Abstract
Intramuscular stimulation (IMS) is widely used to treat myofascial pain syndrome. IMS is a safe procedure but several complications have been described. To our knowledge, spinal subarachnoid hematoma has never been reported as a complication of an IMS. The authors have experienced a case of spinal subarachnoid hematoma occurring after an IMS, which was tentatively diagnosed as intracranial subarachnoid hemorrhage because of severe headache. Patient was successfully treated with surgery. Here, we report our case with a review of literature.
Deep dry needing (DDN) is one of the newest treatment modalities for the management of chronic pain, and intramuscular stimulation (IMS) is more advanced type of DDN. Because IMS needles are thin and have rounded tips, complications are not usually expected. However, we experienced a case of spinal subarachnoid hematoma occurring after an IMS, which was tentatively diagnosed as intracranial subarachnoid hemorrhage because of severe headache. Patient was successfully treated with surgery. Here, we report our case with a review of literatures.
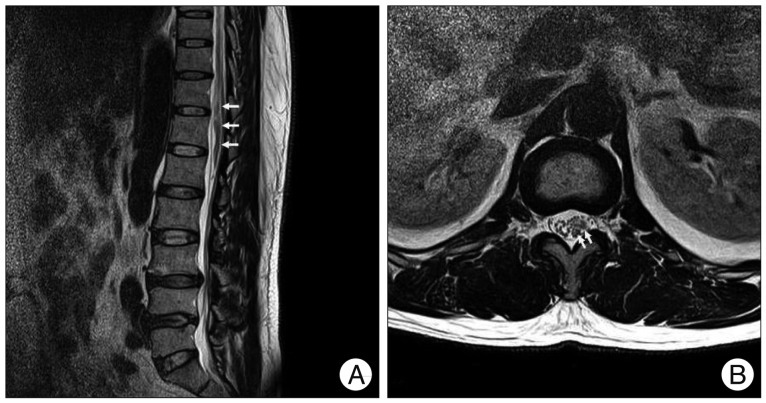
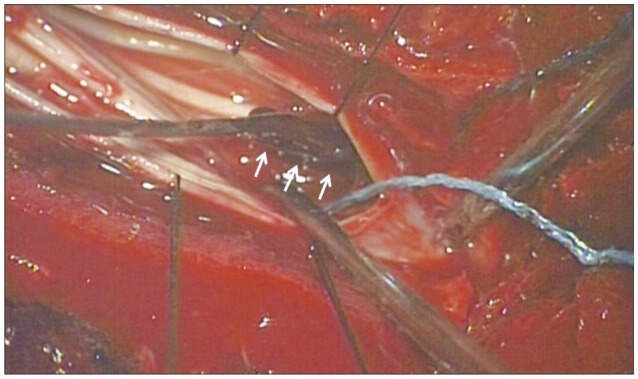
A 45-year-old man was hospitalized at a local clinic because of back pain. On the last day at the clinic, the patient underwent an IMS procedure and subsequently experienced severe headache and nausea. The patient underwent conservative management of the symptoms, but symptoms persisted. The patient was then referred to our hospital. Upon arrival, the patient had stable vital signs. A review of his medical history revealed a 5-year use of antihypertensive drugs, including daily aspirin (100 mg). Physical examination revealed neck stiffness without any other initial neurologic deficits. Clinical laboratory findings were all normal. Brain computed tomography (CT) was performed because the patient was suspected of having intracranial subarachnoid hemorrhage. But, this showed no abnormal findings. Because the patient continued to experience severe headache and nausea, he was admitted to the neurosurgical department for further evaluation and treatment. On the following day, the patient experienced severe back pain, decreased motor power of the lower extremities and constant headache. Based on these findings, the patient was suspected having intraspinal subarachnoid hematoma. The patient was interviewed in detail about the IMS procedure and its relatedness to the onset of headache. The patient stated that he had a history of severe radiating pain toward the lower extremities, while the IMS was directed toward the back. The severe headache and nausea occurred following the IMS procedure. We performed magnetic resonance imaging (MRI) of the thoracolumbar spine. But, the radiologic findings were suggestive of intraspinal subarachnoid hematoma (Fig. 1). The patient underwent an emergency exploratory laminectomy expecting to find a intradural hematoma. Then, we observed a solid hematoma compressing the cauda equina in the operative field (Fig. 2). The hematoma was completely evacuated. No evidence of tumor or vascular malformation was evident on histopathologic examination. Postoperatively, the patient's symptoms gradually improved. On postoperative week 3, the patient was discharged without any complications.
IMS was developed in 1973 and has proven to be an effective treatment for chronic pain, including myofascial pain syndrome7,11). Because the needle is very thin (diameter : 0.25-0.4 mm) and has a rounded tip, IMS has relatively few side effects5) and can be safely used for most patients, except those with local infection at the treatment site, uncontrolled diabetes mellitus, or increased bleeding tendency.
If clinicians encounter any patients who underwent IMS near the vertebral column and complained of extreme radiating pain and paresthesia followed by severe headache and nausea, as shown in the current case, they should consider the possibility of intraspinal subarachnoid hemorrhage due to spinal vessel injury.
Considering the present case retrospectively, the brain CT might have been negative despite the occurrence of severe headache and nausea because bleeding was minimal. If the chief complaint had been paraparesis rather than a severe headache, we would have initially suspected spinal hematoma8,10). According to Kreppel et al.4), who evaluated 613 cases of spinal hematoma (epidural, subdural, and subarachnoid), no etiological factor that explained bleeding was identified in nearly one-third of cases (29.7%). Following idiopathic spinal hematoma, cases related to anticoagulant therapy and vascular malformations represent the second and third most common categories. In patients with only subarachnoid hematoma, tumor hemorrhage is the most common cause of subarachnoid spinal hematoma, followed by vascular malformations, coagulopathy, puncture of the spinal space, and idiopathic factors. In a review by Domenicucci et al.2), 69 cases of spinal subarachnoid hematomas were assessed (excluding tumor or vascular anomalies), and the common causes were lumbar puncture for diagnostic or anesthesiological purposes (44.9%), coagulopathies (40.5%), and traumatic injuries (15.9%); these factors could be present singly or in various combinations. Knowles et al.3) investigated red blood cell counts in the cerebrospinal fluid (CSF) of patients undergoing routine spinal anesthesia. They found that the incidence of paresthesia was significantly associated with the increased RBC counts.
The cause and the underlying mechanism of spinal subarachnoid hematoma in the current case remain unclear. The most likely mechanism is that needling traumatized the fine radicular vessels parallel to nerve roots6,14). In general, the natural flow of CSF tends to dilute and wash away blood. This cannot easily lead to the formation of blood clots. However, excessive bleeding in the subarachnoid space; diminished CSF flow due to spondylo-arthrotic processes, arachnoiditis, disc herniation, or thickening of the ligamentum flavum; and coagulation defects may contribute to the formation of subarachnoid hematoma2).
In the current case, the patient complained of severe paresthesia during IMS, and subsequently suffered from headache and nausea. Therefore, our case indicates that the IMS procedure might be the cause of hematoma. It has been previously reported that aspirin induced the occurrence of spontaneous spinal hematoma. This implies that the role of aspirin in causing spinal hematoma cannot be ignored13). Clinicians should therefore perform a thorough review of patients' medical history of taking anticoagulants and antiplatelets and that of bleeding tendency before performing IMS1,9,12). In addition, they should also be equipped with a sufficient level of knowledge about the anatomy and exact practice is required. The timing of surgical decompression of the spinal cord and preoperative neurological status are both essential for the treatment outcomes4). In the current case, in which the motor weakness was not severe, the emergency decompression was performed after onset. This might explain why the patient's neurologic symptoms recovered fully without any complications.
This is the first reported case of spinal subarachnoid hematoma after IMS. In the event of negative brain CT findings but persistent meningeal irritations signs, including spinal anesthesia, myelography, diagnostic lumbar puncture, or IMS near paravertebral muscle, spinal MRI should be performed to determine the bleeding focus.
In conclusion, our case indicates that clinicians should consider the possibility that serious complications might also occur, although rare, in patients undergoing IMS.
References
1. Chee YL, Crawford JC, Watson HG, Greaves M. Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. British Committee for Standards in Haematology. Br J Haematol. 2008; 140:496–504. PMID: 18275427.

