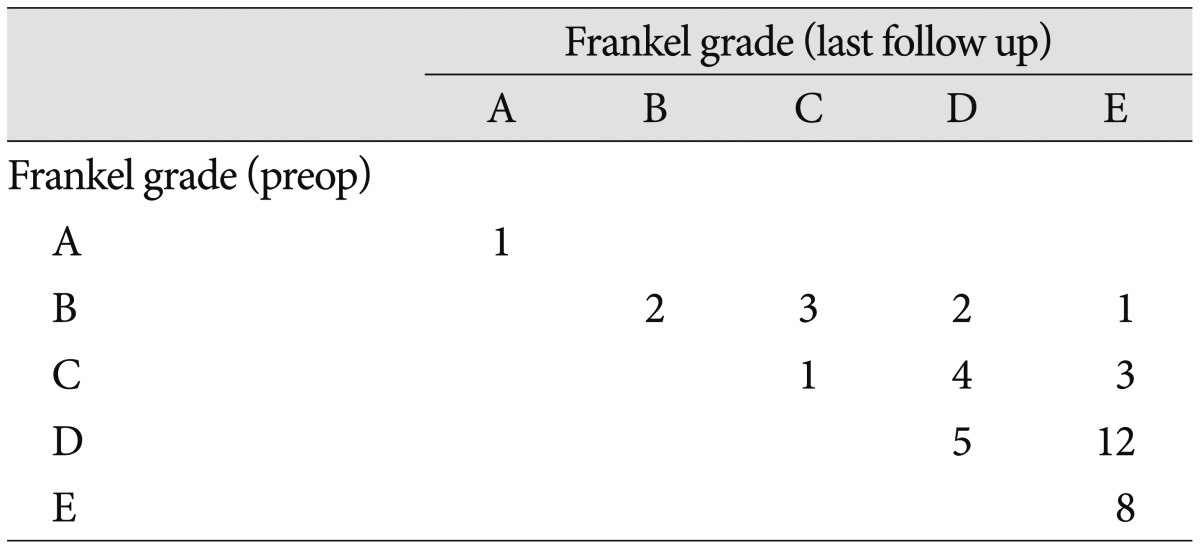
Simple plain radiographs were obtained prior to surgery, immediately after surgery, and at final follow up. Cobb angle (CA), vertebral body compression ratio (VBCR), vertebral wedge angle (VWA), and difference between VWA and CA (DbVC) were measured on neutral lateral radiographs (Fig. 1). We used the CA as the parameter for local kyphosis angle. Each injury was clarified by the classification of Denis burst fracture10).
The Thoracolumbar Injury Classification and Severity Score (TLICS), introduced by the Spine Trauma Study Group in 2005, was intended to provide a clear, reliable system for classification of thoracolumbar injury29). The system assigns numerical values to each injury based on the categories of morphology of injury, integrity of the posterior ligamentous complex, and neurological involvement. The load-sharing classification (LCS) was designed for quantification of comminution of the injured vertebral body20). We calculated the preoperative scores of TLICS and LSC by review of patient's charts, operative notes, radiographs, CT scans, and magnetic resonance imaging (MRI) images.
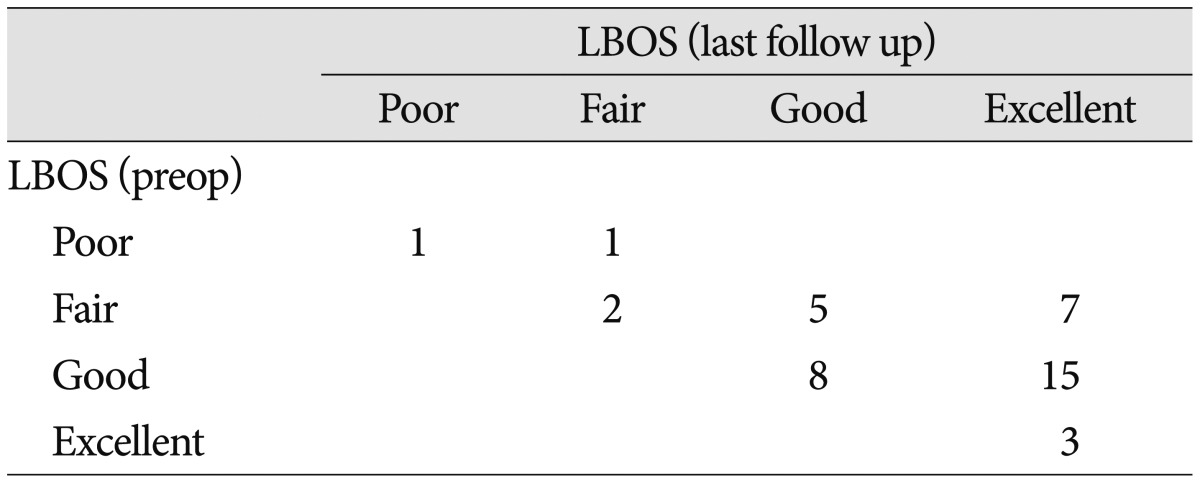
Neurologic assessment was performed using the grading scale of Frankel et al.12). Pain and work status were determined using the low back outcome score (LBOS) devised by Greenough and Fraser13). The grading system used was as follows : "excellent" (65-75), "good" (50-64), "fair" (30-49), and "poor" (0-30).
In this study, significant kyphosis recurrence was defined 3.7 degree, which was the mean value of kyphosis recurrence of this study. For determination of preoperative contributing factors associated with kyphosis recurrence, patients were divided into two groups, one with and one without significant kyphosis recurrence. The relationships between kyphosis recurrence and CA, VBCR, VWA, DbVC, the type of burst fracture, TLICS, and LSC score, were assessed. Clinical outcomes, including Frankel classification and LBOS, were also analyzed.
The SPSS program for Windows V15.0 (SPSS, Chicago, IL, USA) was used for analysis of data; categorical variables were compared using Pearson's chi-square tests or Fisher exact tests. Continuous variables were reported as mean±standard deviations and compared using independent Student t-tests or Mann-Whitney U test. For all analyses, a p-value of <0.05 was considered statistically significant.
The average age of the patients was 46.7 years (range, 20-69 years), and there were 25 men and 17 women. At review all patients had a minimum follow-up of 1 year, with a mean of 38.6 months (range, 24-64 months). The fractured levels were T11 in 4 patients; T12 in 13, L1 in 19, and L2 in 6. A fall from height was the most common cause of injury, followed by traffic accidents.
CA, which generally reflects changes in the segmental curve, was measured between the inferior endplate of the upper and the superior endplate of the lower adjacent vertebrae. The average preoperative CA was 19.2±8.1, which decreased significantly decreased to 7.2±4.9 after surgery (p<0.05). However, there was no statistically significant difference of preoperative CA between two groups.
The VBCR is the percentage of the anterior vertebral body height of the fractured vertebra with respect to the average anterior height of two adjacent vertebrae. The VWA was measured between the superior endplate and the inferior endplate of the fractured vertebra body. They generally reflect the anatomical shape of the fractured vertebral body. The average VBCR and VWA were 35.5±11.5% and 25.3±11.5, which improved significantly to 15.3±8.4% and 11.9±5.9 after surgery (p<0.05). However, in the VBCR (p>0.05) and the VWA (p>0.05), there were no statistically significances between two parameters and kyphosis recurrence.
