Abstract
Extra-axial medulloblastoma is a rare phenomenon. We report a case in a 5-year-old boy who presented with nausea, vomiting, and gait disturbance. He was treated with total removal of the tumor. This is the first case of an extra-axially located medulloblastoma occurring in the cerebellar hemisphere posteriolateral to the cerebellopontine angle in Korea. Although the extra-axial occurrence of medulloblastoma is rare, it should be considered in the differential diagnosis of extra-axial lesions of the posterior fossa in children.
Medulloblastomas are commonly occurring tumors in the cerebellar vermis in children. Most are located in the midline of the cerebellum and are commonly seen in the pediatric age group12). However, the tumor can be rarely situated extra-axially. Previously, 33 cases of medulloblastomas located extra-axially have been reported7), but most extra-axial medulloblastomas occurred at the cerebellopontine angle (CPA). Ours is the first case in Korea in which a medulloblastoma was entirely located in the cerebellar hemisphere.
A 5-year-old boy presented with nausea, vomiting, and gait disturbance 5 days in duration. The initial neurologic exam revealed terminal ataxia, dysmetria, and tandem gait.
Brain magnetic resonance imaging (MRI) depicted a well-defined, oval mass in the left posterior fossa measuring about 5.1×3.1×4.6 cm. The mass was compressing the fourth ventricle, causing hydrocephalus. Given its extra-axial location and homogeneous pattern of contrast uptake, we considered a differential diagnosis of hemangiopericytoma or meningioma.
The mass abutted upon the meninges and evidenced iso-SI with gray matter on T2-weighted imaging and T1-weighted imaging. Following the infusion of contrast media, the mass exhibited well-contrasted enhancement (Fig. 1). The left cerebellar hemisphere appeared compressed by the mass, and resultant surrounding parenchymal edema and compression of the fourth ventricle were evident. Dilatation of the 3rd and both lateral ventricles was observed.
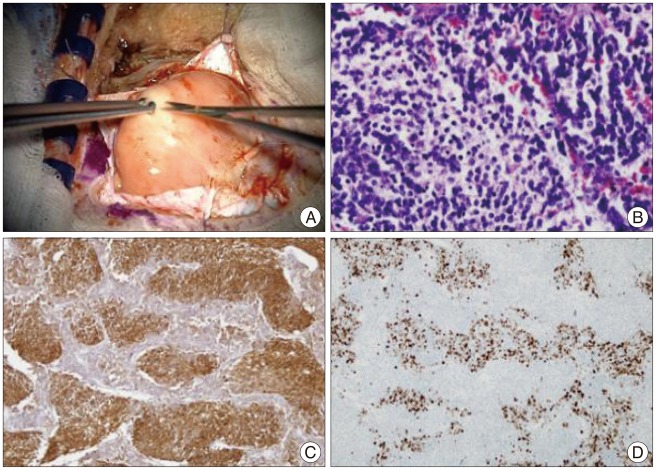
An emergency operation was performed. An external ventricular drain was used to control increased intracranial pressure, and a left lateral suboccipital, infratentorial craniotomy was performed for tumor resection. Macroscopically, a soft, well-demarcated mass was observed extra-axially, attached to the dura next to the transverse-sigmoid sinus with invasion into the cerebellar hemisphere (Fig. 2A). A gross total surgical excision was performed.
Microscopically, the tumor consisted of pale nodular areas and a surrounding dark cellular area with reticulin framework, which is consistent with desmoplastic/nodular type medulloblastoma (WHO grade IV) (Fig. 2B). The pale nodular areas contained tumor cells with low nuclear cytoplasmic ratio and neuronal maturation shown by neuron-specific enolase (Fig. 2C). The dark cellular areas were highly cellular with a high nuclear cytoplasm ratio and increased Ki67 proliferative index (Fig. 2D). The tumor cells exhibited no immunoreactivity for GFAP or epithelial membrane antigen.
MRI following surgery revealed no evidence of remnant enhancing lesion in the left posterior fossa. Also, MRI of the spinal cord showed no definitive evidence of CSF seeding of the tumor. The postoperative course was marked by rapid resolution of symptoms. Since medulloblastomas are very radio-sensitive, we considered post-op radiotherapy applied to the whole cranio-spinal axis to prevent tumor recurrence.
