Abstract
Traumatic intracranial aneurysms (TICAs) are rare and are associated with high rates of morbidity and mortality. TICAs usually result from head injuries caused by traffic accidents, industrial accidents, or gunshots. We report a traumatic aneurysm of the callosomarginal artery-cortical artery junction arising from a penetrating injury by scissors. A 51-year-old woman was admitted to our hospital after suffering a penetrating injury caused by scissors. Computed tomography (CT) and CT-angiography demonstrated a right orbital roof fracture, subarachnoid hemorrhage, frontal lobe hemorrhage, intraventricular hemorrhage, and a traumatic aneurysm of the right callosomarginal artery-cortical artery junction. We trapped the traumatic aneurysm and repositioned a galeal flap. Postoperative CT showed a small infarction in the left frontal lobe. Follow-up angiography two months later showed no residual aneurysm. We suggest that an aggressive surgical intervention be performed whenever TICA is diagnosed.
Traumatic intracranial aneurysms (TICAs) are rare and constitute less than 1% of all aneurysms in large series3,14,20). TICAs have been reported in almost all major intracranial arteries but are most common in the middle cerebral and pericallosal arteries3,20). There are very few reports in the literature of TICAs of the callosomarginal artery (CM)9,12). The most frequent causes of peripheral TICAs are closed head trauma (62%), penetrating wounds (27%), and iatrogenic trauma (11%)2). Penetrating orbitocranial injuries are quite common in military practice, but they are very rarely seen in civilian life, where they are predominantly accidental injuries10).
Penetrating orbitocranial injuries caused by nonmissile low-velocity bodies constitute a rare subgroup, which has special features. Penetrating object injuries that occur when the victim falls onto a penetrating object, such as a nail, are encountered rarely1,4), and we have found only three reports of penetrating intracranial injury by scissors8,15,21).
We report a TICA of the CM-cortical artery (CM-CA) junction caused by a penetrating injury with scissors. We discuss its diagnosis and treatment.
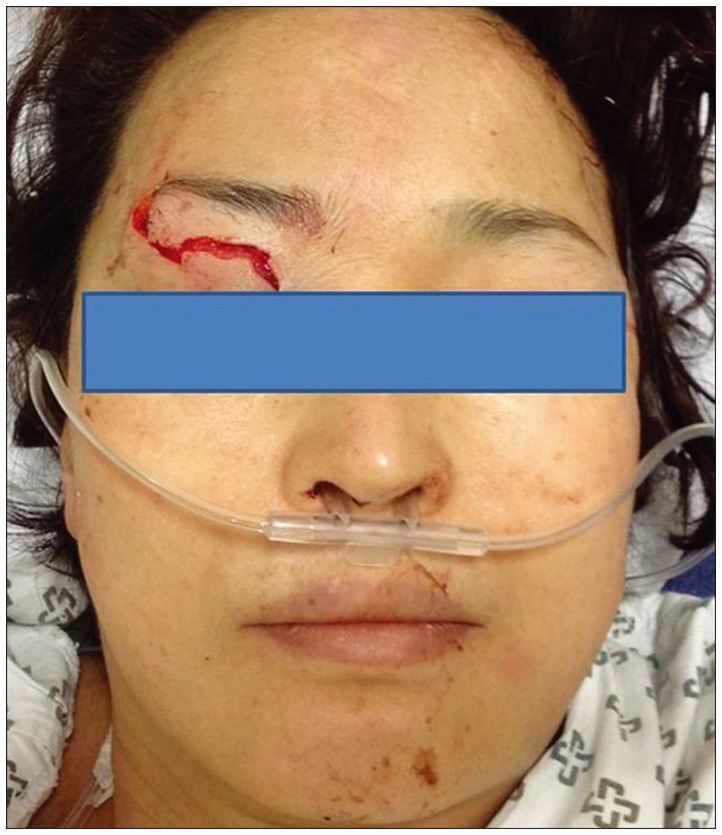
A 51-year-old woman visited to our hospital after suffering a penetrating injury with scissors. Another person at accident place had removed the scissors immediately (Fig. 1). A physical examination in an emergency department demonstrated a laceration wound in the right upper eyelid (Fig. 2). A neurological examination upon admission revealed a drowsy mental state, neck stiffness, but no weakness. Computed tomography (CT) one hour later from accident revealed subarachnoid hemorrhage, frontal lobe hemorrhage, and intraventricular hemorrhage (Fig. 3). The scissors entered the skull through the right orbital roof and crossed the midline of the brain. Because the trajectory crossed the midline and there was subarachnoid hemorrhage, a CT-angiographic examination was performed eight hours later from accident. A TICA at the right CM-CA junction was identified (Fig. 4). We made a bicoronal incision and performed an interhemispheric approach two days later. We identified a skull defect in the anterior cranial fossa and repaired it with a galeal flap. After the hematoma adjacent to the TICA was removed, acute bleeding developed from the CM-CA junction. We identified two ruptured sites at left side wall of cortical artery and two injured sites at right side wall of cortical artery. Ruptured sites of cortical artery led to cystic dilation of CM-CA lumen. We trapped the TICA at the right CM-CA junction including ruptured and injured sites of CM-CA junction (Fig. 5). Proximal clip was applied to CM-CA junction and distal one to cortical artery. Proximal clipping resulted to partial stenosis of CM lumen but preserved flow in CM. Postoperative CT showed a small infarction in the left frontal lobe (Fig. 6). The patient developed postoperative meningitis due to methicillin-resistant coagulase-negative Staphylococcus and demonstrated behavioral changes. However, these symptoms were improved after the administration of vancomycin and conservative treatment. Follow-up angiography performed two months later showed no residual aneurysm and a preserved right callosomarginal arterial flow but no flow in one cortical artery (Fig. 7).
In injuries that penetrate the orbit, the three most frequent routes by which foreign bodies penetrate the cranium are through the orbit roof, the superior orbital fissure, or the optic canal6,17,22). The most frequent route is via the orbital roof because the superior orbital plate of the frontal bone is fragile17), and during the injury, patients extend their heads backwards, exposing the orbital roof6). Such penetration often leads to frontal lobe contusion. Penetration through the roof of the orbit may also affect the circle of Willis, and especially the anterior cerebral arteries. The second most frequent site of penetration is the superior orbital fissure17,22). Penetration through the superior orbital fissure may result in a lesion of the carotid artery, which can lead to a carotid-cavernous fistula or lesion of the occipital lobe13).