In cases with large preoperative DbVC, the difference between anterior and posterior disc height had been observed large compared to those with small preoperative DbVC. We thought that the value of preoperative DbVC may reflect the injured conditions of the above and below intervertebral disc spaces of the fractured vertebra after trauma (Fig. 2). In the patients group with significant kyphosis recurrence, the preoperative DbVC was significantly large compared to opposite group (p<0.05) (Table 1, 2).
According to the classification of Denis burst fracture, Type A is defined as a vertebral body fracture involving both end plates and Type B is defined as a fracture involving the superior end plate. There were 19 Type A and 23 Type B. We found that significant kyphosis recurrence was related with the Type A Denis burst fracture after SSPSF including fractured level (p<0.05) (Table 2).
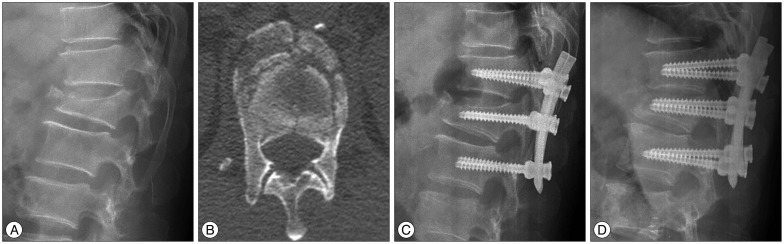
LSC scores were 3 points in 3 patients; 4 points in 9, 5 points in 11, 6 points in 8, 7 points in 9, 8 points in 2. TLICS scores were 2 points in 1 patient; 4 points in 10, 5 points in 13, 6 points in 8, 7 points in 6, 8 points in 4. Statistically significant difference of LSC score was found between two groups (p<0.001) (Fig. 3). However, no statistically significant difference of TLICS scores was observed between two groups (p>0.05) (Table 2).
No statistically significant differences of age, sex, and lesion site were observed between two groups (p>0.05) (Table 2).
The thoracolumbar junction (T11-L2) is the transitional zone between the stiff thoracic and the mobile lumbar spine; therefore, burst fractures in this region are usually very unstable and aggravation of kyphotic deformity after conservative managements is a frequently observed11). Selection of the surgical approach and method, such as corpectomy and reconstruction via an anterior approach, posterior instrumentation, or combined with an anterior and posterior approach, remains controversial1,6,16,26).
In TLBFs, introduction of transpedicular screw insertion by Roy-Camille made possible the frequently used posterior approaches25). Gurr and McAfee.14) demonstrated that long segment pedicle screw instrumentation, which included two levels above and below the fractured vertebra, offered adequate stiffness to stabilize an unstable thoracic or lumbar burst fractures. Alvine et al.3) suggested that use of long segment pedicle screw fixation to lengthen the level arm of the construct might not only have enhanced stiffness but also permitted effective correction of kyphosis. However, the technique requires extensive paraspinal muscle dissection, a large amount of intraoperative blood loss, many spinal motion segments for fixation, and longer operation time.
With development of instrumentation for a pedicle screw system, SSPSF has frequently been used as the procedure of choice for treatment of TLBFs, because it has several advantages, including incorporation of fewer motion segments in the fixation, shorter operative time and less blood loss, compared with long segment pedicle fixation. Initially, SSPSF involves screw insertion only at the levels adjacent to the fractured vertebra; however, results of this traditional SSPSF are not always as satisfactory as predicted1,18,20). To reduce the postoperative failure of SSPSF, additional insertion of pedicle screws at the level of the fracture has been adopted. As the additional screw provides a protective effect on the fractured vertebral body by indirectly supporting the anterior column and improving biomechanical stability, it is expected that postoperative surgical failures, such as screw loosening, breakage, and kyphosis recurrence, will be decreased19). In our series, there was no other instrumentation failure during the follow-up period after SSPSF with additional screws to the fractured vertebra.