2. Domenicucci M, Ramieri A, Paolini S, Russo N, Occhiogrosso G, Di Biasi C, et al. Spinal subarachnoid hematomas : our experience and literature review. Acta Neurochir (Wien). 2005; 147:741–750. discussion 750. PMID: 15711890.

3. Knowles PR, Randall NP, Lockhart AS. Vascular trauma associated with routine spinal anaesthesia. Anaesthesia. 1999; 54:647–650. PMID: 10417455.

4. Kreppel D, Antoniadis G, Seeling W. Spinal hematoma : a literature survey with meta-analysis of 613 patients. Neurosurg Rev. 2003; 26:1–49. PMID: 12520314.

5. Lee YJ, Ahn K, Lee SC. The deep dry needling techniques, and interventional muscle & nerve stimulation (IMS) for the treatment of chronic pain. Korean J Pain. 2006; 19:1–7.

6. Liu WH, Lin JH, Lin JC, Ma HI. Severe intracranial and intraspinal subarachnoid hemorrhage after lumbar puncture : a rare case report. Am J Emerg Med. 2008; 26:633.e1–633.e3. PMID: 18534309.
7. Nam KH, Choi CH, Yang MS, Kang DW. Spinal epidural hematoma after pain control procedure. J Korean Neurosurg Soc. 2010; 48:281–284. PMID: 21082060.

8. Nam SG, Jeon IS, Heo HM, Hwang KH, Park W. Assessment of intramuscular stimulation in patients with myofascial pain syndrome using thermography. J Korean Pain Soc. 2003; 16:54–59.
9. Seet RC, Lim EC, Wilder-Smith EP, Ong BK. Spontaneous epidural haematoma presenting as cord compression in a patient receiving clopidogrel. Eur J Neurol. 2005; 12:811–812. PMID: 16190921.

10. Song JY, Chen YH, Hung KC, Chang TS. Traumatic subdural hematoma in the lumbar spine. Kaohsiung J Med Sci. 2011; 27:473–476. PMID: 21943822.

11. Srbely JZ, Dickey JP, Lee D, Lowerison M. Dry needle stimulation of myofascial trigger points evokes segmental anti-nociceptive effects. J Rehabil Med. 2010; 42:463–468. PMID: 20544158.

12. Sung JH, Hong JT, Son BC, Lee SW. Clopidogrel-induced spontaneous spinal epidural hematoma. J Korean Med Sci. 2007; 22:577–579. PMID: 17596676.

13. Weber J, Hoch A, Kilisek L, Spring A. [Spontaneous intraspinal epidural hematoma secondary to use of platelet aggregation inhibitors]. Dtsch Med Wochenschr. 2001; 126:876–878. PMID: 11569370.

14. Wood GG, Jacka MJ. Spinal hematoma following spinal anesthesia in a patient with spina bifida occulta. Anesthesiology. 1997; 87:983–984. PMID: 9357903.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download