In our patient, the scissors penetrated the right orbital roof, and we suspected a traumatic aneurysm in this case for two reasons : the presence of subarachnoid hemorrhage and because the trajectory of the scissors crossed the midline. When a penetrating orbital or cranial injury is suspected, CT is considered the primary diagnostic examination11). Angiography is required to identify the site of injury to the intracranial vascular structures11).
TICAs have been classified by Burton et al.5) according to the type of aneurysm produced, which include true aneurysms (partial disruption of the arterial wall), false aneurysms (or pseudoaneurysms; cavity in the encapsulated hematoma communicates with the lumen of the artery), and mixed aneurysms (rupture of a true aneurysm generates a secondary false aneurysm). In our patient, the type of TICA was pseudoaneurysm. Two ruptured sites of CM-CA junction were partial disruption of the arterial wall and had no true aneurysm. Cystic dilation of CM-CA junction was composed with hematoma and disrupted vessel wall.
When a patient who has suffered a penetrating head injury caused by scissors is taken to hospital, the general surgeon should not attempt to remove the foreign body. Previous reports have described frantic, unsuccessful efforts to extract scissors8,11,21). The notching of the scissor blades can catch on the skull, making their withdrawal difficult21). When someone tried to extract scissors too roughly, the tip of the scissors broke off and lodged in the brain15). In our case, person at accident place had removed the scissors from our patient.
With craniocerebral injuries of this type, there is a major risk of infection, with the direct infiltration of pathogens into the meningeal spaces or the cerebral parenchyma7). Infectious complications may arise from the presence of a contaminated foreign body or injury to a frontal sinus, or they can originate on the skin18). In our patient, early radical debridement was mandatory to prevent potentially fatal infectious complications. We consider that the patient's meningitis was easily controlled because the early operation provided massive irrigation and the anterior cranial fossa was repaired with a galeal flap. The removed scissors might also had been contaminated with a low-virulence pathogen. Contamination with a Gram-negative or a more virulent Gram-positive bacterium may have resulted in a more complex situation.
In the case of nonmissile penetrating orbitocranial injuries, every effort should be made to find and remove any retained foreign body, because the risk of cerebral infection is high6).
TICAs of the CM tend to rupture and should be managed with aggressive treatment. Yokota et al.24) suggested that clinicians should manage TICAs aggressively based on their observation that a nonsurgical treatment group had a mortality rate of 40%, about four times higher than the corresponding rate for a surgical group of 11%. Therefore, we suggest that all TICAs be treated aggressively.
TICAs are often fragile and prone to rupture, and therefore present a challenging subset of vascular lesions for either surgical or endovascular therapy23). In our patient, neck clipping was difficult because the aneurysm had no defined aneurysmal neck. In the acute phase, the wall of a TICA can be extremely fragile. In contrast, after a few weeks (in the subacute stage), the wall of a TICA is presumed to be more stable because the aneurysm wall contains fibroblasts and other elements that strengthen and encapsulate the wall16). However, the rerupture rate for pseudoaneurysms or dissecting aneurysms is much higher in the acute stage19). Therefore, a delayed operation strategy entails a risk of rerupture.
The surgical treatment of TICAs without sacrificing the parent artery can be extremely difficult, depending on the location of the TICA. In our patient, neck clipping was difficult because the aneurysm had a poorly defined neck and the parent artery could not be trapped without sacrificing a parent artery. Sacrifice of one cortical artery resulted to small infarction of frontal lobe.
Acknowledgements
This work was supported by research grant from an Inje University College of Medicine.
This article was presented as poster in 26th annual meeting of Korean Society of Cerebrovascular Surgeons on February 15-16, 2013.
References
1. Agrillo A, Sassano P, Mustazza MC, Filiaci F. Complex-type penetrating injuries of craniomaxillofacial region. J Craniofac Surg. 2006; 17:442–446. PMID: 16770179.