Clinically, an average of 15 degrees of regional kyphosis correction could be obtained using SSPSF19). In traditional, non-segmental SSPSF, which was SSPSF without fractured level screw fixation, Cho et al.7) reported 6 degrees of initial postoperative kyphosis correction, and Carl et al.4) achieved 7 degrees of initial kyphosis correction. In the above two groups, much of the immediately postoperative kyphosis correction was lost at final follow-up radiographs. Our surgical results showed an initial correction of 12.0±5.3 degrees of regional kyphosis after surgery. The last follow-up films revealed 3.7±2.8 degrees loss of kyphosis correction, resulting in a final kyphosis correction of 8.3±4.2 degrees. Although kyphosis recurrence of 3.7±2.8 degrees was observed, this result suggested that SSPSF including fractured level was effective and likely better than traditional, non-segmental SSPSF.
Among the classification of TLBFs based on a three-column concept, the classification of Denis was widely used, because it could be easily applied by radiologic exams. In our study, only patients with Denis type A or B fractures were included. The group with Denis type A was significantly associated with kyphosis recurrence after SSPSF, compared with the group with Denis type B on the last follow-up radiographs. Denis type A involves a fracture of the superior and inferior end plates and Denis type B, the most common type of TLBF, involves only failure of the superior vertebral end plate. Therefore, it is reasonable that Denis type A is more unstable than Denis type B and that more significant development of kyphosis recurrence can occur in patients with Denis type A burst fracture, compared to patients with Denis type B.
The TLICS and the LSC scoring systems have been widely used for decisions regarding treatment of TLBFs. The TLICS scoring system defines injuries according to injury morphology, posterior ligamentous complex (PLC) integrity, and neurological status of the patient. It serves in surgical or medical decision-making by providing both diagnostic and prognostic information with a weighted injury severity score. Patel et al.24) suggested that stable TLBFs, which TLICS score is less than 4, may be treated nonoperatively with brace immobilization and that unstable injury patterns (TLICS score >4) may be treated operatively. The LSC scoring system was developed for quantification of the most injured vertebral body. Dai et al.8) advocated that SSPSF without posterolateral fusion can provide sufficient spinal stability in TLBFs with a LSC score of <6. Our result showed that the TLICS score was not associated with kyphosis recurrence. By contrast, a LSC score in group with significant kyphosis recurrence was statistically larger than that of opposite group. In this study, preoperative LSC score in group with significant kyphosis recurrence was 6.8±1.8. In general, the TLICS scoring system reflects the overall state of fractured vertebra, including adjacent ligamentous complex and neural structure compression, and the LSC scoring system reflects only the degrees of comminution of vertebral body in detail. In the present study, kyphosis recurrence after SSPSF was associated with the LSC system, and, thus, the severity of the vertebral body comminution may be an important factor in recurrence of postoperative kyphosis. This result suggests that the LSC may be a more effective classification system for use in selection of a surgical method in treatment of TLBFs.
In our results, VWA and VBCR were not associated with kyphosis recurrence. This fact indicates that VWA and VBCR may not reflect the overall state of fractured vertebra, including the degree of comminution, adjacent intervertebral discs, and ligamentous injury, although these radiologic parameters reflect the anatomical shape of the fractured vertebral body. CA was also not associated with kyphosis recurrence. Although it indicates changes in the segmental curve of the fractured segment, CA may also not reflect the overall state of a fractured segment. As a result, we thought that these simple radiologic parameters, including vertebral wedge angle, vertebral body compression ratio, and CA, may not be the predictive factor associated with correction loss after SSPSF in TLBFs.