The term "medulloblastoma" refers to cerebellar tumors belonging to the family of primitive neuroectodermic tumors10). Medulloblastomas usually occur in the midline; however, they may rarely occur extra-axially. Although the cellular origin of medulloblastoma is still controversial, it may originate either from germinal cells or their remnants, situated at the end of the posterior medullary velum14), or from remnants of the external granular layer16). Cells originating in the neuroepithelial roof of the fourth ventricle migrate upward and laterally to form the external granular layer of the cerebellum5). Kadin et al.8) suggested that medulloblastomas arise from germinal cells (or their remnants) anywhere along their migratory path, and because the migratory process normally proceeds in a lateral direction, a relatively higher frequency of laterally-situated tumors should be observed in adults.
In this report, we present a rare case of a primary extra-axial medulloblastoma occurring in the cerebellum hemisphere. Extra-axial medulloblastomas are rare, and only 33 cases have been previously reported1,2,4,6,9,10,11,15,17,18,19). Most of the reported extra-axial medulloblastomas occurred at the CPA.
Medulloblastomas have long been classified into two chief histological variants, "classical" and "desmoplastic". Other variants of medulloblastoma, such as extensive nodularity, anaplastic, and large-cell, are rarer.
Pramanik et al.13) reviewed a total of 181 cases of medulloblastoma obtained from medical records for a 10-year period. Comparative evaluations of 87 classical medulloblastoma cases and 43 desmoplastic medulloblastoma cases were performed. The desmoplastic variant has been reported to occur more frequently among extra-axial tumors, as in our case.
However, the relationship between histologic types of medulloblastomas and their location is unclear and should be further studied.
The treatment and prognosis of extra-axial medulloblastoma are still uncertain because of the small number of reported cases. Among 33 patients, follow-up was available only in 4 cases and ranged from 2 months to 1 year. During follow-up, recurrence was noted in one case, and another patient received post-op chemotherapy due to malignant meningitis. The remaining two patients were symptom-free at last follow-up.
The major prognostic factors of medulloblastoma include fourth ventricular floor involvement, histologic subtype, radiation dose, and post-op functional status13). In particular, the desmoplastic type is known to have a better prognosis due to its stable DNA pattern3).
Kumar et al.9) described 4 pediatric cases of medulloblastoma, and only 1 of the 4 patients survived and was symptom-free, while the others succumbed to the disease within a short follow-up period of only 30 months. This may suggest the higher malignant potential of CPA medulloblastomas compared to midline medulloblastomas; however, there is currently no clear-cut consensus as to whether extra-axially located medulloblastomas are more aggressive compared to their midline counterparts.
A larger number of cases and longer follow-up periods are needed to understand the relationship between tumor location and prognosis.
The extra-axial occurrence of medulloblastoma is extremely rare, but must be considered in the differential diagnosis of extra-axial lesions. Most extra-axial medulloblastomas occur at the CPA; however, extra-axial medulloblastomas can also occur in the cerebellar hemisphere, such as in this case. This is the first case of an extra-axially located medulloblastoma occurring in the cerebellar hemisphere posteriolateral to the cerebellopontine angle in Korea. Clinically, it is very difficult to distinguish these neoplasms from other extra-axial lesions, although we should always keep in mind the possible occurrence of medulloblastoma.
Total surgical excision followed by radio- and/or chemotherapy is necessary in all cases of medulloblastoma to prevent tumor recurrence.
References
1. Brackmann DE, Bartels LJ. Rare tumors of the cerebellopontine angle. Otolaryngol Head Neck Surg (1979). 1980; 88:555–559. PMID: 6969383.

