Abstract
Giant cell tumor (GCT) of the spine is a rare benign tumor, but can be aggressive and can exhibit a high local recurrence rate. Furthermore, GCT of the upper thoracic spine may pose diagnostic and management difficulties. Here, we report a rare case of GCT of the upper thoracic spine with soft tissue extension to the spinal canal. The patient was managed by decompressive laminectomy and posterolateral fusion followed by an injection of polymethylmethacrylate into the vertebral lesion. The patient recovered clinically and showed radiological improvement after surgical treatment without tumor recurrence at his last follow-up of postoperative 7 years. We present this unusual case of GCT and include a review of the literature.
Giant cell tumors (GCTs) of the spine are generally considered benign, but they can be aggressive with high rate of local recurrence5,7). Recurrence may exacerbate neurologic deficits, increase management difficulties, and even lead to death when the opportunity for reoperation is missed. For this reason, complete surgical resection is recommended to reduce the risk of recurrence. However, the surgical approach to anterior lesions in the upper thoracic spine is troublesome, because of the physical constraints imposed by the sternum, thoracic kyphosis, narrowness of the spinal canal, and presence of major vessels. Here, we describe a patient who recovered from clinically and showed radiological improvement T4 GCT after injecting polymethylmethacrylate (PMMA) into a vertebral lesion following decompressive laminectomy and posterolateral fusion.
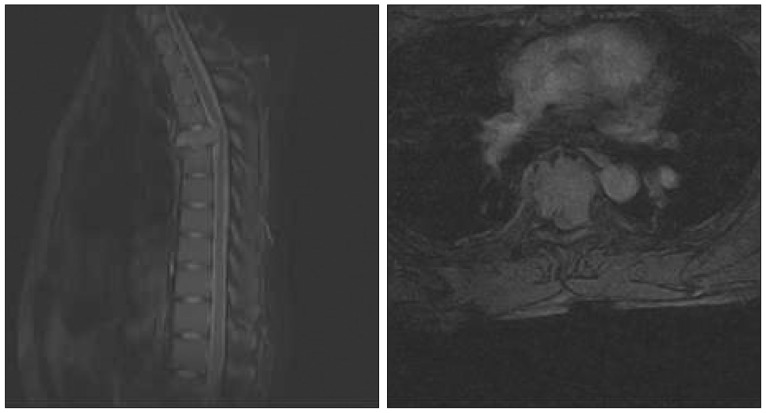
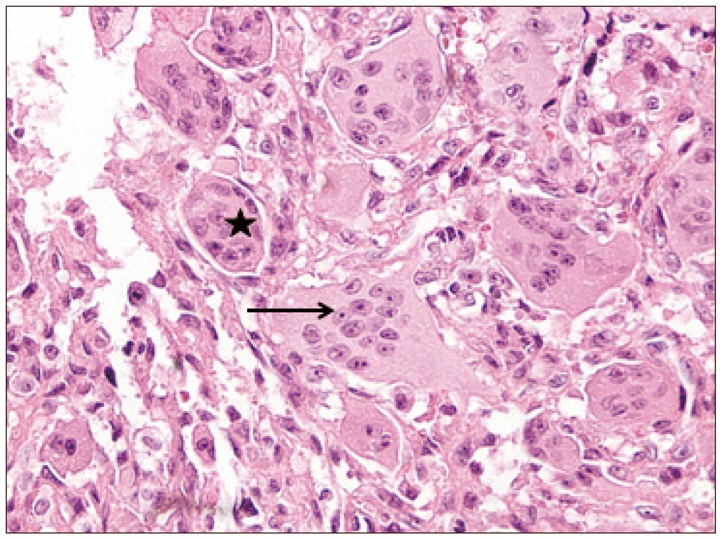
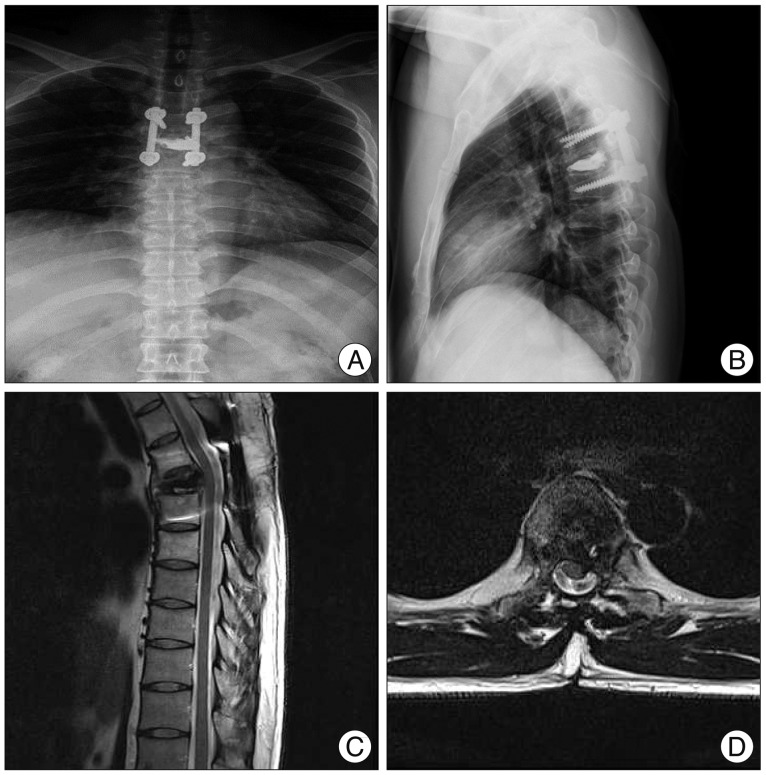
A 20-year-old man presented with a 2-month history of severe upper thoracic pain, which was followed by complaints of referred pain in the anterior chest. Physical examination revealed mild tenderness on palpation in the upper thoracic region. He did not feel any fabrile sensation, and the results of laboratory blood tests including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were all within normal limits. Computed tomography (CT) revealed destruction of the T4 vertebra, but intact disc spaces at T3-4 and T4-5 (Fig. 1). Magnetic resonance imaging (MRI) showed an extensive neoplastic process at T4 with destruction of the vertebral body and cord compression (Fig. 2). Based on these clinical symptoms and radiological findings, and under a preliminary diagnosis of a primary or metastatic bone tumor, CT-guided transpedicular biopsy of the T4 lesion was performed. The color of aspirated solid material was bright brown in appearance, and it was forwarded for histopathological examination. The bone marrow specimen showed multinuclear giant cells (Fig. 3). Due to the patient's intractable pain, surgical treatment was performed using a posterior approach. Decompressive laminectomy and posterolateral fusion of T3-5 followed by a 7 cc PMMA injection at T4 were performed. Immediately after surgery, the intractable upper thoracic pain disappeared. He has since been followed uneventfully for 7 years with no subjective complaints or evidence of recurrence (Fig. 4).