Upper and lower intervertebral discs adjacent to fractured vertebra can also be injured in TLBFs. Wang et al.30) advocated that intervertebral disc space collapse resulted in a progressive postoperative kyphotic deformity. In his study, the authors believed that progressive disc space narrowing might be a result of a simple adaptation to morphologic change in the osseous endplate or creeping of the disc back into the central depression of the endplate. However, central creeping was not routinely observed in the cases with severe disc space changes related to postoperative kyphosis recurrence. In this study, we defined the DbVC as the difference between VWA and CA, and we supposed that the DbVC may reflect the injured state of the upper and lower intervertebral discs adjacent to fractured vertebra. Our results showed that DbVC was 8.4±6.6 in group with significant kyphosis recurrence, and it was significantly large compared to the opposite group. In these cases, the anterior disc height was observed to be larger than the posterior disc height, compared with other level discs. In TLBFs, the main mechanisms are compression and flexion force; therefore, the anterior portion of the vertebral body is the most fragile structure. This fact indicates that the anterior portion of the intervertebral discs adjacent to the fractured vertebra may be injured by flexion and compression forces with severe anterior body collapse. Disruption of adjacent intervertebral discs is considered one of the major reasons for postoperative morphologic change, in which the anterior disc height was gradually reduced, and may eventually lead to kyphosis recurrence without additional bony morphological changes of the fractured vertebra.
Excessive preoperative or intraoperative kyphosis correction may be associated with significant correction loss5,7). In our study, we did not demonstrate a relationship between excessive intraoperative kyphosis correction and kyphosis recurrence. We thought that regional kyphosis correction can be performed without correction of VWA in cases with a large DbVC. The tension powers of adjacent anterior intervertebral discs can be decreased after injury, which may lead to correction of regional kyphosis without reduction of the fractured vertebral body. As a result, we suggested that the DbVC can be an important factor to in prediction of the kyphosis recurrence after surgery for treatment of TLBFs. In the future, biomechanical studies, and radiologic proof including magnetic resonance image findings for injured adjacent intervertebral discs will be required to confirm the usefulness of the DbVC in TLBFs.
SSPSF including additional fixation to the fractured level is effective clinically and radiologically for treatment of TLBFs. However, significant positive correlations were found between kyphosis recurrence and the Denis burst type A fracture, LSC score >6, or DbVC >8. Although, clinical outcomes were acceptable in the previously suggested groups, long-term follow up of patients is necessary in order to more clearly evaluate all of these results. Finally, the DbVC, which can easily be measured in simple radiographs, will play an important role in prediction of kyphosis recurrence after SSPSF for treatment of TLBFs.
Acknowledgements
This work was supported by a grant (CRI14021-1) from the Chonnam National University Hospital Research Institute of Clinical Medicine.
References
1. Alanay A, Acaroglu E, Yazici M, Oznur A, Surat A. Short-segment pedicle instrumentation of thoracolumbar burst fractures : does transpedicular intracorporeal grafting prevent early failure? Spine (Phila Pa 1976). 2001; 26:213–217. PMID: 11154543.
2. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007; 16:1145–1155. PMID: 17252216.