2. Asari S, Nakamura S, Yamada O, Beck H, Sugatani H. Traumatic aneurysm of peripheral cerebral arteries. Report of two cases. J Neurosurg. 1977; 46:795–803. PMID: 859016.
3. Benoit BG, Wortzman G. Traumatic cerebral aneurysms. Clinical features and natural history. J Neurol Neurosurg Psychiatry. 1973; 36:127–138. PMID: 4691685.

4. Bilotta F, Rosa G, Delfini R, Pinto R, Fiorani B. Unrecognized periorbital penetrating nail in the brain : case report. Am J Emerg Med. 2007; 25:198–199. PMID: 17276812.
5. Burton C, Velasco F, Dorman J. Traumatic aneurysm of a peripheral cerebral artery. Review and case report. J Neurosurg. 1968; 28:468–474. PMID: 5659574.
6. Chibbaro S, Tacconi L. Orbito-cranial injuries caused by penetrating non-missile foreign bodies. Experience with eighteen patients. Acta Neurochir (Wien). 2006; 148:937–941. discussion 941-942. PMID: 16763734.

7. Di Roio C, Jourdan C, Mottolese C, Convert J, Artru F. Craniocerebral injury resulting from transorbital stick penetration in children. Childs Nerv Syst. 2000; 16:503–506. discussion 507. PMID: 11007502.

8. Dooling JA, Bell WE, Whitehurst WR Jr. Penetrating skull wound from a pair of scissors. Case report. J Neurosurg. 1967; 26:636–638. PMID: 6027450.
9. Endo S, Sato S, Uneoka K, Takaku A, Suzuki J. [Traumatic aneurysm of the callosomarginal artery : case report (author's transl)]. No Shinkei Geka. 1974; 2:329–336. PMID: 4473746.
10. Erkutlu I, Alptekin M, Dokur M, Geyik M, Gök A. Unusual penetration of a construction nail through the orbit to the cranium : a case report. Ulus Travma Acil Cerrahi Derg. 2011; 17:79–82. PMID: 21341140.

11. Hansen JE, Gudeman SK, Holgate RC, Saunders RA. Penetrating intracranial wood wounds : clinical limitations of computerized tomography. J Neurosurg. 1988; 68:752–756. PMID: 3357035.

12. Jakobsson KE, Carlsson C, Elfverson J, von Essen C. Traumatic aneurysms of cerebral arteries. A study of five cases. Acta Neurochir (Wien). 1984; 71:91–98. PMID: 6731059.

13. Kahler RJ, Tomlinson FH, Eisen DP, Masel JP. Orbitocranial penetration by a fern : case report. Neurosurgery. 1998; 42:1370–1373. PMID: 9632198.
14. Kassell NF, Torner JC, Haley EC Jr, Jane JA, Adams HP, Kongable GL. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1 : Overall management results. J Neurosurg. 1990; 73:18–36. PMID: 2191090.
15. Kumar A, Pandey R, Singh K, Sharma V. Scissors in brain : an unusual presentation of tribal culture in India. Turk Neurosurg. 2011; 21:413–417. PMID: 21845581.
16. Lempert TE, Halbach VV, Higashida RT, Dowd CF, Urwin RW, Balousek PA, et al. Endovascular treatment of pseudoaneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 1998; 19:907–911. PMID: 9613510.
17. Matsumoto S, Hasuo K, Mizushima A, Mihara F, Fukui M, Shirouzu T, et al. Intracranial penetrating injuries via the optic canal. AJNR Am J Neuroradiol. 1998; 19:1163–1165. PMID: 9672032.
18. Miller CF, Brodkey JS, Colombi BJ. The danger of intracranial wood. Surg Neurol. 1977; 7:95–103. PMID: 835079.
19. Mizutani T, Aruga T, Kirino T, Miki Y, Saito I, Tsuchida T. Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995; 36:905–911. discussion 912-913. PMID: 7791980.