GCT of bone is an uncommon neoplasm that accounts for about 4% of all primary bone tumors, and isolated intravertebral GCT is rare among GCTs4). Most GCTs of the spine occur in the sacrum, followed in order of decreasing frequency by the thoracic, cervical, and lumbar segments with female predominance2). Due to a potentially aggressive behavior, the most important management issue is the prevention of recurrence. Treatment options include surgical resection of affected segment of bone with or without the adjuvant therapy, such as, phenol, alcohol, liquid nitrogen, methylmethacrylate, or bone grafting9). Complete surgical resection is the foundational treatment strategy for GCT of the spine, as it is presumed that complete removal of an entire osseous compartment improves prognosis. Some authors have reported that total en bloc spondylectomy of intravertebral GCT results in an excellent prognosis1,3). However, total en bloc spondylectomy is near impossible in upper thoracic region because of anatomical complexity and the physical constraints imposed by the sternum and surrounding major blood vessels and visceral organs. Bone cement injection into spine tumors by vertebroplasty is used to relieve intractable pain, because it gives mechanical stabilization of bone, destruction of sensitive nerve endings, and the induction of tumor necrosis8). Actually, bone cement is also injected into bone lesions as an adjuvant therapy, for example, after surgery to treat GCTs10). Paúl et al.6) reported complete necrosis of a GCT after vertebroplasty, and postulated that cement-induced tumor necrosis was due to the cytotoxic effects of PMMA monomer and tissue hyperthermia caused by the heat generated during polymerization. We also achieved clinical and radiological improvement after decompressive laminectomy and posterolateral fusion followed by an injection of PMMA. However, as GCTs of the spine are rare, scientific communication and multicenter studies on this disease entity are required to determine the effectiveness of PMMA as an adjuvant therapy.
We report a rare case of an upper thoracic giant cell tumor that was difficult to treat by en-bloc spondylectomy. Our experience suggests that bone cement injection offers an adjuvant strategy that may enhance the efficacy of treatment for GCT when complete en bloc spondylectomy is difficult.
References
1. Bertoni F, Bacchini P, Staals EL. Malignancy in giant cell tumor of bone. Cancer. 2003; 97:2520–2529. PMID: 12733152.