3. Alvine GF, Swain JM, Asher MA, Burton DC. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis : case series and literature review. J Spinal Disord Tech. 2004; 17:251–264. PMID: 15280752.

4. Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 1992; 17(8 Suppl):S317–S324. PMID: 1523519.

5. Celebi L, Doğan O, Muratli HH, Yağmurlu MF, Biçimoğlu A. [The effectiveness of short-segment posterior instrumentation of thoracolumbar burst fractures]. Acta Orthop Traumatol Turc. 2007; 41:183–189. PMID: 17876116.
6. Chen HH, Wang WK, Li KC, Chen TH. Biomechanical effects of the body augmenter for reconstruction of the vertebral body. Spine (Phila Pa 1976). 2004; 29:E382–E387. PMID: 15371717.

7. Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery. 2003; 53:1354–1360. discussion 1360-1361. PMID: 14633301.

8. Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am. 2009; 91:1033–1041. PMID: 19411450.

9. Dai LY, Yao WF, Cui YM, Zhou Q. Thoracolumbar fractures in patients with multiple injuries : diagnosis and treatment-a review of 147 cases. J Trauma. 2004; 56:348–355. PMID: 14960979.

10. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8:817–831. PMID: 6670016.

11. Denis F, Armstrong GW, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit. A comparison between operative and nonoperative treatment. Clin Orthop Relat Res. 1984; (189):142–149. PMID: 6478691.

12. Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969; 7:179–192. PMID: 5360915.

13. Greenough CG, Fraser RD. Assessment of outcome in patients with low-back pain. Spine (Phila Pa 1976). 1992; 17:36–41. PMID: 1531553.

14. Gurr KR, McAfee PC. Cotrel-Dubousset instrumentation in adults. A preliminary report. Spine (Phila Pa 1976). 1988; 13:510–520. PMID: 3187697.
15. Jacobs RR, Asher MA, Snider RK. Thoracolumbar spinal injuries. A comparative study of recumbent and operative treatment in 100 patients. Spine (Phila Pa 1976). 1980; 5:463–477. PMID: 7455777.
16. Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997; 79:69–83. PMID: 9010188.

17. Katonis PG, Kontakis GM, Loupasis GA, Aligizakis AC, Christoforakis JI, Velivassakis EG. Treatment of unstable thoracolumbar and lumbar spine injuries using Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976). 1999; 24:2352–2357. PMID: 10586460.

18. Leferink VJ, Zimmerman KW, Veldhuis EF, ten Vergert EM, ten Duis HJ. Thoracolumbar spinal fractures : radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J. 2001; 10:517–523. PMID: 11806393.

19. Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976). 2007; 32:1503–1507. PMID: 17572619.

20. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994; 19:1741–1744. PMID: 7973969.

21. McLain RF. Functional outcomes after surgery for spinal fractures : return to work and activity. Spine (Phila Pa 1976). 2004; 29:470–477. discussion Z6. PMID: 15094545.

22. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am. 1993; 75:162–167. PMID: 8423176.

23. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures : a consecutive 41/2-year series. Spine (Phila Pa 1976). 2000; 25:1157–1170. PMID: 10788862.

24. Patel AA, Dailey A, Brodke DS, Daubs M, Harrop J, Whang PG, et al. Thoracolumbar spine trauma classification : the Thoracolumbar Injury Classification and Severity Score system and case examples. J Neurosurg Spine. 2009; 10:201–206. PMID: 19320578.

25. Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986; 17:147–159. PMID: 3945476.

26. Sasso RC, Best NM, Reilly TM, McGuire RA Jr. Anterior-only stabilization of three-column thoracolumbar injuries. J Spinal Disord Tech. 2005; (18 Suppl):S7–S14. PMID: 15699808.

27. Shin TS, Kim HW, Park KS, Kim JM, Jung CK. Short-segment pedicle instrumentation of thoracolumbar burst-compression fractures; short term follow-up results. J Korean Neurosurg Soc. 2007; 42:265–270. PMID: 19096554.

28. Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture : short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech. 2005; 18:485–488. PMID: 16306834.
29. Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries : the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005; 30:2325–2333. PMID: 16227897.
30. Wang XY, Dai LY, Xu HZ, Chi YL. Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine. 2008; 8:246–254. PMID: 18312076.