20. Nakstad P, Nornes H, Hauge HN. Traumatic aneurysms of the pericallosal arteries. Neuroradiology. 1986; 28:335–338. PMID: 3762911.

21. Schneider RC. Head injuries in infancy and childhood. Surg Clin North Am. 1961; 41:1255–1269. PMID: 13908953.

22. Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury : case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011; 114:53–61. PMID: 20868210.

23. Yang TC, Lo YL, Huang YC, Yang ST. Traumatic anterior cerebral artery aneurysm following blunt craniofacial trauma. Eur Neurol. 2007; 58:239–245. PMID: 17851246.

24. Yokota H, Tazaki H, Murayama K, Shimura T, Higuchi H, Yajima K, et al. [Traumatic cerebral aneurysm : 94 cases from the literature and 5 cases observed by the authors]. No Shinkei Geka. 1983; 11:521–528. PMID: 6877511.
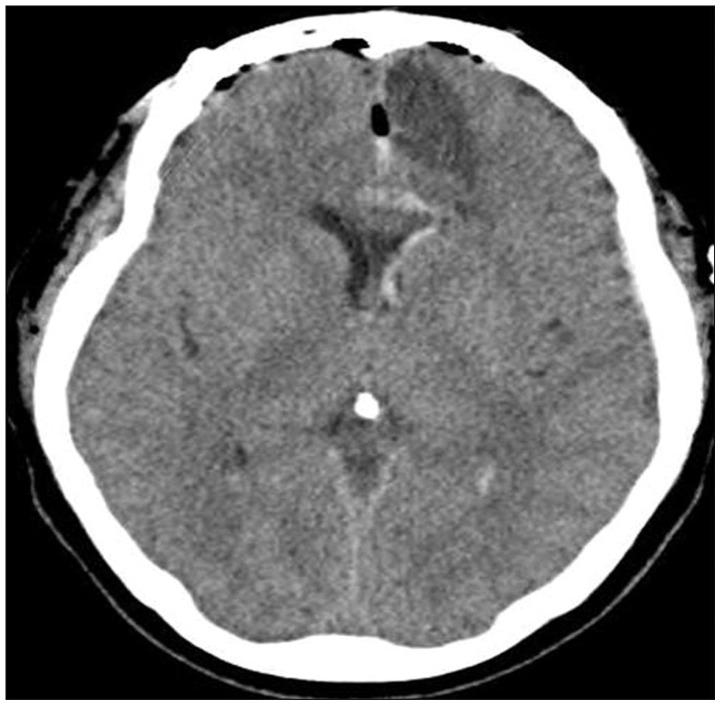
Fig. 3
Computed tomography in the emergency department shows subarachnoid hemorrhage, frontal lobe hemorrhage, and intraventricular hemorrhage.