2. Bidwell JK, Young JW, Khalluff E. Giant cell tumor of the spine : computed tomography appearance and review of the literature. J Comput Tomogr. 1987; 11:307–311. PMID: 3608560.
3. Hart RA, Boriani S, Biagini R, Currier B, Weinstein JN. A system for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine (Phila Pa 1976). 1997; 22:1773–1782. discussion 1783. PMID: 9259790.
4. Hwang GJ, Kim KN, Yoon DH, Yang WI. Total spondylectomy for giant cell tumor of cervical spine. J Korean Neurosurg Soc. 2003; 34:262–264.
5. Larsson SE, Lorentzon R, Boquist L. Giant-cell tumors of the spine and sacrum causing neurological symptoms. Clin Orthop Relat Res. 1975; (111):201–211. PMID: 1157418.

6. Paúl L, Santonja C, Izquierdo E. Complete necrosis of a spinal giant cell tumor after vertebroplasty. J Vasc Interv Radiol. 2006; 17:727–731. PMID: 16614158.

7. Sanjay BK, Sim FH, Unni KK, McLeod RA, Klassen RA. Giant-cell tumours of the spine. J Bone Joint Surg Br. 1993; 75:148–154. PMID: 8421014.

8. Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases : indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996; 199:241–247. PMID: 8633152.

9. Yan SC, Xu QM, Lin JR. Diagnosis and treatment of giant cell tumor in the thoracic spine. J Surg Oncol. 1989; 40:128–131. PMID: 2492623.

10. Zhen W, Yaotian H, Songjian L, Ge L, Qingliang W. Giant-cell tumour of bone. The long-term results of treatment by curettage and bone graft. J Bone Joint Surg Br. 2004; 86:212–216. PMID: 15046435.
Fig. 1
Sagittal (A) and 3-dimensional (B) computed tomographs reveal bony destruction involving the T4 vertebral body.
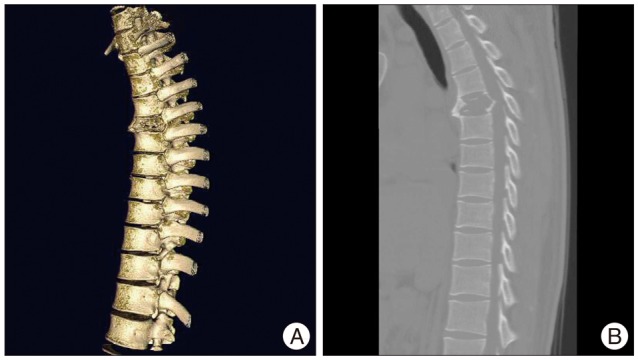
Fig. 2
T2-weighted magnetic resonance images show a neoplastic lesion extensively involving the T4 vertebra with cord compression.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download