2. Britton BH. Adult medulloblastoma : neurotologic manifestations. Ann Otol Rhinol Laryngol. 1975; 84(3 Pt 1):364–367. PMID: 1079441.
3. Chatty EM, Earle KM. Medulloblastoma. A report of 201 cases with emphasis on the relationship of histologic variants to survival. Cancer. 1971; 28:977–983. PMID: 5111749.

4. Ehrenberger K. Endoscopy of the cerebellopontine angle. Endoscopy. 1978; 10:260–264. PMID: 310770.

5. Fujita S, Shimada M, Nakamura T. H3-thymidine autoradiographic studies on the cell proliferation and differentiation in the external and the internal granular layers of the mouse cerebellum. J Comp Neurol. 1966; 128:191–208. PMID: 5970298.

6. House JL, Burt MR. Primary CNS tumors presenting as cerebellopontine angle tumors. Am J Otol. 1985; (Suppl):147–153. PMID: 3878087.
7. Jaiswal AK, Mahapatra AK, Sharma MC. Cerebellopointine angle medulloblastoma. J Clin Neurosci. 2004; 11:42–45. PMID: 14642364.

8. Kadin ME, Rubinstein LJ, Nelson JS. Neonatal cerebellar medulloblastoma originating from the fetal external granular layer. J Neuropathol Exp Neurol. 1970; 29:583–600. PMID: 5471923.

9. Kumar R, Achari G, Mishra A, Chhabra DK. Medulloblastomas of the cerebellopontine angle. Neurol India. 2001; 49:380–383. PMID: 11799412.
10. Mohan M, Pande A, Vasudevan MC, Ramamurthi R. Pediatric medulloblastoma : a review of 67 cases at a single institute. Asian J Neurosurg. 2008; 2:63–69.
11. Naim-ur-Rahman , Jamjoom A, al-Rayess M, Jamjoom ZA. Cerebellopontine angle medulloblastoma. Br J Neurosurg. 2000; 14:262–263. PMID: 10912209.

12. Park TS, Hoffman HJ, Hendrick EB, Humphreys RP, Becker LE. Medulloblastoma : clinical presentation and management. Experience at the hospital for sick children, toronto, 1950-1980. J Neurosurg. 1983; 58:543–552. PMID: 6827349.
13. Pramanik P, Sharma MC, Mukhopadhyay P, Singh VP, Sarkar C. A comparative study of classical vs. desmoplastic medulloblastomas. Neurol India. 2003; 51:27–34. PMID: 12865511.
14. Raaf J, Kernohan JW. Relation of abnormal collections of cells in posterior medullary velum of cerebellum to origin of medulloblastoma. Arch Neurol Psychiatry. 1944; 52:163–169.

15. Ringertz N, Tola JH. Medulloblastoma. J Neuropathol Exp Neurol. 1950; 9:354–372. PMID: 14784854.

16. Stevenson L, Echlim F. Nature and origin of some tumors of cerebellum : Medullobastoma. Arch Neurol Psychiatry. 1934; 31:93–109.
17. Weisberg LA. Computerized tomographic findings in medulloblastomas. Comput Radiol. 1982; 6:83–91. PMID: 7083845.

18. Yamada S, Aiba T, Hara M. Cerebellopontine angle medulloblastoma : case report and literature review. Br J Neurosurg. 1993; 7:91–94. PMID: 8435152.

19. Zee CS, Segall HD, Miller C, Ahmadi J, McComb JG, Han JS, et al. Less common CT features of medulloblastoma. Radiology. 1982; 144:97–102. PMID: 6979760.

Fig. 1
A well-defined, oval mass in the left posterior fossa measuring about 5.1×3.1×4.6 cm. The mass is compressing the fourth ventricle, causing hydrocephalus. A : Gadolium-enhanced axial T1-weighted MRI. B : Gadolium-enhanced coronal T1-weighted MRI.
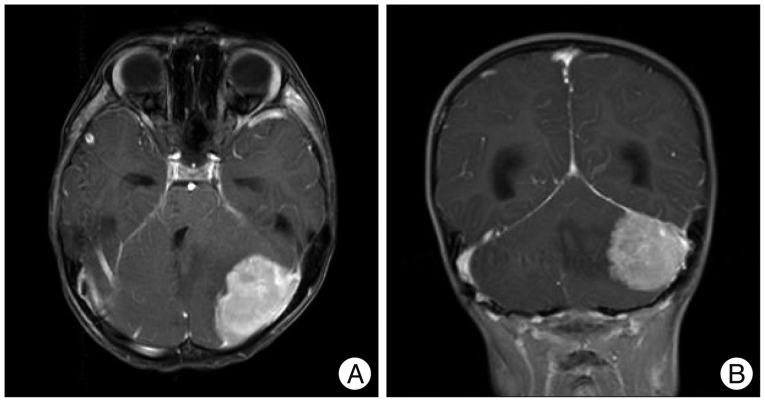
Fig. 2
A : A soft, well-demarcated mass is observed extra-axially, attached to the dura next to the transverse-sigmoid sinus with invasion into the cerebellar hemisphere. B : The pale nodular areas contain tumor cells having low nuclear cytoplasmic ratio and the dark cellular areas are highly cellular with a high nuclear cytoplasm ratio (H&E, ×400). C : The pale area showing immunoreactivity for neuron specific enolase (×100). D : The dark cellular areas showing high Ki67 proliferative index (×100).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download