Fig. 4
Computed tomography-angiography shows fracture of the right orbital roof and a traumatic aneurysm of the callosomarginal artery-cortical artery junction [1 : right orbital fracture, 2 : right callosomarginal artery, 3 : right pericallosal artery (A4), 4 : traumatic anerusym, 5 : right long callosal artery, 6 : right pericallosal artey (A2), 7 : left pericallosal artery (A2), 8 : cortical artery].
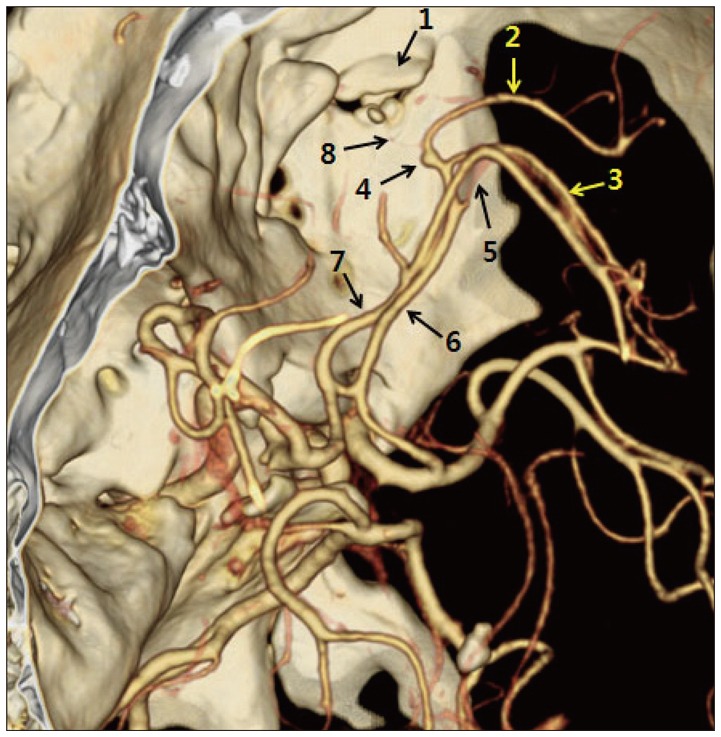
Fig. 5
Intraoperative findings. This figure shows the trapping of the pseudoaneurysm of callosomarginal artery-cortical artery junction (arrow : cortical artery, red dotted line : callosomarginal artery, curved arrow : cystic dialation of cortical artery, red arrow : ruptured site, black dotted line : blade of proximal clip).
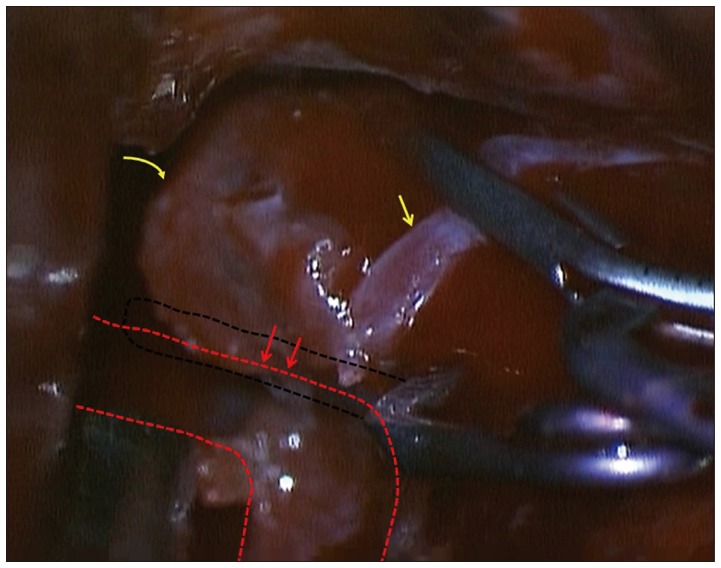
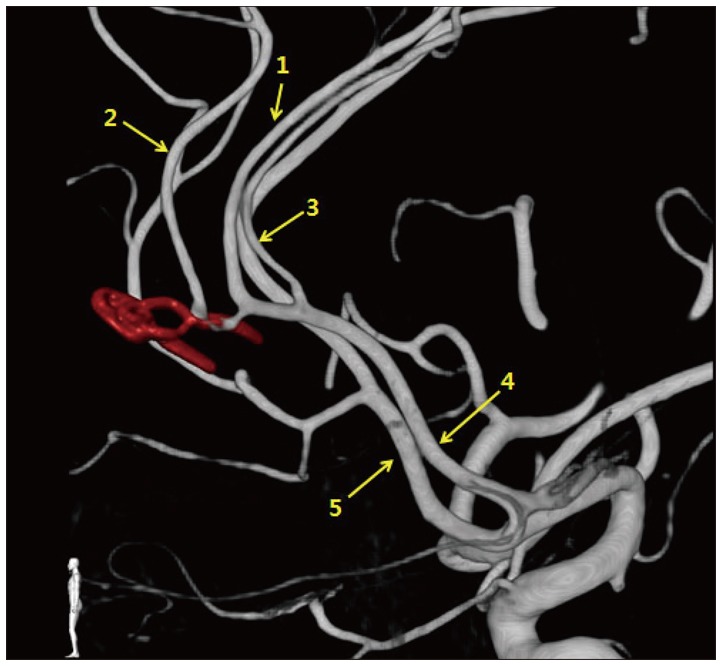
Fig. 7
Internal carotid angiography two months later demonstrates no flow in one cortical artery, but preserved flow in and stenosis of the right callosomarginal artery [1 : right pericallosal artery (A4), 2 : right callosomarginal artery, 3 : right long callosal artery, 4 : right pericallosal artery (A2), 5 : left pericallosal artery (A2)].




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download