Fig. 1
Schematic diagram of radiological parameters measured on a lateral neutral radiograph. Vertebral body compression ration : [1-(2×body height 2)/(body height 1+3)]×100. CA : Cobb angle, VWA : vertebral wedge angle, DbVC : difference between VWA and CA, UADH : upper anterior disc height, LADH : lower anterior disc height, PDH : posterior disc height.
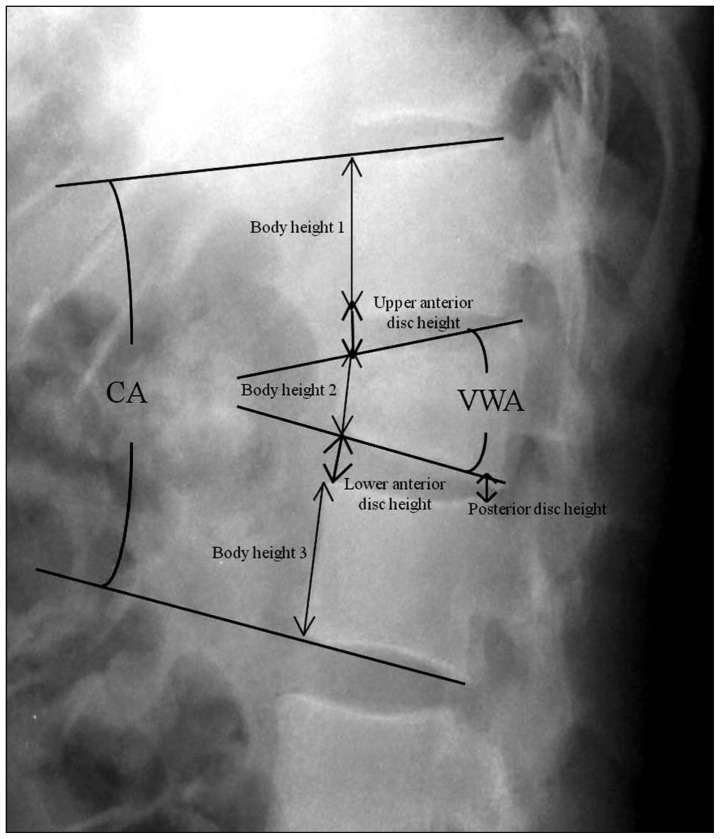
Fig. 2
Radiographs obtained in a 36-year-old man demonstrating an L2 burst fracture. A : Preoperatively, the Cobb angle measured 20.1 degrees and the vertebral wedge angle is 30.5 degrees. The difference between vertebral wedge angle and Cobb angle (DbVC) is 10.4. B : Postoperatively, the Cobb angle and the vertebral wedge angle are reduced to 6.6 degrees and 15.8 degrees. C : In the last follow-up radiograph, kyphosis recurrence is observed with a decline of the adjacent anterior disc height of fractured vertebra.
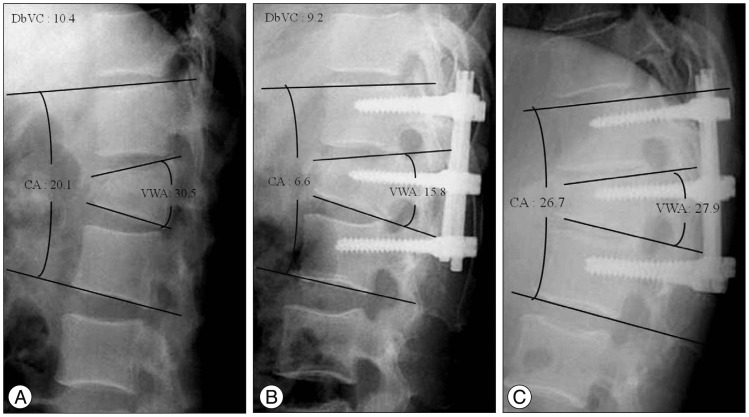
Fig. 3
Radiographs obtained in a 53-year-old man demonstrating an L1 burst fracture. A : Preoperatively, the Cobb angle measured 27.9 degrees and the vertebral wedge angle is 29.7 degrees. B : Preoperatively, computed tomography (CT) scan shows severe comminution of fractured vertebral body. C : Postoperatively, the Cobb angle and the vertebral wedge angle are reduced to 13.8 degrees and 15.5 degrees. Load-sharing classification score is 8 points. D : In the last follow-up radiograph, 9.4 degrees of correction loss is observed with an additional collapse of fractured vertebra.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download